HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: HMA Annual Conference on Innovations in Publicly Sponsored Healthcare

- California Proposes Increasing Medicaid Reimbursement Rates for Providers

- Florida Disenrolls 250,000 Medicaid Beneficiaries Since Redeterminations Began

- Iowa Releases Dental RFP for Iowa Dental Wellness Plan, Hawki

- Iowa Expects 3,000 Individuals to Lose Medicaid Coverage by June 1

- Massachusetts Considers Increasing Medicaid Reimbursement Rates for Substance Use Disorder Treatment Providers

- Minnesota Legislature Passes Bill to Set Minimum Wages, Benefits for Nursing Home Staff

- Nebraska Passes Certified Community Behavioral Health Clinic Act

- Nevada to Transition to Medicaid Managed Care in Rural Areas

- Nevada Senate Considers Bill to Reimburse Rural Hospitals at Cost for Outpatient Services

- New Hampshire House Committee Subdivision Votes to Hold Medicaid Reauthorization Bill for a Year

- Texas Senate Passes Bill to Extend Postpartum Medicaid Coverage

- Vermont Lawmakers Approve 50 Percent Increase in Fiscal 2024 Medicaid Reimbursement Rates for Dental Services

- Washington Legislature to Increase Medicaid Reimbursement Rates for Nursing Homes by 14 Percent for Two Years

