HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: President’s Budget Recommends Significant Investments in Unity Agenda Issues

- HMA Conference: Drew Altman of KFF to Deliver Keynote Address on Politics and the ‘New Normal’ for U.S. Healthcare at HMA Conference in Chicago, October 10-11

- Arkansas Eligibles Face Barriers Enrolling in Medicaid, Report Finds

- Connecticut Medicaid Enrollment Increases by 120,000 During Pandemic

- Florida Medicaid Plan Has New Enrollment Suspended by State

- Kansas Governor Urges Legislature to Remove Budget Bill Provision to Extend KanCare Contracts

- Michigan Home-Based Care Providers Struggle After Reimbursement Rate Cut

- New Hampshire Hospitals Can Proceed with Lawsuit Over Vermont Over Medicaid Rates

- North Carolina Launches Initiative to Provide Integrated Care for Children On Medicaid, CHIP

- Pennsylvania to Release MMIS RFP in September 2022

- South Carolina Receives CMS Approval of Temporary HCBS Rate Increases

- Health Plan Invests More Than $85 Million to Help Develop Affordable Housing in Texas

- Medicaid Spending Will Exceed $1 Trillion in 2028, CMS Projects

- Optum Health to Acquire LHC Group for $5.4 Billion

- New this week on HMAIS

In Focus
President’s Budget Recommends Significant Investments in Unity Agenda Issues
This week, our In Focus section reviews President Biden’s budget proposal for federal fiscal year 2023, released on March 28, 2022. The President’s proposal kicks off the Congressional budget process and negotiations on the annual spending bills for the federal fiscal year that starts October 1, 2022. The budget proposal highlights the Administration’s program initiatives and recommended legislative and regulatory changes. The President’s budget is merely a request of Congress, who drafts the actual budget resolution that will go into effect if passed.
President Biden previewed several major initiatives in his State of the Union address earlier this month, and the budget request includes details his recommended funding and policy changes to advance these priorities. Cutting across all aspects of the Administration’s budget plan are efforts focused on racial equity, including health equity. HMA and Leavitt Partners, an HMA company, are closely monitoring the policies that fall into what the President has called his “Unity Agenda”, including:
- Reforms to address the mental health crisis, including parity in coverage across federally funding programs and development of the mental health workforce;
- Bolstering services to help individuals with and at risk of substance use disorders
- Investments to reduce cancer death; and
- Funding for the Advanced Research Projects Agency for Health (ARPA-H).
In the remainder of our post we provide a snapshot of the Department of Health and Human Services’ budget proposals
Medicare
The President’s budget includes several behavioral health proposals in the Medicare program. For example, the Administration calls on Congress to:
- Extend mental health and addiction parity to Medicare
- Allow Medicare to cover three behavioral health visits without cost-sharing;
- Reimburse for services provided by community health workers, including behavioral health coordination; and
- Expand the types of providers and remove limits on scope of services that are eligible for Medicare reimbursement.
Additionally, the budget addresses looming reimbursement issues for Medicare physicians. The budget recommends Congress update the physician fee schedule by 0.25 percent for clinicians who do not participate in Medicare’s approved alternative payment models (APMs), and 0.75 percent annually for those who do, beginning in performance year 2023 for payment in 2025 instead of 2026. This change would increase Medicare’s costs by $3.5 billion through 2032.
The budget proposal also states that the Administration is committed to supporting a temporary extension of broader telehealth coverage under Medicare beyond the COVID-19 Public Health Emergency declared by the Secretary in order to study its ability to promote proper use and access to care. The recently enacted spending bill for the current fiscal year extends many of the temporary telehealth policies already in place for an additional 151 days following the end of the PHE declaration. It also required the Medicare Payment and Advisory Commission to report on several aspects of telehealth by June 15, 2023, and directs CMS to begin publishing telehealth data by July 1, 2022. The Administration’s ongoing support for temporary extension of the policies could be critical while policymakers wait on MedPAC and other expected analyses.
Medicaid
The budget plan for Medicaid also includes a significant focus on mental health services, including calling on Congress to:
