HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Improving Culturally Relevant Care for AI/AN Populations: Insights into Federal Approval of Medicaid-Covered Traditional Healing

- Colorado Proposed Fiscal 2026 Budget Includes Medicaid Provider Rate Cuts

- Florida Releases Children’s Medical Services Program ITN

- Florida Submits Amendment Request for 1115 Managed Medical Assistance Demonstration

- Illinois Releases EVV System Vendor RFP

- Nebraska Names Drew Gonshorowski as Medicaid Director

- Ohio Receives Protest Over Next Generation MyCare Contract Awards

- Texas to Begin Transition from Dual Demonstration to Integrated D-SNP January 2026

- CMS Approves Five Medicaid Demonstrations to Provide Continuous Enrollment for Children

- CMS Issues Guidance to State Medicaid Directors on Medicaid Coverage of SUD, Managed Care Medical Loss Ratio Provisions

- President-elect Donald Trump to Nominate Dr. Oz to Head CMS

- Eli Lily Files Lawsuit Over Use of 340B Drug Pricing Program Rebates

- More News Here

In Focus
Improving Culturally Relevant Care for AI/AN Populations: Insights into Federal Approval of Medicaid-Covered Traditional Healing
This week, our In Focus section reviews new state initiatives to cover traditional healing services through Medicaid for American Indian/Alaska Native (AI/AN) individuals and communities.
Overview
In October 2024, The Centers for Medicare & Medicaid Services (CMS) approved Medicaid Section 1115 demonstration amendments for Arizona, California, New Mexico, and Oregon, allowing Medicaid and Children’s Health Insurance Program (CHIP) coverage of traditional healing services delivered at or through Indian Health Service facilities, Tribal facilities, and urban Indian organizations (I/T/U facilities).
This demonstration approval enables state Medicaid agencies to acknowledge traditional healthcare practices as important components of the wellness continuum of care for Native American populations. Medicaid funding will help strengthen and expand access to these services and support integration of these services into primary care, substance use disorder (SUD) treatment, and other behavioral health care in a way that I/T/U providers have designed and developed to meet the unique needs of their community.
Demonstrations for Arizona and Oregon are approved through September 30, 2027, New Mexico’s demonstration is authorized through December 31, 2029, and California’s through December 31, 2026.
Traditional Health Services: Providing Culturally Relevant Care
AI/AN populations generally experience worse health disparities compared with non-AI/AN populations, particularly in terms of obesity, diabetes, tobacco addiction, and cancer. AI/AN populations also face higher rates of mental health disorders, SUDs, and suicide.
Using Transformed Medicaid Statistical Information System (T-MSIS) claims and demographics data, Health Management Associates, Inc. (HMA), staff assessed the incidence of specific chronic diseases in the Native American and non-Native American population in the four states approved to cover traditional healing services through their Medicaid program. For example, in these states, the prevalence of diabetes in AI/AN populations ranged from 27 percent to 87 percent higher than among non-AI/AN groups. Figure 1 shows the percentage of three chronic conditions among these groups in the four states.
Figure 1. Percentage of AI/AN vs. Non-AI/AN Medicaid Beneficiaries Living with Chronic Conditions in AZ, CA, NM, and OR (2022)
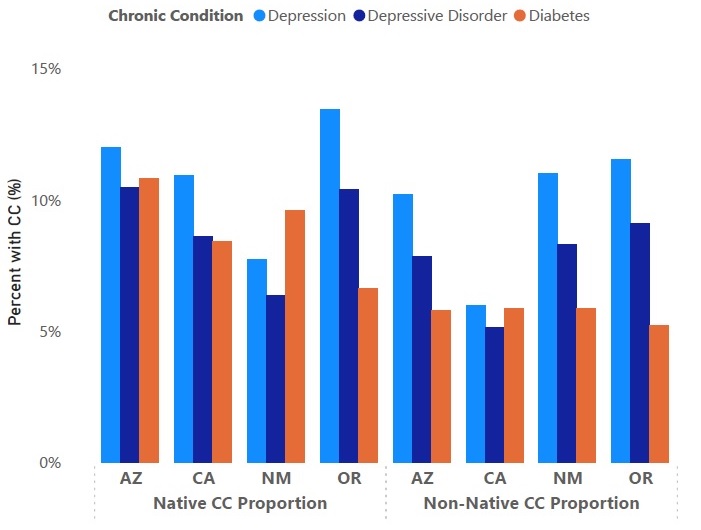
The demonstration approval is expected to improve access to culturally appropriate healthcare to address these disparities in chronic conditions for Tribal communities. Traditional healthcare practices vary widely across the 574 federally recognized Tribes in the United States, and many see traditional healthcare practices as a fundamental element of well-being that can help patients with specific physical and behavioral health conditions. For example, commonly offered traditional practices in Native American communities include talking circles, sweat lodges, and smudging. Studies show that incorporating traditional healthcare practices may improve mental health symptoms, outcomes, and quality of life, including among individuals with SUD.