- CMS Releases Regulatory Requirements for State MES Modules

- HCA Healthcare Acquires TX Urgent Care Centers from FastMed

In Focus
HMA Annual Conference on Innovations in Publicly Sponsored Healthcare
Innovations in Publicly Sponsored Healthcare: How Medicaid, Medicare, and Marketplaces
Are Driving Value, Equity, and Growth
Pre-Conference Workshop: October 29, 2023
Conference: October 30−31, 2023
Location: Fairmont Chicago, Millennium Park
Health Management Associates has announced the preliminary lineup of speakers for its sixth annual conference, Innovations in Publicly Sponsored Healthcare: How Medicaid, Medicare, and Marketplaces Are Driving Value, Equity, and Growth.
Hundreds of executives from health plans, providers, state and federal government, investment firms, and community-based organizations will convene to enjoy top-notch content, make new connections, and garner fresh ideas and best practices.
A pre-conference workshop, Behavioral Health at the Intersection of General Health and Human Services, will take place Sunday, October 29.
Confirmed speakers to date include (in alphabetical order):
- Jacey Cooper, State Medicaid Director, Chief Deputy Director, California Department of Health Care Services
- Kelly Cunningham, Administrator, Division of Medical Programs, Illinois Department of Healthcare and Family Services
- Karen Dale, Chief Diversity, Equity, and Inclusion Officer, AmeriHealth Caritas
- Mitchell Evans, Market Vice-President, Policy & Strategy, Medicaid & Dual Eligibles, Humana
- Peter Lee, Health Care Policy Catalyst and former Executive Director, Covered California
- John Lovelace, President, Government Programs, Individual Advantage, UPMC Health Plan
- Julie Morita, MD, Executive Vice President, Robert Wood Johnson Foundation
- Anne Rote, President, Medicaid, Health Care Service Corp.
- Drew Snyder, Executive Director, Mississippi Division of Medicaid
- Tim Spilker, CEO, UnitedHealthcare Community & State
- Stacie Weeks, Administrator/Medicaid Director, Division of Health Care Financing and Policy, Nevada Department of Health and Human Services
- Lisa Wright, President and CEO, Community Health Choice
Publicly sponsored programs like Medicare, Medicaid, and the Marketplaces are leading the charge in driving value, equity, and growth in the U.S. healthcare system. This year’s event will highlight the innovations, initiatives, emerging models, and growth strategies designed to drive improved patient outcomes, increased affordability, and expanded access.
Early bird registration ends July 31. Questions may be directed to Carl Mercurio at [email protected]. Group rates, government discounts, and sponsorships are available.
HMA Roundup
Arkansas
Arkansas Subcommittee Signs Emergency Rule Allowing Facilities to Apply for Rural Emergency Hospital Designation. The Arkansas Democrat Gazette reported on May 19, 2023, that the Arkansas Legislative Council Executive Subcommittee signed an emergency rule that will allow facilities to apply for a Rural Emergency Hospital designation in order to receive additional federal assistance and higher Medicare reimbursement rates. The rule will last 120 days. In April, the state Board of Health approved a permanent rule that still needs to go through a public comment process before it can take effect. Thirty-eight hospitals in Arkansas will be eligible to apply for the Rural Emergency Hospital designation. Read More
California
California Proposes Increasing Medicaid Reimbursement Rates for Providers. CalMatters reported on May 23, 2023, that California officials are proposing an increase in Medicaid reimbursement rates for providers in primary care, maternity care, and non-specialty mental health care to 87.5 percent of Medicare rates. Currently, rates range from 70 to 100 percent of Medicare rates. Read More
Florida
Florida Disenrolls 250,000 Medicaid Beneficiaries Since Redeterminations Began. The Tampa Bay Times reported on May 17, 2023, that Florida has disenrolled about 250,000 Medicaid beneficiaries since beginning eligibility redeterminations on April 18. The state has reviewed more than 461,000 beneficiaries. About 205,000 were disenrolled after failing to respond to requests for information to renew their eligibility, while the remaining 44,000 were ineligible and referred to other forms of coverage. Read More
Illinois