- Make permanent the current demonstration for Certified Community Behavioral Health Clinics. [$24 billion over 10 years]
- Provide $7.5 billion for planning grants and a Medicaid provider capacity demo for mental health treatment.
- Require state Medicaid programs to allow reimbursement for mental health and physical health visits provided to a Medicaid enrollee which happen on the same day.
Notably, HHS recommends Congress give CMS new managed care program oversight and enforcement tools. In particular, CMS is seeking the ability to withhold the federal match in Medicaid managed care plan contract capitation payment amounts on a service-by-service basis. Currently, CMS’s only recourse when it identifies compliance failures is to withhold all federal match under the contract, which has proven untenable in many situations. The Administration projects it will result in $2.1 billion in savings over ten years. This could be attractive to Congress if it needs to identify proposals that generate federal savings (or “offsets”) to increase federal expenditures for other policies or reduce the deficit.
Behavioral Health
In addition to parity in Medicare, the Administration recommends Congress extend enforcement of mental health and addiction parity requirements in commercial insurance, TRICARE, and the Veteran’s Affairs healthcare system. The budget seeks to enhance mental health parity in the individual and group insurance markets by:
- Requiring coverage of three behavioral health visits and three primary care visits without cost-sharing [$310 million in costs over 10 years];
- Increasing mental health parity enforcement through new regulations on behavioral health network adequacy, and standards for parity in reimbursement rates based on the results of comparative analyses submitted by plans and issuers. [$720 million over 10 years]; and
- Providing new grants to states to enforce behavioral health parity [$125 million over 5 years].
Generally, the budget recommends increasing investments in numerous behavioral health programs administered by HHS agencies and other federal programs. For example, the budget prioritizes several behavioral health workforce initiatives, 9-8-8 implementation efforts, Project Aware, the Children’s Mental Health Services program, and community-based mental health services. There is a strong interest in supporting comprehensive, coordinated, and integrated state efforts to make schools safer and increase access to mental health services. The budget proposes to increase funding for the State Opioid Response (SOR) grant program by $475 million.
Congress is also working on a bipartisan basis to address mental health and substance use disorder prevention, evidence-based treatment, and support services. The President’s priorities in this area could help shape final spending levels and a consensus mental health package that could take shape as the year goes on.
Public Health and Pandemic Preparedness
The President’s budget request includes $88.2 billion in new mandatory spending over a 5-year period for biodefense & preparedness, vaccine development, and technology infrastructure. $40 billion of this amount would be allocated to the HHS Assistant Secretary for Preparedness and Response (ASPR) to:
- Expand the nation’s manufacturing capacity through capital investments focused on manufacturing infrastructure and technology, especially for warm surge capacity for vaccines, therapeutics, tests, personal protective equipment, and medical equipment;
- Support “end-to-end” advanced development and manufacturing scale-up of prototype vaccines and therapeutics against the highest priority viral families;
- Support the advanced development and procurement of diagnostics, advanced disease surveillance technologies, next-generation personal protective equipment, and other medical countermeasure technologies;
- Refill and modernize depleted pandemic stockpiles;
- Expand the public health workforce; and
- Manage the mission within ASPR, which will include recruiting staff and centralizing coordination efforts to ensure alignment of activities across HHS.
The budget also includes a $28 billion investment for CDC to enhance public health system infrastructure, domestic and global threat surveillance, public health workforce development, public health laboratory capacity, and global health security.
What’s Next
The President’s budget request underscores the likelihood of bipartisan action this year on mental and behavioral health, the opioid crisis, the Cancer Moonshot, and biomedical innovation. It is less clear if Congress will be able to pass more partisan health policies included in the
