HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Nevada Releases Medicaid Managed Care RFP: State Will Expand Managed Care Statewide Into Rural Areas

- Illinois D-SNP Procurement Attracts Six Bidders

- Michigan Releases In Lieu of Services Program Policy Guide for Medicaid Plans

- Nevada Releases Draft Section 1115 Reentry Services Demonstration

- Wisconsin Receives Federal Approval for BadgerCare Reform Demonstration Extension

- CMS Announces Additional State Participants in AHEAD Model

- Medicare Shared Savings ACOs Saved $2.1 Billion in 2023

- Orlando Health Finalizes Acquisition of FL-based Steward Health Hospitals

- More News Here

In Focus
Nevada Releases Medicaid Managed Care RFP: State Will Expand Managed Care Statewide Into Rural Areas
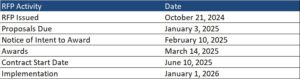
This week, our In Focus section highlights the State of Nevada’s October 21, 2024 request for proposals (RFP), which will expand Medicaid managed care to cover nearly all populations in all counties. The Department of Health and Human Services’ Division of Health Care Financing and Policy (DHCFP) estimates that the expansion statewide will cover 75,000 additional individuals who live in rural areas, including children, parents, and adults without children. The expansion to rural areas in all counties presents new opportunities and critical issues for managed care plans, ensuring that they meet the needs of rural populations effectively.
Background
In 2024, Nevada covers 788,000 Medicaid members, with risk-based capitated Medicaid managed care making up about 75 percent of the total Medicaid population. Managed care covers traditional Medicaid and expansion, the Children’s Health Insurance Program (CHIP) known as Nevada Check Up, and children who have aged out of foster care. Enrollment in an MCO is mandatory for these populations. Currently, Medicaid managed care is only offered in the urban Washoe and Clark counties, which include cities such as Reno and Las Vegas.
Nevada has four MCOs that were procured in 2021: Centene/SilverSummit HealthPlan, Elevance/Anthem, Molina, and UnitedHealthcare/Health Plan of Nevada. These MCOs serve approximately 588,000 beneficiaries in Urban Washoe and Urban Clark counties as of August 2024.
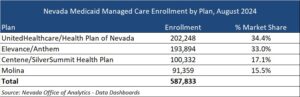
United and Elevance make up the majority of market share by enrollment, with 34.4 percent and 33 percent respectively.
Individuals who receive Medicaid through fee-for-service (FFS) are Medicaid-enrolled children in foster care, juvenile justice, and child welfare systems; individuals with disabilities; seniors; and individuals receiving services through one of the three 1915 home and community-based waiver programs. These individuals will continue to receive services through FFS.
RFP Highlights
The RFP describes the state’s three managed care service areas (SA): Urban Washoe, Urban Clark, and Rural. The Rural SA will include all other counties in Nevada in addition to the rural areas of Washoe and Clark counties.
MCOs must bid on all service areas. DHCFP anticipates selecting four plans. The two awarded vendors with the highest rural care score will operate in all three SAs. The remaining awarded vendors will operate in Urban Clark and Urban Washoe SAs. The state has the option to award a fifth contract to an MCO to operate in the Urban Clark SA only.
The RFP focuses on rural care and policies designed to improve outcomes and access to care, reduce burdens for providers to participate, and simplify administrative tasks for the state. MCOs will need to show their understanding of the unique challenges facing rural providers. They will describe their approach for provider outreach, contracting, and provider training strategies in rural areas, with a focus on primary care, maternal and child health, and behavioral health. Due to the geographic limitations, telehealth will also play a strong role. MCOs will need to address limitations such as access to internet and provide an approach to help members access telehealth. Additionally, MCOs will need to provide their experience in managing non-emergency medical transportation (NEMT) in rural areas and describe an approach for establishing and maintaining a network of transportation providers in these remote areas.
MCOs also will be required to offer at least one Silver and one Gold Qualified Health Plan (QHP) on Nevada Health Link Marketplace by the 2026 coverage year. The state expects this contractual requirement will help reduce churning and improve continuity of care for individuals and families who have a change in eligibility status.
MCOs must also contract with providers that use alternative payment methodologies (APMs), and plans will need to outline value-based purchasing (VBP) strategies within their proposals. APM contracting strategies must support priority areas such as addressing health-related social needs (HRSNs) and improving health equity, access, behavioral health, and maternal and child health outcomes. APM contracting strategies must include quality measures in the payment methodology and outline reporting and estimated financial details. Additionally, MCOs are required to develop a Population Health Program, so proposals must outline how it will leverage specific APMs to meet the program’s goals.
Evaluation
MCOs will require a minimum score of 945 points (out of 1,350 points) on the Technical Proposal to be eligible to win a contract. The Building Provider Networks and Access to Care technical questions is worth the most points, 450, while 300 points are available under the Rural Care and Service Area Expansion section. The table below provides a breakdown of the Technical Proposal Scoring.