Illinois Senate Committee Advances Bill to Create State-based Insurance Exchange. Health News Illinois reported on May 19, 2023, that the Illinois Senate Executive Committee approved House Bill 579 to create a state-based health insurance Exchange. Under the plan, an initial version would be operational on the federal platform by plan year 2025, with a final version on a state-based platform ready for the 2026 plan year. The bill now heads to the full Senate for a vote. Read More
Iowa
Iowa Releases Dental RFP for Iowa Dental Wellness Plan, Hawki. The Iowa Department of Health and Human Services released on May 18, 2023, a request for proposals (RFP) for pre-paid ambulatory health plans (PAHPs) to provide dental services in the Iowa Dental Wellness Plan and Healthy and Well Kids in Iowa (Hawki) programs. Iowa expects to award three-year contracts to two or more PAHPs, with two optional two-year extensions. Current incumbents are Delta Dental and MCNA Dental. Intent to bid letters are due June 6, with proposals due July 14. Notices of intent to award will be announced November 1 and implementation is anticipated July 1, 2024. Read More
Iowa Expects 3,000 Individuals to Lose Medicaid Coverage by June 1. Radio Iowa reported on May 18, 2023, that Iowa expects more than 3,000 individuals to lose Medicaid coverage by June 1 because of eligibility redeterminations. Of the 150,000 redeterminations, more than 100,000 individuals already had some form of other insurance. The state expects the unwinding process to take a year. Read More
Massachusetts
Massachusetts Considers Increasing Medicaid Reimbursement Rates for Substance Use Disorder Treatment Providers. The Boston Business Journal reported on May 22, 2023, that Massachusetts is considering increasing Medicaid reimbursement rates for substance use disorder treatment providers. Currently, Medicaid reimbursement rates for providers are 50 percent of commercial insurer rates, according to the Massachusetts Association of Behavioral Health Systems. Read More
Minnesota
Minnesota Legislature Passes Bill to Set Minimum Wages, Benefits for Nursing Home Staff. Modern Healthcare reported on May 22, 2023, that the Minnesota legislature passed a bill establishing a board that will set minimum wages and benefits for nursing home staff. The legislation is intended to address the current workforce shortage. It is now headed to Governor Tim Walz, who is expected to sign it. Read More
Nebraska
Nebraska Passes Certified Community Behavioral Health Clinic Act. The Unicameral Update reported on May 19, 2023, that the Nebraska legislature passed the Certified Community Behavioral Health Clinic (CCBHC) Act, with the goal of increasing access to outpatient mental health and substance abuse treatment through coordination with community partners under a prospective payment system. CCBHCs would be implemented by January 1, 2026, pending federal approval of a Medicaid state plan amendment. Read More
Nevada
Nevada to Transition to Medicaid Managed Care in Rural Areas. The Nevada Independent reported on May 22, 2023, that Nevada lawmakers approved funding to transition to Medicaid managed care in rural areas of the state, effective January 2026. Nevada Medicaid beneficiaries are already in managed care plans in Clarke (Las Vegas) and Washoe (Reno) counties, which account for about 75 percent of Medicaid enrollment in the state. Current contracts are set to expire December 31, 2025. The remaining 25 percent of beneficiaries are in fee-for-service, largely in rural areas. Following the transition, about 90 percent of the state’s Medicaid population would be in managed care. Read More
Senate Considers Bill to Reimburse Rural Hospitals at Cost for Outpatient Services. The Nevada Current reported on May 23, 2023, that the Nevada Senate is considering a bill (Senate Bill 241) that would require the state Medicaid program to reimburse Critical Access Hospitals (CAH) in rural areas at cost for outpatient services and swing beds. Hospitals are currently only reimbursed at cost for inpatient services. There are 13 CAHs in rural Nevada, which serve about 250,000 individuals. Read More
Senate Considers Extending Medicaid to Undocumented Individuals Under 17, Pregnant Women. The Nevada Independent reported on May 18, 2023, that the Nevada Senate is considering a bill (Senate Bill 419) to provide Medicaid coverage to individuals who are pregnant and to children under age 17, regardless of immigration status. A previous version of the bill extended coverage to all income-eligible Nevadans. The bill is waiting on a hearing in the Senate Budget Committee. Read More
New Hampshire