Build Back Better Act, such as expanding the Affordable Care Act’s subsidies and giving Medicare the power to negotiate drug prices. Beginning this week, agency officials will testify before these committees to justify and explain their budget requests to Congress and respond to questions from committee members.
This post covers a portion of the important programs within the Department of Health and Human Services. For inquiries about the potential implications of the budget proposal for your agency/health plan/provider/stakeholder and how you can engage in or keep tabs on the federal process going forward, please contact Andrea Maresca at Health Management Associates and Liz Wroe at Leavitt Partners.
__________________
Drew Altman of KFF to Deliver Keynote Address on Politics and the ‘New Normal’ for U.S. Healthcare at HMA Conference in Chicago, October 10-11
Drew Altman, president and chief executive of the Kaiser Family Foundation, will deliver the keynote address on Politics and the “New Normal” for U.S. Healthcare at the HMA conference, October 10-11, 2022, at the Fairmont Chicago, Millennium Park. To register visit https://conference.healthmanagement.com/.
Altman will discuss the politics of healthcare at the state and federal level, including a look at how the midterm elections may further complicate efforts to reach a consensus on necessary changes and improvements to the U.S. healthcare system in the wake of COVID-19.
The overall theme of this year’s conference is How Medicaid, Medicare, and Other Publicly Sponsored Programs Are Shaping the Future of Healthcare in a Time of Crisis.
This is the fifth conference HMA has presented on trends in publicly sponsored healthcare. Our last event brought together 500 executives and more than 40 speakers from health plans, providers, state and federal government, community-based organizations and others serving Medicaid, Medicare, and other vulnerable populations.
Other confirmed speakers to date include (in alphabetical order):
State Medicaid Priorities, Challenges – Now and After the Public Health Emergency
Jacey Cooper, Medicaid Director, Chief Deputy Director, California Department of Health Care Services
Allison Matters Taylor, Medicaid Director, Indiana
Dave Richard, Deputy Secretary, North Carolina Medicaid
Jami Snyder, Director, Arizona Health Care Cost Containment System
Key Strategies, Opportunities, and Concerns for Medicaid Managed Care
Aimee Dailey, President, Medicaid, Anthem, Inc.
Brent Layton, President, COO, Centene Corporation
Kelly Munson, President, Aetna Medicaid
Timothy Spilker, CEO, UnitedHealthcare Community & State
The Role of Health Plans, Providers, and States in Addressing Health Equity
Kody Kinsley, Secretary, North Carolina Department of Health and Human Services
Additional planned sessions to focus on Medicare, dual eligibles, social determinants of health, eligibility redeterminations, long-term care, long-term services and supports, behavioral health, substance use disorder, healthcare investing, pharmacy benefits, and healthcare information technology.
HMA will also host a pre-conference workshop on Sunday, October 9, on important trends and developments in value-based care.
Sponsorships and group discounts are available. For additional information, contact Carl Mercurio.
HMA Roundup
Arkansas
Arkansas Eligibles Face Barriers Enrolling in Medicaid, Report Finds. KFSM reported on March 23, 2022, that individuals in Arkansas face barriers enrolling in Medicaid, such as long wait times, unanswered phone calls, and a hard-to-navigate website, according to a report by Arkansas Community Organizations and Columbia University. The report offers recommendations for improving the Medicaid application process, including strengthening customer support and simplifying the application process. Read More
Colorado
House Committee Advances Bill to Expand Medicaid to Pregnant Women, Children Regardless of Immigration Status. The Denver Channel reported on March 25, 2022, that the Colorado House Public and Behavioral Health and Human Services committee advanced a bill (HB22-1289) to extend Medicaid eligibility to eligible pregnant women and children regardless of immigration status. The bill also creates an outreach strategy for enrolling eligible groups in coverage and aims to improve the quality of Exchange plans. Read More
Connecticut
Connecticut Medicaid Enrollment Increases by 120,000 During Pandemic. The Connecticut Insider reported on March 30, 2022, that Connecticut Medicaid enrollment increased by 120,000 to about 969,000 from March 2020 to February 2022, driven by continuous eligibility requirements. State officials are working to ensure individuals will be contacted when eligibility redeterminations resume after the end of the public health emergency. Read More