The state assigns the highest number of points to the section addressing provider networks and access to care followed by the section addressing rural care and service area expansion.
Timeline
Key Considerations
HMA experts identified the key considerations for MCOs, partners to MCOs, providers who will furnish services to members, and other interested stakeholders.
- The Building Provider Networks and Access to Care Rural Care and Service Area Expansion sections together are worth 750 points, most of the minimum needed, and more than half of the total available points. This is a strong indicator of that MCOs need to demonstrate capacity and innovation to ensure access to members using multiple strategies. Ensuring a robust network of healthcare providers in rural areas is crucial. This includes recruiting and retaining providers who are willing to serve in these regions.
- In this RFP, DCHFP is evolving its value-based payment (VBP) initiatives and expectations for MCOs. The VBP strategies are intended to enhance care quality, improve patient outcomes, and ensure the sustainability of the Medicaid program. MCOs will need to design these models and successfully work with providers to implement the strategies and models.
- Both improving maternal and child health outcomes and addressing mental health and substance use disorders are priorities for the state. These can be more challenging in rural settings due to limited access to specialized care and will require rural specific solutions.
- Changing the Medicaid delivery system model in some rural areas may create the need for building awareness and understanding for the changes that come with this transition. MCOs should be prepared to effectively address the issues of equity and disparities that are present in in rural communities.
Connect with Us
HMA’s experts understand the Medicaid managed care environment and specific issues presented by rural areas. We work with clients to address the multilevel challenges for delivery of quality healthcare and social services to rural populations, and the workforce concerns they create. We identify and help plan for access issues such as lack of services, transportation difficulties, and socio-economic barriers. HMA knows the difficulties that often keep rural providers and organizations from achieving their full potential to serve and support their communities’ need and help Medicaid clients in rural areas in states around the country to solve these difficult problems.
Read more about the work we are engaged in with a range of healthcare industry leaders focused on rural and frontier areas.
HMA Roundup
Arkansas
Arkansas Delivers First Postpartum Medicaid Quarterly Update to the Legislature. The Arkansas Advocate reported on October 28, 2024, that the Arkansas Department of Human Services delivered the first postpartum Medicaid quarterly update to the Legislature, required by Act 161 of 2024 under the fiscal 2025 budget. The report showed that Arkansas had 4,234 postpartum Medicaid beneficiaries during the third quarter, of which 1,451 were not eligible for coverage 60 days postpartum. The state had 1,711 beneficiaries remain in the same eligibility category 60 days postpartum. Arkansas is the only state that has not adopted postpartum Medicaid expansion from 60 days to 12 months after birth.
Arkansas Opens Investigation Over CareSource PASSE Billing Practices. The Northwest Arkansas Democrat Gazette reported on October 27, 2024, that the Arkansas Department of Human Services has opened an investigation into expenses reported by CareSource, one of the state’s Provider-led Arkansas Shared Savings Entities (PASSEs) serving about 4,300 Medicaid recipients with complex mental health needs or intellectual or developmental disabilities. The investigation is focused on billing practices related to supportive living payments.
Georgia
Georgia Pathways to Coverage First-year Enrollment Falls Short of Expectations, Report Finds. The Georgia Budget and Policy Institute, a nonprofit policy advocacy organization, released on October 29, 2024, a report outlining trends seen in the first year of the state’s Pathways to Coverage program, which expands Medicaid coverage to non-pregnant, non-disabled, low-income individuals who meet eligibility and report certain work requirements. The report found that enrollment in the program was lower than expected due to a complicated enrollment process and restrictive eligibility criteria; more than 40 percent of Georgia counties had fewer than 10 enrollees despite the high uninsured rate statewide. The report also found that on average, each enrollee cost more than $13,000 in combined federal and state funds from time of approval until the end of the first year, and that the largest portion of total program costs came from upgrades to Georgia’s online eligibility and enrollment system. The program is set to expire September 2025.