Considerations for Key Partners
AZ, CA, NM, and OR are the first states to receive federal approval and will lay the groundwork for integrating time-honored healing practices into their Medicaid systems. They also could serve as a model for other states that choose to pursue this demonstration. I/T/Us were integral to shaping the demonstration design and are poised to continue shaping the program details and implementation of traditional approaches to care into their Medicaid systems.
HMA experts identified some key considerations for partners, such as states and Medicaid managed care organizations (MCOs), to follow as these services are incorporated into Medicaid:
- Collaborate with I/T/U facilities and communities. Traditional healing practices are sacred and ceremonial, so flexibility will be essential in determining how Medicaid funding can be best allocated to support providers who offer traditional practices. Communities will be critical in helping identify the specific traditional healing practices that are needed.
- Support operational changes needed in I/T/U facilities. Compliant and efficient billing practices will be essential to the success of the demonstrations. States can support I/T/U facilities to develop necessary trainings, workflows, and administrative processes. For example, the provider qualification criteria and implementation is central to meeting federal compliance and reporting requirements. Facilities also will need to meet Medicaid billing requirements to collect 100 percent of the federal medical assistance percentage (FMAP).
- Partner with I/T/U facilities. To facilitate proper care coordination, states, health plans, and non-I/T/U providers should partner with I/T/U facilities to ensure patients experience the best health outcomes.
Connect With Us
HMA has learned the value and importance of working with Native American and Alaska Native populations and respecting their unique approaches to improving healthcare. HMA has expertise on healthcare issues that uniquely affect AI/AN populations and is experienced in addressing these challenges through AI/AN leadership and engagement that is culturally sensitive and respectful. Our experience working directly with Tribes encompasses extensive and applicable knowledge of healthcare operations in rural and urban settings to support infrastructure needs, including data management, IT, staffing, policies and procedures, training, and eligibility and enrollment processes.
Contact Rebecca Kellenberg to learn more about HMA’s work to support Native American and Alaska Native communities.
HMA Roundup
Arkansas
Arkansas Officials Consider Replacement for ARHOME Demonstration. KARK reported on November 14, 2024, that Arkansas Senator Ben Gilmore (R-Crossett) inquired with Department of Human Services Secretary Kristi Putnam about pursuing a replacement to its Section 1115 AR Health and Opportunity for Me (ARHOME) demonstration during a budget hearing. The demonstration, which is set to expire December 31, 2026, is the state’s Medicaid expansion program that uses Medicaid funding to purchase coverage from qualified health plans offered on the Arkansas Health Insurance Marketplace.
Colorado
Colorado Proposed Fiscal 2026 Budget Includes Medicaid Provider Rate Cuts. The Denver Post reported on November 13, 2024, that Colorado Governor Jared Polis’ proposed $14.8 billion budget for the 2025-2026 fiscal year outlines significant cuts to help balance a $635 million budget deficit, including a proposed cut to Medicaid provider rates. The deficit is largely credited to high Medicaid costs and utilization, as well as alleviating inflation. Lawmakers raised concerns over the proposed Medicaid cuts, arguing that cutting provider rates would negatively impact the system.
Florida
Florida Releases Children’s Medical Services Program ITN. The Florida Department of Health released on November 14, 2024, an invitation to negotiate (ITN) for its Statewide Medicaid Managed Care (SMMC) Program and Children’s Health Insurance Program (CHIP) services, covering about 88,000 children. The Department intends to make a single statewide award. Proposals are due December 23, 2024, and awards are anticipated on March 21, 2025. The contract term will begin the date of contract execution through December 31, 2030, with no renewal options. The current incumbent is Sunshine Health.