Florida
Florida Medicaid Plan Has New Enrollment Suspended by State. Modern Healthcare reported on March 25, 2022, that the Florida Agency for Health Care Administration suspended new Medicaid and long-term care enrollment in Centene/Sunshine State Health Plan over improper claims denials. The plan can begin enrolling new individuals again after it pays a $9.1 million fine, submits a plan for reprocessing claims, and demonstrates that future claims are paid promptly. Read More
Florida Fines Medicaid Plan $9.1 Million for Improper Claims Denials Tied to Technology Issues. The Tampa Bay Times reported on March 23, 2022, that Florida fined Centene/Sunshine State Health Plan nearly $9.1 million for technology problems resulting in more than 121,000 improperly denied Medicaid claims from providers serving critically ill children. The state Agency for Health Care Administration also demanded an explanation of the problem and evidence that future claims would be paid in a timely manner. Read More
Idaho
Idaho Medicaid Rates for Long-Term Care, Dental, Community Services Remain Largely Unchanged, Watchdog Finds. The Idaho Capital Sun reported on March 30, 2022, that Idaho Medicaid reimbursement rates for benefits including long-term care, dental services, and community supports for individuals with disabilities have remained largely unchanged for years, according to a report by the Idaho Legislature Office of Performance Evaluations. The report, which was created at the request of the state’s Joint Legislative Oversight Committee, blamed a lack of administrative capacity to establish a rate review process and a lack of trust from state legislators. Read More
Illinois
Illinois Health Benefits for Immigrant Adults Program Enrolls 9,000 Undocumented Seniors in First Year. Modern Healthcare/The Associated Press reported on March 26, 2022, that the Illinois Health Benefits for Immigrant Adults program enrolled roughly 9,000 undocumented seniors in 2021, the first year of the program. The program, which is aimed at individuals who are ineligible for Medicaid and Medicare because of immigration status, does not cover long-term care or community-based health services. Read More
Indiana
Indiana Expands Medicaid Coverage for Pregnant Women, Postpartum Benefits. The Northwest Indiana Times reported on March 22, 2022, that Indiana enacted legislation covering pregnant women up to 208 percent of poverty and extending Medicaid postpartum coverage to 12 months. Previously, Medicaid coverage was available to pregnant women up to 200 percent of poverty, and postpartum coverage lasted six weeks. Read More
Kansas
Governor Urges Legislature to Remove Budget Bill Provision to Extend KanCare Contracts Through 2024. The Kansas Reflector reported on March 29, 2022, that Kansas Governor Laura Kelly issued a letter to state legislative leaders urging the removal of a budget bill provision that would extend existing Kansas Medicaid managed care contracts through December 2024. The letter comes after Kansas Attorney General Derek Schmidt said the legislature has the power to prevent the current administration from rebidding the Medicaid contracts in October 2022 as planned. The budget bill recently passed the Kansas House. Read More
House Passes Bill to Extend KanCare Contracts Through 2024. The Topeka Capital-Journal reported on March 23, 2022, that the Kansas House passed a budget bill, requiring the state to extend existing Kansas Medicaid managed care contracts through December 2024. The contracts are currently set to expire at the end of 2023, and the state has been preparing to release a request for proposals in October 2022. The extension would mean the next procurement would occur after the gubernatorial election. Read More
Kentucky
Senate Committee Advances Bill to Tighten Medicaid Eligibility Requirements. WKU Public Radio reported on March 29, 2022, that the Kentucky Senate Health and Welfare Committee advanced a bill (House Bill 7) to tighten Medicaid eligibility requirements, including requiring able-bodied Medicaid beneficiaries to participate in 80 hours per month of work, volunteering, or other community activities. The bill now moves to the full Senate. Read More
Michigan
Michigan Home-Based Care Providers Struggle After Reimbursement Rate Cut. Home Health Care News reported on March 27, 2022, that home-based care providers in Michigan are struggling financially since the state legislature cut reimbursement rates, according to Barry Cargill, chief executive, Michigan HomeCare & Hospice Association. Cargill said that since July 2, 2021, roughly 3,000 people have lost their jobs, and more than 20 home-care providers have closed. Read More
Montana