Illinois
Illinois D-SNP Procurement Attracts Six Bidders. The Illinois Department of Healthcare and Family Services (HFS) confirmed that six plans have submitted proposals for the state’s Dual Eligible Special Needs Plan (D-SNP) reprocurement: Aetna Better Health Premier Plan, Centene/Meridian Health Plan, Molina Healthcare, Humana Health Plan, UnitedHealthcare, and Health Care Service Corporation. Contracts will begin January 1, 2026, and run through December 31, 2029, with extensions up to five years and six months.
Illinois Certified Community Behavioral Health Clinics Offer Mental Health, Substance Use Treatment Services. The Illinois Department of Healthcare and Family Services (HFS) announced on October 24, 2024, that 19 Certified Community Behavioral Health Clinics (CCBHCs) across the state are now offering enhanced behavioral health services, including mental health care and substance use treatment services. The new model of care is part of the four-year federal CCBHC Medicaid Demonstration Program, designed to expand and improve access to coordinated services.
Michigan
Michigan Releases In Lieu of Services Program Policy Guide for Medicaid Plans. The Michigan Department of Health and Human Services (MDHHS) released in September 2024, an in lieu of services (ILOS) policy guide for Medicaid Health Plans (MHPs) participating in the Comprehensive Health Care Program to provide medically appropriate and cost-effective substitutes for covered services or settings under the Michigan Medicaid State Plan. Pending federal approval, MHPs will be able offer one or more ILOS including medically tailored home delivered meals; healthy home delivered meals; healthy food packs; and produce prescriptions. The state will designate a set of federally approved ILOS that plans may offer beginning January 2025.
Nevada
Nevada Releases Draft Section 1115 Reentry Services Demonstration. The Nevada Department of Health and Human Services Division of Health Care Financing and Policy (DHCFP) reported on October 24, 2024, a draft section 1115 justice-involved reentry demonstration application to provide services to Medicaid and Children’s Health Insurance Plan eligible justice-involved youth and adults 90 days prior to their release. Public comments will be accepted through November 24.
New York
New York Senator Introduces Bill to Allow Grants for Medicaid Enrollees During, After Pregnancy. Crain’s New York reported on October 25, 2024, that New York State Senator Andrew Gounardes introduced a bill that would allow one-time grants of $1,800 for Medicaid enrollees during and after a pregnancy, aiming to help families cover the costs of food, rent, or clothing. The New York Healthy Birth Grant Program would require federal approval through a Section 1115 demonstration. It is estimated it would cost New York $177 million to provide grants to the approximately 98,000 babies born each year who are eligible for Medicaid.
New York Plan Faces Lawsuit Over Provider Network. Fierce Healthcare reported on October 23, 2024, that Anthem Blue Cross Blue Shield of New York is facing a class-action lawsuit over its directory of mental health providers in the Federal Employees Health Benefits program. The lawsuit alleges that the plan’s provider directory is a “ghost network” containing inaccurate information, duplicate entries of the same clinicians, and names of clinicians who do not accept BCBS insurance, which is forcing patients to seek out-of-network care. The lawsuit notes that ghost networks violate the No Surprises Act, Mental Health Parity and Addiction Equity Act, and New York insurance law.
Oregon
Oregon Paid $445 Million for Duplicate Medicaid Enrollees, Audit Finds. The Statesman Journal reported on October 28, 2024, that Oregon paid $445 million toward Medicaid beneficiaries enrolled in more than one state between 2019 and 2022, according to an audit conducted by the Oregon Secretary of State, the Office of the Washington State Auditor, and the U.S. Department of Health and Human Services Office of the Inspector General. The report outlined recommendations to prevent improper payments, including a pilot program in Oregon and Washington to address risks with concurrent enrollment, strengthened federal help to identify concurrent enrollment earlier, and improving the Public Assistance Reporting Information System (PARIS), a data matching service administered in Oregon by the Office of Payment Accuracy and Recovery that checks if recipients of public assistance receive duplicate benefits.