New Hampshire House Committee Subdivision Votes to Hold Medicaid Reauthorization Bill for a Year. InDepthNH.org reported on May 23, 2023, that a subdivision of the New Hampshire House Finance Committee voted to hold for a year a bill (Senate Bill 263) that would permanently reauthorize Medicaid expansion. The bill already passed the Senate and received initial approval in the House, pending financial review by the House Finance Committee. The bill will go before the full committee on June 1 for its recommendation for the House session on June 8. Read More
House Passes Bill to Make Medicaid Expansion Permanent. The New Hampshire Bulletin reported on May 18, 2023, that the New Hampshire House passed a bill to permanently expand Medicaid. Originally, the House had only agreed to a two-year extension of the existing Medicaid expansion program. Because the bill involves spending, it must now go to the House Finance Committee for another look. Read More
New York
New York Lawmakers Consider Medicaid Audit Reform Bill. Crain’s New York Business reported on May 22, 2023, that New York lawmakers are considering a bill to reform the Medicaid audit process by preventing auditors from imposing large fines and extending the timeline for providers to correct clerical errors. Lawmakers are also hoping to bring the Medicaid audit process in alignment with practices used by the federal government to audit Medicare providers. A similar bill passed in 2022 but was vetoed by Governor Kathy Hochul. The New York legislative session ends on June 8. Read More
Audit Finds $37.4 Million in Improper Fee-for-Service Medicaid Pharmacy Payments. New York State Comptroller Thomas P. DiNapoli announced on May 18, 2023, that an audit found $37.4 million in improper fee-for-service Medicaid pharmacy payments. The Department of Health and the Office of the Medicaid Inspector General did not ensure that Gainwell Technologies identified claims where Medicaid is incorrectly identified as the primary payer. Another audit found $1.5 million in Medicaid overpayments for durable medical equipment rentals. Read More
Texas
Texas Senate Passes Bill to Extend Postpartum Medicaid Coverage. The Texas Tribune reported on May 21, 2023, that the Texas Senate passed a bill to extend postpartum Medicaid coverage from 60 days to 12 months. The Senate bill includes an amendment stating that the extended coverage is not available if the pregnancy ended with an abortion. The bill now returns to the House, which passed a version without the abortion amendment. Read More
Vermont
Vermont Lawmakers Approve 50 Percent Increase in Fiscal 2024 Medicaid Reimbursement Rates for Dental Services. VTDigger reported on May 23, 2023, that Vermont lawmakers approved $13.1 million in the fiscal 2024 budget that includes a 50 percent increase to Medicaid reimbursement rates for dental services. Lawmakers are expected to work out final details of the approved budget in a special session beginning on June 20. Read More
Washington
Washington Legislature to Increase Medicaid Reimbursement Rates for Nursing Homes by 14 Percent For Two Years. The Everett Herald reported on May 22, 2023, that the Washington legislature included a temporary 14 percent increase in Medicaid reimbursement rates for skilled nursing facilities in fiscal years 2024 and 2025. The legislature will revisit the rates in 2025. Read More
Wisconsin
Hospitals Ask Lawmakers for $185 Million from Budget Surplus to Cover Medicaid Costs. Becker’s Hospital Review reported on May 22, 2023, that the Wisconsin Hospital Association is asking state lawmakers for $185 million per year from the state’s budget surplus to cover Medicaid costs. The request was made in a letter to the Joint Committee on Finance. Read More
National
CMS Releases Regulatory Requirements for State MES Modules. The Centers for Medicare & Medicaid Services (CMS) released on May 24, 2023, guidance for state compliance with regulatory requirements for Medicaid Enterprise System (MES) modules and solutions for states claiming a 75 percent federal match. CMS may periodically review and reapprove each system to ensure compliance with federal requirements. Read More
HHS Proposes Prescription Drug Price Verification Surveys to Increase Transparency. The U.S. Department of Health and Human Services (HHS) announced on May 23, 2023, a proposal to verify drug prices via survey in an effort to reduce Medicaid drug costs and help states in negotiations for certain high-cost medication. The proposal also targets spread pricing and the misclassification of drugs as brand name or generic. Read More