Montana Spends Medicaid Funds on Out-of-State Behavioral Care at Troubled Residential Facilities for Children. Kaiser Health News reported on March 25, 2022, that Montana is sending troubled children out of state for behavioral health and substance use disorder treatment, in some cases to residential facilities accused of abuse. As of March 2022, there were approximately 90 Montana children being treated out-of-state. Read More
Nebraska
Nebraska Anthem/Healthy Blue Health Plan Names Rob Rhodes President. Nebraska Medicaid managed care plan Anthem/Healthy Blue Nebraska announced on March 28, 2022, that Rob Rhodes has been named president. Rhodes previously served as chief medical officer for Healthy Blue. Read More
New Hampshire
New Hampshire Hospitals Can Proceed With Lawsuit Against Vermont Over Medicaid Rates, Judge Rules. Bloomberg Law reported on March 23, 2022, that New Hampshire hospitals can proceed with a lawsuit against the state of Vermont over Medicaid rates paid to out-of-state providers, a federal judge ruled. However, the judge dismissed claims against U.S. Health and Human Services Secretary Xavier Becerra and other federal defendants, ruling they did not have a role in the state’s rate setting. Read More
New York
New York Launches Assertive Community Treatment Program for Children. Crain’s New York Business reported on March 30, 2022, that New York Governor Kathy Hochul announced the state will spend $21 million to launch its Assertive Community Treatment program for children aged 10 to 21 and their families. The program will support an estimated 600 New Yorkers who have not responded well to traditional behavioral health treatments and are at risk of entering residential or inpatient psychiatric programs. The funding comes from a one-time $6 million federal grant through the Community Mental Health Services Block Grant and Federal Medical Assistance Percentage programs, and the remaining $15 million is from the state and Medicaid reimbursements. Read More
New York Home Care Providers File Lawsuit to Halt Planned Distribution of Pandemic Stimulus Funds. Potomac Law Group announced on March 21, 2022, that a group of New York Licensed Home Care Services Agencies has filed a lawsuit arguing that the New York State Department of Health should halt the distribution of $361 million in COVID-19 stimulus as planned on March 31. The group argues that funds will go to the largest agencies, while leaving smaller agencies behind. Read More
New York Receives CMS Approval of 5-Year Medicaid 1115 Waiver Renewal. The New York State Department of Health announced on March 24, 2022, that the Centers for Medicare & Medicaid Services (CMS) granted approval of the state’s Medicaid Section 1115 waiver renewal for five years through March 31, 2027. CMS extended the current waiver and approved an amendment to permit dual eligibles who enroll in a Medicare Dual Eligible Special Needs Plan to stay enrolled in a mainstream Medicaid managed care plan under certain criteria. Read More
North Carolina
North Carolina Launches Initiative to Provide Integrated Care for Children Covered by Medicaid, CHIP. North Carolina announced on March 24, 2022, the launch of the state’s Integrated Care for Kids (NC InCK) program in five counties (Alamance, Orange, Durham, Granville, and Vance). The program, which is expected to serve approximately 95,000 children on Medicaid and the Children’s Health Insurance Program (CHIP), is a partnership of Duke University, UNC Health, and the NC Department of Health and Human Services. Read More
Oregon
Oregon Medicaid CCO Wins State Settlement After Long Legal Battle. Modern Healthcare reported on March 27, 2022, that the Oregon Health Authority (OHA) will pay Medicaid coordinated care organization FamilyCare, Inc. $22.5 million to settle a dispute over rates. OHA admitted no wrongdoing in the settlement. FamilyCare, which will donate the funds to a local medical school, has shrunk from 370 employees to four. Read More
Pennsylvania
Pennsylvania to Release MMIS RFP in September 2022; EQRO RFP in July 2022. The Pennsylvania Department of Human Services announced that it will release a request for proposals (RFP) on September 1, 2022, for a vendor to take over the state’s Medicaid management information system (MMIS). Implementation is targeted for November 1, 2024. The state will also release a solicitation for an external quality review organization on July 1, 2022.
South Carolina