Respondents must offer innovative and evidence-based approaches in meeting goals under the Medicaid program including improving mental health; promoting preventative health; enhancing care coordination; and utilizing a full array of services in the home to avoid institutional care. During the negotiation process, respondents may be provided an opportunity to recommend value added services, which are additional services provided that include new and innovative technologies relating to the telecommunication services sought under this solicitation.
Florida Submits Amendment Request for 1115 Managed Medical Assistance Demonstration. The Centers for Medicare & Medicaid Services (CMS) announced on November 14, 2024, that Florida submitted an amendment to its section 1115 Florida Managed Medical Assistance (MMA) demonstration requesting to expand the Behavioral Health and Supportive Housing Assistance Pilot to two additional regions; provide voluntary MMA enrolled populations a choice of managed care plans and auto-assignment; transfer coverage of behavior analysis services to managed care; transfer coverage of non-emergency dental services to dental managed care plans; and update the special terms and conditions to reflect that specialty plans are now specialty products incorporated into managed care plans rather than being allowed to be standalone plans.
Illinois
Illinois Releases EVV System Vendor RFP. The Illinois Department of Human Services (DHS) released on November 18, 2024, a request for proposals (RFP) seeking a vendor to provide integration, training, maintenance, and operational services for a new Electronic Timekeeping and Visit Verification (EVV) system for Medicaid-covered home and community-based services (HCBS). DHS will be replacing its current EVV system. The new system will have technical and functional capabilities to verify at-home visits and allow for programmatic and cost efficiencies, HCBS program growth, future innovations, and increased fraud prevention and internal controls. Proposals are due January 8, 2025. DHS will announce awards in February 2025, and anticipates the contracts will start March 2025.
Indiana
Indiana Faces Class Action Lawsuit Over Medicaid HCBS Waiver Waitlists. The Indianapolis Star reported on November 14, 2024, that five plaintiffs filed a class action lawsuit against the Indiana Family and Social Services Administration (FSSA) in October over the waitlists for the Pathways for Aging and Health and Wellness waivers, which were formerly combined as the Aged and Disabled waiver. The lawsuit represents plaintiffs specifically on the Pathways waitlist, and claims that FSSA’s choice to implement the waitlists violates the Medicaid Act, the Rehabilitation Act, and the Americans with Disabilities Act. The lawsuit seeks an injunction to block the waitlists, which housed more than 13,000 people in October 2024. FSSA is pursuing alternative funding to help waitlisted people, seeking federal approval from the Centers for Medicare & Medicaid Services to effectively open up more waiver slots, and meeting with providers to help smooth out the waitlist process.
Louisiana
Louisiana to Release Dental Benefit Program Manager RFP. The Louisiana Department of Health Bureau of Health Services Financing announced in November 2024, that it will be releasing a request for proposals (RFP) to secure two dental benefit program managers (DBPM) for new contracts beginning January 1, 2026. The DBPMs will help the agency achieve a variety of goals, including improving oral health outcomes and coordination of care, increasing dental care quality, improving access to specialty dental services, and increasing outreach and education to promote dental health for 1.5 million Medicaid and Children’s Health Insurance Plan (CHIP) beneficiaries. Incumbents are DentaQuest and MCNA. Feedback will be accepted through November 22.
Michigan
Michigan Announces Grant Funding Opportunity, Resource Enhancements to Improve SUD Services. The Michigan Department of Health and Human Services announced on November 20, 2024, that it has launched a new tool that will identify licensed substance use disorder (SUD) treatment and recovery locations through a geographic search. The state has transitioned Opioid Health Homes to SUD Health Homes as a statewide benefit and added the diagnoses of Alcohol Use Disorder and Stimulant Use Disorder to broaden service eligibility. Additionally, Michigan issued a competitive grant funding opportunity worth $1.3 million for organizations to develop Quick Response Teams to provide follow-up and outreach to survivors of non-fatal opioid overdoses. Applications are due January 7.
Michigan House Passes Bill to Remove Medicaid Expansion Work Requirements. Michigan Advance reported on November 18, 2024, that the Michigan House passed a bill to permanently repeal work requirements for the state’s Healthy Michigan Medicaid expansion program. Although work requirements became inactive following a 2020 federal court ruling, lawmakers fear incoming federal officials could revisit this policy. The bill now moves to the state Senate for further consideration.