U.S. Representatives Urge House Leaders to Consider Bill to Eliminate DSH Payment Cuts for Fiscal 2024, 2025. RevCycleIntelligence reported on May 23, 2023, that a bipartisan group of U.S. House Representatives are urging Speaker of the House Kevin McCarthy (R-CA) and Democratic Leader Hakeem Jeffries (D-NY) to consider a bill (House Resolution 2665) to eliminate Medicaid Disproportionate Share Hospital (DSH) payment cuts for fiscal 2024 and 2025. The $8 billion cuts are set to begin on October 1 and occur annually through fiscal 2027. Read More
States Partner with Medicaid Plans During Redeterminations Process. InsuranceNewsNet reported on May 22, 2023, that states are partnering with Medicaid managed care organizations (MCOs) to assist with eligibility redeterminations, according to industry group AHIP. MCOs in Maryland are identifying beneficiaries who are at highest risk of losing coverage and conducting outreach. In Nebraska and Rhode Island, plans are providing the state with updated enrollee contact information. Read More
HHS Awards $65 Million to Health Centers to Address Maternal Mortality. The U.S. Department of Health and Human Services (HHS) announced on May 19, 2023, that it has awarded more than $65 million to 35 Health Resources and Services Administration (HRSA)-funded health centers in medically underserved and rural communities to address maternal mortality. Funding will go toward improved maternal health outcomes and reduced disparities among Black and American Indian/Alaska Native women. Read More
Medicaid, Medicare Spending on Dual Eligibles Totals $27,000 Per Person Annually, Study Finds. Health Leaders Media reported on May 19, 2023, that Medicare and Medicaid spending on dual-eligibles totaled nearly $27,000 per person annually, with Medicare accounting for $14,175 and Medicaid $12,698, according to a JAMA Health Forum study. The study concluded that a lack of coordination between Medicare and Medicaid results in higher costs and worse care and that integration is necessary to better serve beneficiaries. Read More
Biden Announces Plan to Combat Homelessness in Major Cities. Spectrum News reported on May 18, 2023, that the Biden administration announced a plan to combat homelessness in Chicago, Dallas, Los Angeles, Phoenix, Seattle, and the state of California through the U.S. Interagency Council on Homelessness and its 19 federal member agencies. As part of the effort, the U.S. Department of Health and Human Services will work to help communities leverage programs such as Medicaid to provide housing-related services. Read More
HHS Releases Guidance to Make It Easier for Schools to Bill Medicaid for Healthcare Services Provided to Students. The U.S. Department of Health and Human Services (HHS) announced on May 18, 2023, guidance designed to make it easier for schools to bill Medicaid for health care services provided to students. The U.S. Department of Education is also proposing a rule that would streamline Medicaid billing permissions for students with disabilities, which would impact approximately 300,000 students. Additionally, HHS approved requests from New Mexico and Oregon to expand access to healthcare services in schools to all Medicaid enrolled students. Read More
U.S. House Speaker Pushes for Medicaid Work Requirements During Debt Ceiling Negotiations. The Hill reported on May 18, 2023, that U.S. House Speaker Kevin McCarthy (R-CA) is pushing for work requirements to be added to Medicaid and the Supplemental Nutrition Assistance Program as part of his plan to avoid default on the country’s debt. House Minority Leader Hakeem Jeffries (D-NY) has said he does not support the proposal. Read More
U.S. House Subcommittee Advances Bill to Regulate PBM Practices. Modern Healthcare reported on May 17, 2023, that the U.S. House Energy and Commerce Committee’s Health Subcommittee advanced a bill that would require pharmacy benefit managers (PBMs) to provide employers with detailed annual data on prescription drug spending, including acquisition costs, out-of-pocket spending, and rebates. The bill would also order the Government Accountability Office to report on health plan pharmacy networks. The bill will now move to the full Energy and Commerce Committee for a vote. Read More
Exchange Plans to Issue $1.1 Billion in MLR Rebates in 2023, KFF Finds. Kaiser Family Foundation (KFF) reported on May 17, 2023, that Exchange plans expect to issue $1.1 billion in medical loss ratio (MLR) rebates in 2023, compared to about $1 billion in 2022. Rebates are calculated on a three-year MLR average and include individual and group lines. Read More