South Carolina Receives CMS Approval of Temporary HCBS Rate Increases. The South Carolina Department of Health and Human Services (SCDHHS) announced on March 29, 2022, that the Centers for Medicare & Medicaid Services (CMS) approved a request to amend multiple Medicaid waivers to include Emergency Preparedness and Response Appendix K, which temporarily raises reimbursement rates for some home and community-based services. Appendix K also increases individual cost limits for the community supports waiver and service limits for waiver case management. Appendix K is effective through six months after the end of the public health emergency, after which SCDHHS will submit waiver amendments for permanent rate increases. Read more
South Carolina Extends Postpartum Medicaid Coverage from 60 Days to 12 Months. The South Carolina Department of Health and Human Services announced on March 29, 2022, that postpartum Medicaid coverage will be extended from 60 days to 12 months, effective April 22, 2022. Read More
Texas
Health Plan Invests More Than $85 Million to Help Develop Affordable Housing in Texas. Anthem/Amerigroup Texas announced on March 28, 2022, an investment of more than $85 million to help develop affordable housing in Texas through the federal Low Income Housing Tax Credit program. Anthem has invested $410 million nationwide to address social determinants of health. Read More
Texas Receives CMS Approval for Directed Payment Programs. The Texas Health and Human Services Commission announced on March 25, 2022, that it had received approval from the Centers for Medicare & Medicaid Services (CMS) for the state-directed payment programs (SDPs) included in Texas’ Section 1115 waiver renewal application. The approved SDPs are the Comprehensive Hospital Increase Reimbursement Program, Texas Incentives for Physicians and Professional Services, and Rural Access to Primary and Preventive Services Program. The waiver was initially approved at the end of the Trump administration, but approval was rescinded by CMS under the Biden administration. Read More
National
Federal, State Governments Could See $7.7 Million in Cost Savings by Providing Dental Coverage to Adults with I/DD, Report Finds. The National Council on Disability reported on March 9, 2022, that providing Medicaid dental benefits to adults with intellectual and developmental disabilities (I/DD) would save federal and state governments $7.7 million annually by preventing the need for costly emergency dental services and development of chronic disease. The report, prepared for President Biden, found that 12 states currently provide no or limited dental benefits to adults with ID/D enrolled in Medicaid, and that oral health is necessary for physical health. Read More
Medicaid Spending Will Exceed $1 Trillion in 2028, CMS Projects. The Centers for Medicare & Medicaid Services (CMS) released on March 28, 2022, the 2021-30 National Health Expenditure (NHE) report, which projects Medicaid spending to exceed $1 trillion in 2028. The average annual growth rate for Medicaid spending is expected to be 5.6 percent from 2021-30, after an expected increase of 10.4 percent in 2021. The report also projects annual Medicare spending to average 7.2 percent from 2021-30. Total national healthcare expenditures are expected to average 5.1 percent, reaching nearly $6.8 trillion by 2030. That is on par with projected GDP grow, suggesting healthcare spending as a percentage should remain flat. Read More
U.S. Senator Introduces Bill to Expand Asset Verification Services Program to All Medicaid Applicants. U.S. Senator John Kennedy (R-LA) announced on March 24, 2022, the introduction of a bill (Protecting Medicaid Beneficiaries Act) that would expand the Asset Verification Services (AVS) program to all Medicaid applicants. AVS currently applies only to aged, blind, and disabled Medicaid applicants. Read More
Hospitals, Long-Term Care Providers Petition for Extension of Public Health Emergency. Fierce Healthcare reported on March 28, 2022, that several hospital and long-term care groups called on the Biden administration to extend the public health emergency for another 90 days past the scheduled April 16 expiration date. The groups wrote to Department of Health and Human Services Secretary Xavier Becerra, expressing concerns over continued labor shortages, potential future COVID-19 surges, and an influx of deferred care. Read More
Biden Proposes Nearly $52 Billion to Improve Mental Health System for Medicaid Beneficiaries. Modern Healthcare reported on March 28, 2022, that President Biden issued a fiscal 2023 budget proposal seeking $51.7 billion to improve the nation’s mental health system, including $35.4 billion to enhance mental health access and $7.5 billion for workforce development. The proposal would also require health insurers to cover mental healthcare with adequate provider networks and to ensure parity in coverage between behavioral health and medical benefits. In total, the budget proposal is asking Congress for a 27 percent increase in discretionary funding for the Department of Health and Human Services to $127.3 billion. Read More