Tennessee
Tennessee to Use $100 Million in Medicaid Shared Savings for Hurricane Helene Relief. Tennessee Lookout reported on October 28, 2024, that Governor Bill Lee has directed $100 million from the TennCare shared savings fund toward Helene Emergency Assistance Loans (HEAL) to help 13 counties with disaster relief efforts in the aftermath of Hurricane Helene. Tennessee’s shared savings fund allows the state to spend certain unused Medicaid dollars on non-Medicaid programs, as long as the spending benefits the health and well-being of Tennesseans. HEAL loans are meant to cover costs of debris removal and repairing badly damaged utilities as the counties wait for FEMA funds. According to Governor Lee, certain TennCare programs may be put on hold as counties repay the HEAL loans.
Texas
Texas Cuts School Medicaid Budget by $607 Million. The Texas Tribune reported on October 28, 2024, that Texas school districts are set to receive around $607 million less per year in federal funding for the School Health and Related Services (SHARS) program. SHARS funding allows school districts to provide special education services such as counseling, nursing, therapy, and transportation services for Medicaid-eligible children. The decreased budget is due to stricter limitations that the Texas Health and Human Services Commission imposed on the services for which school districts can request federal reimbursement. Some school districts are formally appealing the cuts, while others, especially in rural areas, are exiting the program.
Wisconsin
Wisconsin Receives Federal Approval for BadgerCare Reform Demonstration Extension. The Centers for Medicare & Medicaid Services (CMS) announced on October 29, 2024, that it has approved a five-year extension of Wisconsin’s Section 1115 Wisconsin BadgerCare Reform demonstration, through December 31, 2029. The extension does not include any substantive changes but renews the state’s authority to continue providing services including substance use disorder (SUD) benefits in institutions for mental diseases (IMDs) and coverage to out-of-state former foster care youth up to 26 years of age who were enrolled in Medicaid in another state.
National
CMS Announces Additional State Participants in AHEAD Model. The Centers for Medicare & Medicaid Services (CMS) announced on October 28, 2024, that Rhode Island and a subsection of New York, including Bronx, Kings, Queens, Richmond, and Westchester counties, have been chosen to participate in Cohort 3 of the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model, beginning in January 2025. The AHEAD Model aims to control healthcare cost growth, improve population health with primary care investments, and advance health equity by addressing disparities. States have the opportunity to receive up to $12 million from CMS during the first five to six years to support implementation. Cohort 3’s two-year pre-implementation period begins in January, and the full program will run from January 2027 through December 2034. Connecticut, Hawaii, Maryland, and Vermont were chosen to participate in Cohorts 1 and 2 of the model beginning in July.
Medicare Shared Savings ACOs Saved $2.1 Billion in 2023. The Centers for Medicare & Medicaid Services (CMS) announced on October 29, 2024, that Accountable Care Organizations (ACOs) in the Medicare shared savings program had net savings of $2.1 billion in 2023, a 16.7 percent increase in savings from the previous year. Providers participating in ACOs earned a total of $3.1 billion in performance payments, up from $2.5 billion in 2022. ACO participation increased, with 480 ACOs in the shared savings program as of January 2024, compared to 456 at the beginning of 2023.
Lawmakers Introduce Bipartisan Bill Seeking to Block Medicare Provider Pay Cuts. Modern Healthcare reported on October 29, 2024, that a bipartisan group of lawmakers, led by Representatives Greg Murphy (R-NC) and Jimmy Panetta (D-CA), has introduced a bill seeking to block a proposed Centers for Medicare & Medicaid Services (CMS) rule that would cut Medicare physicians’ reimbursement by 2.9 percent in 2025. The Medicare Patient Access and Practice Stabilization Act would eliminate the pay cut and give physicians a small pay increase instead to account for inflation. CMS has until November 1 to publish its final rule.