U.S Senators Reintroduce Bill to Make Medicare Telehealth Services Permanent. U.S. Senator Joe Manchin (D-WV) joined other lawmakers on May 17, 2023, in reintroducing the bipartisan Protecting Rural Telehealth Access Act, a bill aimed at making Medicare telehealth flexibilities permanent in rural and underserved communities. Existing telehealth flexibilities are set to expire in December 2024. Read More
U.S. Senators Look Into Medicare Advantage Insurers Using Algorithms to Grant, Deny Access to Care. STAT News reported on May 17, 2023, that U.S. Senators held a hearing on Medicare Advantage insurer practices, with a focus on the use of algorithms to grant or deny access to care. Lawmakers have also asked UnitedHealth Group, Humana, and CVS Health/Aetna for internal documents showing how the decisions to grant or deny care are made. Read More
Union Health Plans to Receive ACA Reinsurance Premium Refunds, Judge Rules. Health Payer Specialist reported on May 17, 2023, that 350 health and welfare benefit plans — many run by labor unions — will get back $185.2 million in reinsurance premiums paid under the Affordable Care Act (ACA), according to a summary judgement by U.S. Court of Claims Judge Eleni Roumel. A group of unions filed the suit in March 2019, arguing they were exempt from the payments under federal law. The case was certified as a class-action in June 2022. Read More
Industry News
HCA Healthcare Acquires TX Urgent Care Centers from FastMed. Modern Healthcare reported on May 18, 2023, that HCA Healthcare will acquire 41 urgent care centers based in Texas from FastMed. HCA already has 45 hospitals, 395 physician practices, and 92 urgent care centers in Texas. Terms of the agreement were not disclosed. Read More
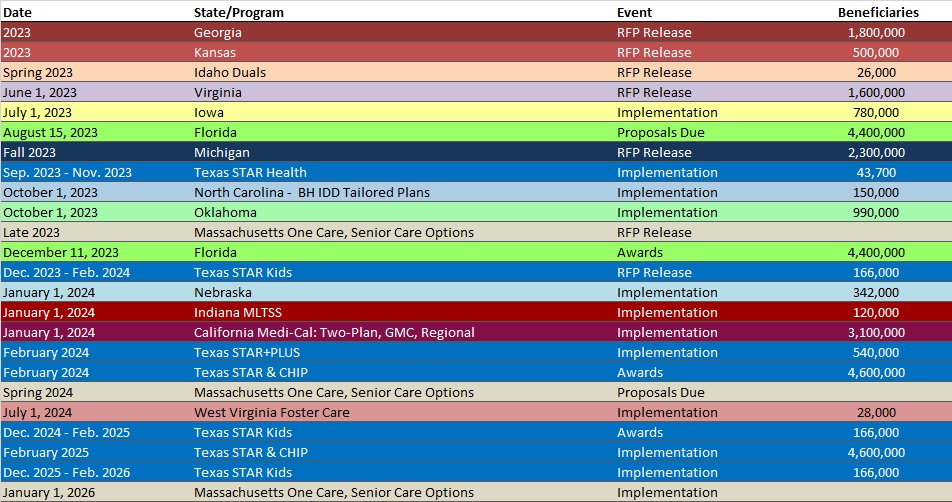
RFP Calendar
Company Announcements
MCG White Paper:
Procedures and the Continuing Shift Toward Ambulatory Care. In this white paper, Milliman’s Senior Director of Clinical Analytics, Lashana Narayan, ASA, MAAA, and MCG’s Clinical Coding Analyst, Pierre Malek, MD, discuss the continuing trend of surgical procedures shifting from the inpatient to outpatient setting. Read More
HMA News & Events
Upcoming HMA Webinar:
Opportunities for State Payers to Improve & Align Incentives for Treatment of Substance Use Disorder. HMA’s 3-part webinar series on New Rules in Treatment of Opioid Addiction is aimed at helping stakeholders prepare for new federal rules that will change how medications are delivered to persons with opioid use disorders. Part 2 highlights Opportunities for State Payers to Improve & Align Incentives so providers can expand access to treatment enabled by new federal regulations that encourage patient-centered care. Tuesday, June 6, 2023, 3pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Iowa Medicaid Managed Care Enrollment is Up 2.9%, Apr-23 Data
- New York Medicaid Managed Care Enrollment is up 4.6%, Feb-23 Data
- New Mexico Medicaid Managed Care Enrollment is Up 0.9%, Mar-23 Data
- Ohio Medicaid Managed Care Enrollment is Up 6.7%, Feb-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 1.6%, Mar-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 0.9%, Apr-23 Data
- Texas Medicaid Managed Care Enrollment is Up 10.6%, Nov-22 Data
- Texas Dual Demo Enrollment is 33,673, Nov-22 Data
- Texas Medicaid Managed Care Enrollment is Up 1.8%, Feb-23 Data
- Texas Dual Demo Enrollment is 33,419, Feb-23 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 2.2%, Apr-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Iowa Asset Verification System RFI, May-23
- Iowa Dental Wellness Plan and Hawki Dental Pre-Paid Ambulatory Health Plan (PAHP) RFP, May-23
- Minnesota Medicaid Enterprise Level Interoperability RFI, May-23
- Ohio Benefits Long-Term Services and Supports Service Provider Data Base and Website Management RFP, May-23
Medicaid Program Reports, Data, and Updates:
- Arizona Annual HCBS Reports, FY 2019-22
- Florida Annual External Quality Review Reports, 2012-22
- Iowa Medicaid MCO Quarterly Performance Data Reports, 2016-23
- Louisiana Medicaid Financial Forecast Reports, SFY 2018-23
- Massachusetts Medicaid Managed Care Capitated Rate Certifications and Appendices, 2022
- Massachusetts Medicaid Managed Care Capitated Rate Certifications and Appendices, 2023
- South Carolina Plan for HCBS Implementation of the American Rescue Plan Act and Quarterly Reports, 2021-23
- Texas Medicaid CHIP Data Analytics Unit Quarterly Reports, 2018-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