MACPAC Issues Brief Showing Limitations of Medicaid Race, Ethnicity Data. The Medicaid and CHIP Payment and Access Commission (MACPAC) issued a brief on March 29, 2022, showing that limitations in race and ethnicity data make it difficult to accurately address disparities and promote equity of care among Medicaid populations. The brief looked at federal standards for capturing information on race and ethnicity, federal requirements for monitoring disparities in Medicaid, and the availability of such information in Medicaid administrative data, specifically the Transformed Medicaid Statistical Information System. Read More
Medicaid, CHIP Had Nearly 86 Million Enrollees as of November 2021. The Centers for Medicare & Medicaid Services (CMS) reported on March 28, 2022, that 85.8 million individuals were enrolled in Medicaid and the Children’s Health Insurance Plans (CHIP) as of November 2021, up 980,636 from September 2021. Another 64.2 million were enrolled in Medicare as of December 2021, including 28 million in Medicare Advantage plans and 11.8 million dual eligibles. Read More
US Senators Request GAO Study on Low COVID-19 Vaccination Rate Among Medicaid Beneficiaries. Kaiser Health News reported on March 25, 2022, that U.S. Senators Robert Casey Jr. (D-PA) and Ron Wyden (D-OR) have asked the Government Accountability Office (GAO) to study why COVID-19 vaccination rates among Medicaid beneficiaries are lower than the general population. There is a 15 to 20 percent difference in vaccination rates between Medicaid beneficiaries and individuals with other forms of coverage, according to a Duke University report. The Senators also want the GAO to look into barriers that states face in their efforts to increase vaccination rates. Read More
Bipartisan Bill Would Expand Access to Treatment for Medicaid Beneficiaries Struggling With Substance Use Disorder. The Times Weekly reported on March 23, 2022, that U.S. Congressman Bill Foster (D-IL) introduced the Medicaid Coverage for Addiction Recovery Expansion (CARE) Act (House Resolution 7156) to expand access to treatment for Medicaid beneficiaries struggling with substance use disorder. The bill is co-sponsored by Representatives Brian Fitzpatrick (R-PA), Sheila Jackson Lee (D-TX), Gwen Moore (D-WI), Joyce Beatty (D-OH), and Jeff Van Drew (R-NJ). Read More
Defense Health Agency Releases RFI for TRICARE Competitive Plans Demonstration Program. The Defense Health Agency (DHA) released on March 22, 2022, a request for information (RFI) for a Competitive Plans Demonstration (CPD) project, which will open one or more of 23 potential TRICARE markets for competition from local or regional health plans. If approved, DHA will initiate the demonstration in 2024. Responses are due on April 22.
CMS Announces Value-Based Payment Arrangements for Medicaid Drug Rebate Program. The Centers for Medicare & Medicaid Services (CMS) announced on March 23, 2022, that states and drug manufacturers can enter into drug therapy value-based payment (VBP) arrangements as a part of the Medicaid Drug Rebate Program (MDRP) beginning on July 1. States can earn rebates or price concessions based on the clinical outcomes of these drugs among Medicaid beneficiaries. Read More
AHIP Submits Amicus Brief in Support of Eliminating Overpayment Rule. Modern Healthcare reported on March 24, 2022, that America’s Health Insurance Plans (AHIP) submitted an amicus brief to the U.S. Supreme Court in support of eliminating the Medicare Advantage overpayment rule. The original lawsuit was filed by UnitedHealthcare. The overpayment rule gives Medicare Advantage plans 60 days to return overpayments to the federal government or potentially face civil lawsuits, damages and penalties. Read More
Industry News
Health Plan Foundation Invests $5.5 Million to Address Social Determinants of Health. The Humana Foundation announced on March 29, 2022, a continued investment to promote health equity, financial security, food security, and social connections through a $5.5 million investment in nine organizations in Florida, Kentucky, Louisiana, and Texas. Initial investments were made in 2019, and funding has continued based on achievement of specific metrics. Read More
Optum Health to Acquire LHC Group for $5.4 Billion. Optum Health announced on March 29, 2022, an agreement to acquire in-home healthcare services provider LHC Group for $170 per share or about $5.4 billion. The deal is expected to close in the second half of 2022. Read More
Traditions Health Acquires Serenity Health Management. Hospice News reported on March 21, 2022, that Traditions Health acquired Serenity Health Management, a hospice and home health provider based in Wichita, KS. Traditions Health, which is a portfolio company of Dorilton Capital Advisors, provides hospice, home health care, and consulting services to about 5,000 individuals in 17 states. Read More