Improper Use of Health Risk Assessments Resulted in Inaccurate MA Payments, HHS OIG Finds. The U.S. Department of Health and Human Services Office of the Inspector General (HHS OIG) released in October 2024, a report examining risk-adjusted payments to Medicare Advantage (MA) plans, finding that improper use of health risk assessments (HRAs) continues to cause overpayments. The report found that in-home HRAs generated two-thirds of the $7.5 billion in risk-adjusted payments in 2023, but that encounter data with MA enrollees showed a lack of follow-up visits for serious conditions diagnosed through these assessments, raising concerns that either the diagnoses were inaccurate or that patients were not receiving needed care. HHS OIG recommends that the Centers for Medicare & Medicaid Services should impose more restrictions on using diagnoses resulting from in-home HRAs when calculating risk-adjusted payments, conduct audits to validate diagnoses, and determine whether certain diagnoses may be more susceptible to misuse on in-home HRAs.
CMS Updates Marketplace Eligibility, Website Ahead of 2025 Plan Year Open Enrollment. Health Payer Specialist reported on October 28, 2024, that the Centers for Medicare & Medicaid Services (CMS) has announced eligibility and plan changes for the federal health insurance Marketplace for the 2025 plan year, including plans focusing on individuals with chronic conditions and high-cost healthcare issues and subsidized coverage for Deferred Action for Childhood recipients. CMS also redesigned the healthcare.gov website to provide greater clarity for important deadlines and actions enrollees must take to ensure their coverage is in place. Plans participating in the state or federal exchanges must ensure that at least 90 percent of their enrollees can receive an appointment for behavioral health services within 10 business days; primary care appointments within 15 business days and non-urgent specialty care appointments within 30 business days.
Half of States are Expanding Coverage or Reducing Barriers for Medicaid, CHIP-Covered Children, KFF Finds. KFF released on October 29, 2024, a policy watch highlighting how states have changed coverage for Medicaid and Children’s Health Insurance Plan (CHIP)-covered children since the start of the pandemic in 2020. The report found that half of all states have implemented or are planning to implement policies to either expand eligibility or reduce barriers for Medicaid and CHIP enrollment. Some states have expanded eligibility by increasing the CHIP/Medicaid income eligibility threshold and/or extending coverage to undocumented children. Many states have also worked to reduce enrollment and coverage barriers by seeking approval for multi-year continuous eligibility, eliminating or reducing premiums, and/or transitioning enrollees in a state-funded CHIP program to a CHIP-funded Medicaid expansion program.
Most Americans Support HHS Rule Strengthening Behavioral Healthcare Parity, Survey Finds. The Hill reported on October 24, 2024, that 79 percent of Americans support the recent U.S. Department of Health and Human Services (HHS) rule that strengthens the Mental Health Parity and Addiction Equity Act and requires insurance plans to cover behavioral healthcare services, according to a West Health-Gallup Healthcare survey of 3,660 U.S. adults. Half of respondents slightly trust or do not trust that all insurance companies will provide adequate access even with the rule, however. Additionally, 73 percent of respondents think the federal government has not done enough to ensure access to affordable mental healthcare.
Providers Advocate for Higher Buprenorphine Doses for Medicaid-covered SUD Treatment. Roll Call reported on October 24, 2024, that doctors treating substance use disorder (SUD) in Medicaid-covered patients are advocating for states to start covering higher doses of buprenorphine. The American Medical Association House of Delegates adopted a resolution earlier this year supporting doctors’ ability to prescribe buprenorphine doses higher than U.S. Food and Drug Administration guidelines, and the group advocates for federal agencies, health plans, and manufacturers to reassess dosing policies and labels. States including Washington and the District of Columbia have increased limits for buprenorphine doses. Buprenorphine doses higher than 24 milligrams had a lower risk of emergency department visits or inpatient visits related to behavioral health, according to a JAMA Network study.
Industry News
Orlando Health Finalizes Acquisition of Florida-based Steward Health Hospitals. Modern Healthcare reported on October 24, 2024, that Orlando Health has finalized its $439 million acquisition of three Florida-based hospitals previously owned by Steward Health Care. The deal includes Melbourne Regional Medical Center, Rockledge Regional Medical Center, and Sebastian River Medical Center.
RFP Calendar