Nebraska
Nebraska Names Drew Gonshorowski as Medicaid Director. Nebraska Examiner reported on November 19, 2024, that Nebraska Governor Jim Pillen has appointed Drew Gonshorowski as director of Medicaid and Long-Term Care in the state Department of Health and Human Services. Gonshorowski previously served as a policy analyst, most recently at the Paragon Health Institute and the Heritage Foundation prior to that.
New York
New York Officials Forecast Medicaid Spending to Exceed Global Cap by $2.2 Billion in FY 2026. News10 ABC reported on November 18, 2024, that New York’s Medicaid budget is projected to exceed the global spending cap allowance by $2.2 billion and reach $35 billion in state funding by 2026, according a report presented by Assembly Ways and Means Committee and Senate Finance Committee state officials at New York’s Fiscal Year (FY) 2026 Quick Start Budget Meeting. The projected increase is due to higher Medicaid enrollment, higher utilization and costs forecasts, and delayed federal approvals. Governor Kathy Hochul will propose a FY 2026 budget by January 21, 2025.
New York Audit Identifies $14 Billion in Improper Medicaid Home Care Services Claims. CNY Central reported on November 14, 2024, that New York paid more than $14 billion on Medicaid home care services with no matching electronic visit verification (EVV) record between January 2021 and March 2023, according to an audit by New York Comptroller Thomas DiNapoli. In 2021, the state implemented a Medicaid processing system to prevent payments for certain claims when there is no matching EVV record, although auditors found this system was not turned on. State officials plan on implementing a program to increase compliance, and the comptroller’s audit made 14 recommendations for improving the verification system.
Ohio
Ohio Receives Protest Over Next Generation MyCare Contract Awards. Health Payer Specialist reported on November 15, 2024, that CVS/Aetna Better Health of Ohio has filed a protest over Ohio’s Next Generation MyCare dual special needs plan (D-SNP) contract awards after the incumbent plan did not receive a contract. Ohio awarded contracts to incumbents Centene/Buckeye Health Plan, CareSource, Molina Healthcare, and non-incumbent Anthem Blue Cross and Blue Shield in November. Incumbent UnitedHealthcare also did not receive an award.
Rhode Island
Rhode Island Faces Class Action Lawsuit Over Medicaid Mental Health Care Denials to Children. The Public’s Radio reported on November 13, 2024, that a group of advocacy organizations filed a class action lawsuit against Rhode Island for denying Medicaid-eligible children access to mental health care. The lawsuit, filed in U.S. District Court by the American Civil Liberties Union of Rhode Island and advocacy groups Disability Rights Rhode Island and New York-based Children’s Rights, claims the state is in violation of the Medicaid Act, the Americans with Disabilities Act, and the Rehabilitation Act.
Tennessee
Tennessee Medicaid Director Seeks $975 Million Increase for TennCare Budget. Tennessee Lookout reported on November 18, 2024, that TennCare Director Stephen Smith has proposed $975 million in additional funding to increase the state’s Medicaid budget to $18.6 billion. The request stems from rising medical costs, including an estimated $165 million in price increases for medical care and $41 million for the price of new drugs to treat diabetes, heart disease, and obesity.
Texas
Texas to Begin Transition from Dual Demonstration to Integrated D-SNP January 2026. The Texas Health and Human Services Commission (HHSC) confirmed on November 5, 2024, that it will transition from Dual Demonstration Medicare-Medicaid Plans (MMPs) to integrated Dual Eligible Special Needs Plans (D-SNPs) for fully dual eligible individuals on January 1, 2026. HHSC will halt passive enrollment for certain MMPs serving demonstration counties in July 2025, but D-SNPs in demonstration counties that are not affiliated with MMPs operating in the integrated D-SNP model and those not in demonstration counties may continue enrolling and serving full and partial dual eligible people. Pending compliance with the Centers for Medicare & Medicaid Services (CMS) regulations, HHSC will extend the integrated D-SNP model for full duals to the remaining D-SNPs that have affiliated STAR+PLUS Medicaid managed care organizations (MCOs) in demonstration counties on January 1, 2027. At that time, HHSC will also pause new member enrollment in coordination-only D-SNPs in demonstration counties that are not affiliated with STAR+PLUS MCOs. HHSC will analyze data from the integrated D-SNP model to make decisions about expanding the model beyond demonstration counties.