Caregiver Acquires Bethesda Lutheran Communities, Majority of Compass Residential & Consulting. Caregiver, Inc. announced on March 22, 2022, the acquisition of Bethesda Lutheran Communities, a provider of services to individuals with intellectual and developmental disabilities (IDD), and the residential and community-based assets of Compass Residential & Consulting, a provider of home and community-based services (HCBS) in seven Indiana counties. Caregiver provides HCBS to individuals with IDD through affiliates in Texas, Georgia, Tennessee, Indiana, and Ohio. Read More
24 Hour Home Care Acquires Bright Moon Care Services. California-based 24 Hour Home Care announced on March 17, 2022, the acquisition of Bright Moon Care Services, a home care agency that specializes in personal care for seniors in Ventura County. The deal was effective February 28, 2022. Read More
UnitedHealth Acquires Refresh Mental Health. Health Payer Specialist reported on March 24, 2022, that UnitedHealth has acquired Florida-based Refresh Mental Health from private equity fund Kelso & Co. Refresh, which specializes in treatment for mental health, substance use disorder, and eating disorders, operates 300 outpatient behavioral health centers across 37 states. Read More
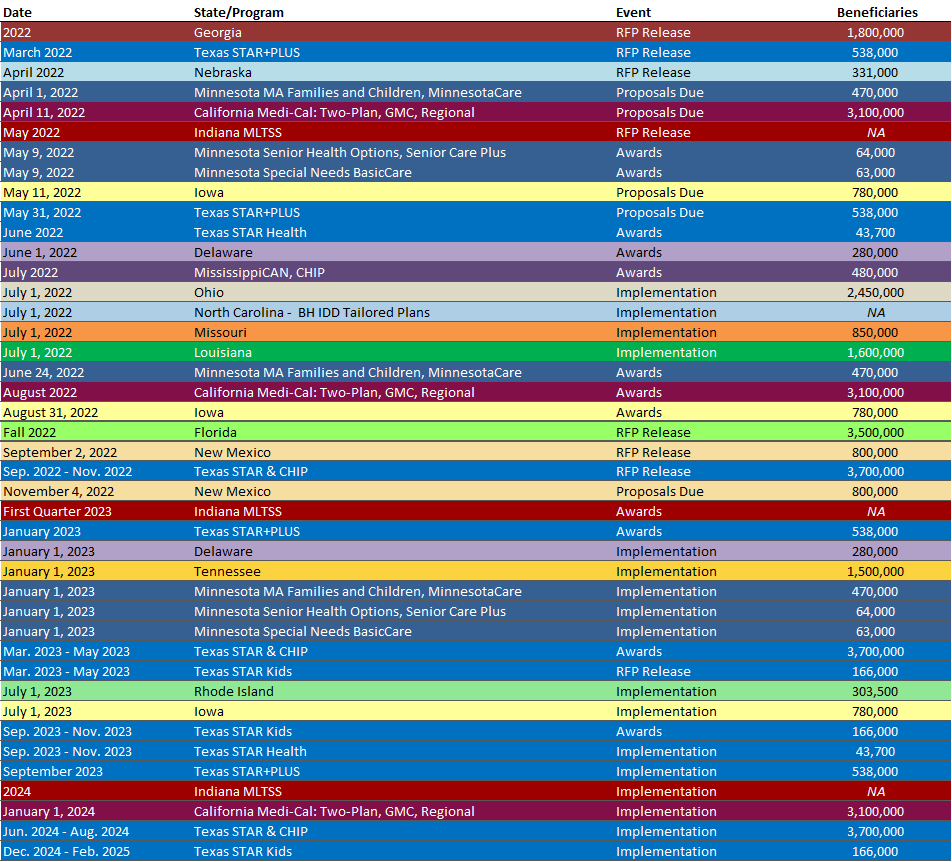
RFP Calendar
HMA News & Events
Leavitt Partners Webinar Replay: Ending Medicaid Continuous Eligibility – What Stakeholders Can Do Now to Minimize Coverage Losses. During this webinar, Medicaid experts from HMA and Leavitt Partners, an HMA Company, shared actionable steps you can take now to prepare for the end of the Public Health Emergency and minimize the number of eligible individuals who lose coverage. Listen now
New this week on HMA Information Services (HMAIS):
Medicaid Data
- California Medi-Cal Managed Care Enrollment Procurement Roadmap, Feb-22 Data
- Indiana Medicaid Managed Care Enrollment Is Up 1.4%, Jan-22 Data
- Minnesota Medicaid Managed Care Enrollment is Up 1.5%, Feb-22 Data
- Minnesota Medicaid Managed Care Enrollment is Up 2.1%, Mar-22 Data
- Nevada Medicaid Managed Care Enrollment is Up 11.4%, Oct-21 Data
- Ohio Medicaid Managed Care Enrollment is Up 7.5%, 2021 Data
- Virginia Medicaid Managed Care Enrollment is Up 10.4%, Sep-21 Data
- Virginia Medicaid MLTSS Enrollment is Up 5.4%, Sep-21 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Actuarial Services RFP, Mar-22
- Hawaii HCBS Provider Monitoring RFP, Mar-22
- Hawaii Kōkua Services for the Med-QUEST Program RFP, Mar-22
- New Mexico Medicare Improvements for Patients and Providers Act (MIPPA) Contracts, 2016-22
- Virginia Service Authorization and Specialty Services RFP, Mar-22
Medicaid Program Reports, Data and Updates:
- Georgia Medical Care Advisory Committee Meetings, 2021
- Iowa Plan for HCBS Implementation of the American Rescue Plan Act, 2021-22
- Nebraska Medicaid Annual Reports, SFY 2013-21
- Nevada External Quality Review Technical Reports, SFY 2014-21
- Nevada Medicaid Dental Dashboards, FY 2018-21
- Nevada Medicaid Managed Care Compliance Reports, SFY 2020-21
- Nevada Medicaid Managed Care Network Adequacy Validation Reports, FY 2020-21
- Ohio OhioRISE Advisory Council Meeting Materials, 2020-22
- Pennsylvania HealthChoices Behavioral Health Rate Development and Certifications, 2019-22
- Pennsylvania HealthChoices Physical Health Rate Development and Certification, CY 2019-22
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Mar-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
About HMA
HMA is an independent, national research and consulting firm specializing in publicly funded healthcare and human services policy, programs, financing, and evaluation. We serve government, public and private providers, health systems, health plans, community-based organizations, institutional investors, foundations, and associations. Every client matters. Every client gets our best. With more than 20 offices and over 500 multidisciplinary consultants coast to coast, our expertise, our services, and our team are always within client reach.
Among other services, HMA provides generalized information, analysis, and business consultation services to investment professionals; however, HMA is not a registered broker-dealer or investment adviser firm. HMA does not provide advice as to the value of securities or the advisability of investing in, purchasing, or selling particular securities. Research and analysis prepared by HMA on behalf of any particular client is independent of and not influenced by the interests of other clients.