HMA News & Events
HMA Webinars:
The Housing Imperative for Persons with Disabilities to Advance Independent Living and Recovery. Thursday, October 31, 2024, 12:00 PM ET. This webinar will elevate the importance of expanding affordable and accessible housing for persons with disabilities. Persons with disabilities face enormous challenges in finding affordable and accessible housing for two main reasons. First, they struggle to afford housing. Second, it’s not easy to find accessible housing. Join us as experts share their key insights into the state of affordable and accessible housing for persons with disabilities and contributions to expanding the housing supply. Register Here
Medications for Opioid Use Disorder (MOUD) in Criminal Justice Settings: Developing Partnerships between Correctional Professionals and Community-based Providers. Thursday, October 31, 2024, 02:00 PM ET. Reentry into the community from jail or prison can be a critical time, particularly for people experiencing substance use disorders. However, many jails and prisons lack the necessary connections and collaboration with local providers to support continuity of care upon release. This webinar will explore the critical role of community partnerships in supporting individuals receiving medications for opioid use disorder (MOUD) within criminal justice settings. Attendees will gain insight into how collaboration between correctional facilities, healthcare providers, and community organizations can enhance continuity of care, reduce recidivism, and support successful reintegration. Register Here
2024 Political Checkpoint. Tuesday, November 12, 2024, 12:00 PM ET. In the 2024 Political Checkpoint webinar hosted by Leavitt Partners, an HMA company, we will explore up-to-the-minute insights on the election results, discussing both confirmed outcomes and remaining uncertainties, along with the mandate for change that has emerged. Our expert panelists will provide an overview of what to expect from Congress and the Administration, focusing on key legislative priorities and executive actions, and share their predictions for what to watch over the first 100 days. Register Here
Mastering Star Performance: Strategies from the HMA Stars Accelerator Program. Wednesday, November 13, 2024, 12:00 PM ET. In this webinar, you’ll learn the essential methods and practices to enhance Star Ratings. HMA has developed our Stars Accelerator Solution to help plans improve their operations and attain higher Star Ratings. We’ll explore how to leverage data analytics to effectively track current star performance and identify areas for improvement. Additionally, we’ll dive into stratification techniques that allow for targeted focus on key measure opportunities throughout the year to ensure optimal results. HMA has also developed a playbook that captures the HMA Stars Accelerator Solution with proven strategies for Stars improvement based on our diverse and extensive expertise in managed care plan (MCP) operations, MCP strategy, performance improvement, actuarial science, data analytics, risk adjustment, and federal and state policy. Register Here
The Future of Medicare Advantage: How the Election Results Impact the Program. Tuesday, November 19, 2024, 12:00 PM ET. More than 50 percent of Medicare enrollees now choose Medicare Advantage (MA) as their preferred coverage option. This increased growth has brought with it increase scrutiny, with elected officials, regulators, think tanks, and news organizations all raising questions about the current makeup of the program. With MA reform potentially on the table in 2025, come learn about how the election results impact what policy changes could be considered in the coming year. Register Here
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
- Updated State Medicaid Agency Contracts (SMACs) Inventory
- Updated District of Columbia State Overview
- Updated Maryland State Overview
- HMA Federal Health Policy Quick Takes
Medicaid Data
Medicaid Enrollment:
- California Medicaid Managed Care Enrollment is Up 3.9%, Jun-24 Data
- Iowa Medicaid Managed Care Enrollment is Down 2.6%, Jun-24 Data
- Louisiana Medicaid Managed Care Enrollment is Down 10.7%, Jun-24 Data
- New Mexico Medicaid Managed Care Enrollment is Down 0.9%, Jun-24 Data
- New York Medicaid Managed Care Enrollment is Down 3.7%, Mar-24 Data
- New York CHIP Managed Care Enrollment is Up 10.4%, Mar-24 Data
- North Carolina Medicaid Managed Care Enrollment is Up 5.8%, May-24 Data
- Oklahoma Medicaid Enrollment is Down 4.9%, Jun-24 Data
- Oregon Medicaid Managed Care Enrollment is Down 1.2%, Apr-24 Data
- South Carolina Medicaid Managed Care Enrollment is Down 7.4%, May-24 Data
- South Carolina Dual Demo Enrollment is Down 13.6%, May-24 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Illinois Dual Eligible Special Needs Plan (D-SNP) RFP, Bidders List, and Related Documents, Oct-24
- Michigan Coordinated Health HIDE SNP RFP, Proposals, Awards, Evaluations, and Related Documents, 2024
- Missouri Medicare Advantage D-SNP Model Contract, 2025
- Oklahoma SoonerSelect Children’s Specialty Plan RFP and Contract, 2022-23
- Pennsylvania Medicare Advantage D-SNP Model Contract, 2025
- Rhode Island Medicare Advantage D-SNP Contracts, 2025
Medicaid Program Reports, Data, and Updates:
- Arkansas Monthly Enrollment and Expenditures Report, CY 2024
- Maryland Prescription Drug Affordability Board Meeting Materials, 2021-24
- Michigan Comprehensive Health Care Program ILOS Policy Guide, Sep-24
- Nevada Section 1115 Reentry Demonstration Waiver Documents, Oct-24
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Sep-24
- Pennsylvania MLTSS Subcommittee Meeting Materials, Oct-24
- Wisconsin BadgerCare Reform 1115 Waiver Documents, 2017-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