Wisconsin
Wisconsin Releases RFA to Assist Pregnant, Postpartum Individuals with Medicaid Renewals, Applications. The Wisconsin Department of Health Services (DHS) Division of Public Health (DPH) released on November 13, 2024, a request for applications (RFA) for funds to support statewide and local organizations participating in the Maternal Medicaid Enrollment Project, which aims to reduce maternal morbidity and mortality. The project helps ensure pregnant and postpartum people are able to enroll in and renew Medicaid coverage so they have continuous access to care. DHS will award up to four organizations between $25,000 and $50,000. Applications are due December 30, 2024.
National
CMS Approves Five Medicaid Demonstrations to Provide Continuous Enrollment for Children. The Centers for Medicare & Medicaid Services (CMS) announced on November 14, 2024, that Colorado, Hawaii, Minnesota, New York, and Pennsylvania received federal approval for section 1115 demonstration amendments to provide multi-year continuous eligibility for children beyond the minimum 12 months required by law. The amendments will allow continuous eligibility for children up to three years of age in Colorado and up to six years of age in Hawaii, Minnesota, New York, and Pennsylvania. These amendments also authorize Colorado and Pennsylvania to provide 12 months of continuous eligibility for individuals aged 19 through 64 who are leaving incarceration.
CMS Issues Guidance to State Medicaid Directors on Medicaid Coverage of SUD, Managed Care Medical Loss Ratio Provisions. The Centers for Medicare & Medicaid Services (CMS) issued on November 19, 2024, guidance to State Medicaid Directors on provisions of the Consolidated Appropriations Act of 2024. Provisions include Section 201, which made permanent the mandatory Medicaid benefit for medications for opioid use disorder; Section 204, which made permanent and amended the state plan option to provide medical assistance for certain individuals in institutions for mental diseases; and Section 211, which made permanent a managed care provision relating to medical loss ratio remittances.
CMS Plans to Adjust Customer Service Call Weighting for MA Star Ratings. Health Payer Specialist reported on November 14, 2024, that the Centers for Medicare & Medicaid Services (CMS) is set to adjust its quality star rating formula to reduce the impact of call centers going forward, according to CMS officials. It is unclear when the changes would go into effect or if these changes would affect the 2025 ratings. Multiple payers have already filed lawsuits challenging the agency’s ratings of their plans in 2025, with Centene specifically citing a single bad customer service call as the decline for many of its ratings.
CMS Releases 2018 Medicare Advantage RADV Audit Methods. The Centers for Medicare & Medicaid Services (CMS) released on November 14, 2024, a report communicating the audit methods and instructions for Medicare Advantage Organizations (MAOs) selected for risk adjustment data validation (RADV) reviews during payment year 2018. Selected MAOs are required to submit a sample of medical records to CMS for validation of risk adjustment data. Contract-specific RADV audits allow CMS to identify overpayments to MAOs.
CMS Releases 2024-28 Comprehensive Medicaid Integrity Plan. The Centers for Medicare & Medicaid Services (CMS) released on November 14, 2024, its Comprehensive Medicaid Integrity Plan (CMIP) for fiscal years 2024 through 2028, which outlines plans to combat fraud, waste, and abuse in Medicaid and the Children’s Health Insurance Plan (CHIP). The CMIP aligns with CMS’ strategic plan and includes four main themes, including; protecting the sustainability of Medicaid and CHIP; engaging with state partners to be mindful of each state’s unique Medicaid program; advancing equity for all Medicaid and CHIP enrollees; and driving innovation to deal with new challenges and risks to the program.
CMS Releases EHB-Benchmark Plan Modernization Grant NOFO. The Centers for Medicare & Medicaid Services (CMS) released on November 13, 2024, a notice of funding opportunity (NOFO) for states with a federally-facilitated exchange (FFE) to apply for the Essential Health Benefits (EHB) Benchmark Plan Modernization Grant. The grant program aims to provide FFE states with funds to review EHB-benchmark plans, with the goal to submit an application to modernize and change the plans. States must have an FFE as of January 1, 2026 to be eligible for funding. Grant applications are due December 15, 2024, and CMS encourages states to submit a Letter of Intent (LOI) for planning purposes, though the LOI is not required.
CMS Releases Rural Health Report, White Paper. The Centers for Medicare & Medicaid Services (CMS) announced on November 12, 2024, that it released a Rural-Urban Disparities in Health Care in Medicare report. CMS also published a white paper, Re-imagining Rural Health: Themes, Concepts, and Next Steps from the CMS Innovation Hackathon Series, which offers recommendations and potential next steps for addressing health challenges in rural communities.
CMS Releases Evaluation of the Oncology Care Model. The Centers for Medicare & Medicaid Services (CMS) announced on November 8, 2024, that it has released an Evaluation of the Oncology Care Model (OCM), which provides analysis of alternative payment methods based on six-month episodes for cancer care for Medicare fee-for- service beneficiaries undergoing chemotherapy treatment. The report shows that practices that adopted two-sided risk drove payment reductions in OCM and achieved net savings totaling $299.6 million.
Improper Medicaid Payments Total $31.1 Billion in Fiscal 2024. Health Payer Specialist announced on November 20, 2024, that improper payments in the Medicaid program reached $31.1 billion in fiscal year (FY) 2024, down from $50.3 billion in FY 2023, which was indirectly credited to the resumption of redeterminations, according to the Centers for Medicare & Medicaid Services. More than 79 percent of the improper Medicaid payments were tied to insufficient documentation and did not indicate fraud. The Medicare Advantage program issued $19.1 billion in improper payments and Medicare fee-for-service issued $31.2 billion in FY 2024.
Health Plans Engaging in Value-based Payment Arrangements Face Provider Barriers, MCO Survey Finds. Healthcare Innovation reported on November 18, 2024, that the percentage of health plans reporting that providers participate in downside risk arrangements has remained below 50 percent and is not expected to increase, impairing adoption of value-based payment (VBP) models, according to the Institute for Medicaid Innovation’s (IMI) annual Medicaid managed care survey. However, health plans have continued to make efforts to implement VBP arrangements, including using strategies to encourage access to care and providing enhanced payment rates for hard-to-recruit provider types. Significant barriers reported included data sharing and readiness; information technology system preparedness; insufficient data to effectively address disparities; and shortage of in-person available behavioral health providers.
President-elect Donald Trump to Nominate Dr. Oz to Head CMS. Reuters reported on November 19, 2024, that U.S. President-elect Donald Trump plans to nominate Dr. Mehmet Oz to serve as administrator for the Centers for Medicare & Medicaid Services (CMS). Oz would work closely with Robert F. Kennedy Jr., who the president-elect intends to nominate to lead the Department of Health and Human Services.
President-elect Donald Trump Nominates RFK Jr. to Head HHS. CQ reported on November 14, 2024, that President-elect Donald Trump announced his intent to nominate Robert F. Kennedy Jr. to be the Health and Human Services (HHS) secretary, which oversees 13 separate agencies. The position still requires Senate confirmation. Trump also has yet to name his picks for other key health care posts including Food and Drug Administration commissioner, Centers for Medicare & Medicaid Services administrator, Centers for Disease Control and Prevention director, and National Institutes of Health director.
GOP Lawmakers Begin Discussions to Cut Spending on Medicaid Program. The Washington Post reported on November 18, 2024, that President-elect Donald Trump’s economic advisers and congressional Republicans have begun preliminary discussions regarding new work requirements and spending caps for Medicaid and other safety-net programs. These discussions are primarily centered on offsetting the cost of extending Trump’s 2017 tax cuts, which are set to expire at the end of 2025. Extending the tax cuts would add more than $4 trillion to the national debt over the next decade, according to congressional bookkeepers.
Industry News
Eli Lily Files Lawsuit Over Use of 340B Drug Pricing Program Rebates. Modern Healthcare reported on November 15, 2024, that Eli Lilly sued the Health and Human Services Department and its sub agency the Health Resources and Services Administration, claiming the agency cannot decide how rebates from the 340B Drug Pricing Program can be used. The lawsuit, filed in the U.S. District Court for the District of Columbia, alleges it should be allowed to vet data from 340B hospitals before offering rebates, rather than providing upfront discounts. Johnson & Johnson filed a similar lawsuit in the same court.
CVS, Cigna, UnitedHealth Sue FTC Over Case on Insulin Cost. CNBC reported on November 19, 2024, that CVS Health, UnitedHealth Group and Cigna filed a lawsuit against the Federal Trade Commission (FTC) claiming the agency’s case against their pharmacy benefit managers (PBMs) raising insulin costs is unconstitutional. The complaint, filed in the U.S. District Court for the Eastern District of Missouri, argues the agency’s administrative court violates the due process rights of the PBM’s under the Fifth Amendment. The action comes after the FTC alleged that large pharmacy benefit managers use illegal rebate programs that raise the price of insulin.
Elevance, Aetna, Cigna Halt Medicare Advantage Broker Commissions in Certain States. Modern Healthcare reported on November 13, 2024, that Aetna, Cigna, and Elevance Health ended Medicare Advantage broker commissions in several states including Connecticut, Georgia, New York, and Texas. Competitor plans are also pulling back broker commissions in those states in the 2025 plan year. The Centers for Medicare & Medicaid Services projects Medicare Advantage enrollment will grow 4 percent to 35.7 million for 2025.
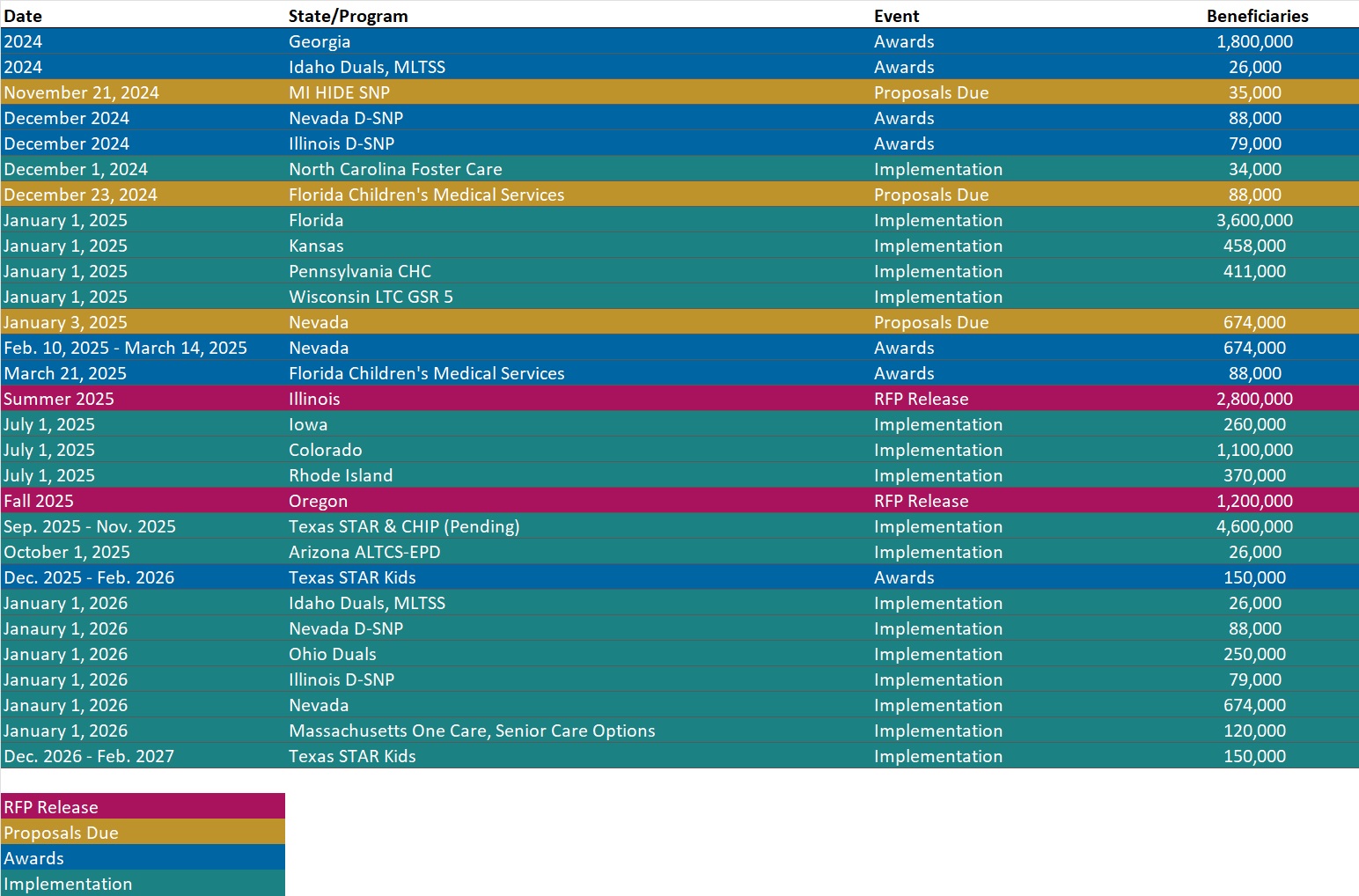
RFP Calendar
HMA News & Events
HMA Webinars:
How Community Care Hubs Can Enhance Family Caregiver Support Services. Tuesday, December 3, 2024, 12 PM ET. To better support family caregivers and the older adults who they care for, Area Agencies on Aging and other aging network agencies are creating Community Care Hubs (CCH) to address social determinants of health, integrate health and social care, and reduce care costs. In this webinar with LTSS policy experts and providers, we will describe the implementation of the CCH model in projects in Massachusetts and New York. Register Here
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
- New State Medicaid Self-directed Program Fiscal Agents Tracker
- New State Medicaid Fact Sheet
- Updated Updated Medicaid Managed Care RFP Calendar: 50 States and DC
- Updated National Medicaid Dental Benefits Management RFP Calendar
- Updated Section 1115 Medicaid Demonstration Inventory
- Updated Massachusetts State Overview
- Updated Minnesota State Overview
- Updated Tennessee State Overview
- HMA Federal Health Policy Quick Takes
Medicaid Data
Medicaid Enrollment:
- Louisiana Medicaid Managed Care Enrollment is Down 11.3%, Sep-24 Data
- Massachusetts Medicaid Managed Care Enrollment is Down 5.1%, Aug-24 Data
- MLRs Average 95.2% at Massachusetts Medicaid MCOs, 2023 Data
- MLRs Average 86.7% at Minnesota Medicaid MCOs, 2023 Data
- New Mexico Medicaid Managed Care Enrollment is Up 1.4%, Jul-24 Data
- North Dakota Medicaid Expansion Enrollment is Down 16.0%, Oct-24 Data
- Pennsylvania Medicaid Managed Care Enrollment is Down 9.7%, Sep-24 Data
- Pennsylvania Medicaid LTSS Enrollment is Down 4.8%, Sep-24 Data
- Virginia Medicaid Managed Care Enrollment is Down 6.7%, Jul-24 Data
- Virginia Medicaid MLTSS Enrollment is Down 4.4%, Jul-24 Data
- Wyoming Medicaid Enrollment Is Up 11.5%, FY 2023 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Florida Children’s Medical Services Program ITN, Nov-24
- Illinois EVV System Vendor RFP, Nov-24
- West Virginia Medicare Advantage D-SNP Contracts, 2025
- Wisconsin Maternal Medicaid Enrollment Projects Funding RFA, Nov-24
Medicaid Program Reports, Data, and Updates:
- Colorado Section 1115 Expanding the SUD Continuum of Care Waiver Documents, 2019-24
- Florida Managed Medical Assistance (MMA) 1115 Demonstration Waiver Approval and Amendments, 2016-24
- Hawaii Quest Integration 1115 Waiver Documents, 2018-24
- Indiana Medicaid Oversight Committee Informational Report, Oct-24
- Louisiana CHIP Annual Reports, SFY 2010-24
- Minnesota Prepaid Medical Assistance Project Plus 1115 Waiver Documents, 2014-24
- New York Medicaid Redesign Team (MRT) 1115 Waiver, Amendments, and Related Documents, 2015-24
- New York Comptroller Medicaid Program EVV Compliance Audit, Nov-24
- North Dakota Medicaid Quality Strategy Plan, 2024
- Pennsylvania Section 1115 Medicaid Coverage for Former Foster Care Youth from a Different State and SUD Demonstration Waiver Application, 2022-24
- Texas Dual Demonstration to Integrated D-SNP Model Transition Timeline, Nov-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
