HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Innovation Center Announces ACO PC Flex Model to Improve Access for Medicare Beneficiaries

- Introducing HMA's New Podcast: Vital Viewpoints on Healthcare

- Alaska Receives Extension for Behavioral Health Reform 1115 Demonstration

- California Approves Proposition 1 to Provide Funding Addressing Homelessness Crisis, Substance Misuse

- Florida Governor Signs Legislative Package Aimed at Boosting Healthcare Workforce, Access

- Georgia Submits Section 1115 Waiver Amendment for Personal Care Services

- Maryland Submits Section 1115 Waiver Amendment for Pre-release Services

- Maryland Submits AHEAD Model Application to CMS

- Nebraska Legislature Passes Provider Tax Bill to Increase Medicaid Hospital Payment Rates

- New York Announces RFP For Development of 13 Certified Community Behavioral Health Clinics

- New York Governor Allocates $102 Million to Fund New Mental Health Care Programs

- Rhode Island Senate Considers Bill to Establish a Prescription Drug Affordability Board

- Rhode Island Receives CMS Approval for 1115 Waiver Amendment Permitting HCBS in Acute Hospital Settings

- Vermont Submits AHEAD Model Application to CMS

- Virginia Rescinds Notice of Intent to Award for Statewide Medicaid Managed Care Procurement

- Biden Administration Issues Final Rule to Streamline Medicaid, CHIP Enrollment

- HHS Announces Lower Coinsurance Rate for 41 Medicare Part B Drugs

- CMS Signals New Guidance on Medicare Part D Coverage of Obesity Drugs

- Kaiser, Town Hall Ventures Launch PACE Joint Venture

- United/Optum to Acquire Steward Health Care’s Physician Network

In Focus
CMS Innovation Center Announces ACO PC Flex Model to Improve Access for Medicare Beneficiaries
This week, our In Focus section looks at the voluntary Accountable Care Organization Primary Care Flex (ACO PC Flex) Model, which the Centers for Medicare & Medicaid Services (CMS) Innovation Center announced on March 19, 2024. This model is designed to increase the number of low revenue ACOs in the Medicare Shared Savings Program (MSSP). Model participants will receive a one-time advanced shared savings payment and monthly prospective population-based payments. The ACO PC Flex Model is intended aims to support care delivery transformation, innovation, and team-based approaches to improve quality and reduce costs of care.
The ACO PC Flex Model is structured to increase the number of low revenue ACOs (i.e., ACOs composed of physicians, a small hospital, and/or serve rural areas). CMS published results in August 2022 indicating that low revenue ACOs generated $113 more per capita savings than their high revenue counterparts. CMS wrote in July of 2023 that the agency was seeking new opportunities for ACOs to serve Medicare beneficiaries. With this model, the Innovation Center is providing flexible payment to support innovative, team-based, person-centered, and proactive approaches to care for a subset of ACOs that have historically generated savings.
ACO PC Flex Model payments are structured to provide advanced shared savings to support administrative activities necessary for the model and ongoing payments specifically for primary care. The payment approach includes:
- A monthly prospective primary care payment consisting of 1) a county base rate determined by average primary care spending, and 2) payment enhancements to support increased access to primary care, provision of care, and care coordination, which are exempt from CMS recoupment
- An advanced shared savings payment as a one-time advance the changes needed to support needed operations and administration
With the approach, the Innovation Center anticipates CMS will be able to improve access to primary care services, particularly for underserved communities, and empower providers through flexible, stable payments to innovate care delivery to better meet their patients’ needs.
The demonstration will start January 1, 2025, and run for five years. The request for applicants (RFA) is expected in the second quarter of 2024, and ACOs must apply for participation in MSSP as a new or renewing organization to be eligible for ACO PC Flex. Applications for MSSP close June 17, 2024.
More details are expected to be included in the RFA. If you are interested learning more about the ACO PC Flex Model, please contact Amy Bassano and Melissa Mannon.
Introducing HMA's New Podcast: Vital Viewpoints on Healthcare
HMA is excited to announce the launch of our new podcast, Vital Viewpoints on Healthcare, featuring provocative conversations with the healthcare industry’s premier experts. What does it mean to be an expert, and what value does that bring to clients? Expertise comes from experience, learning, training, and a curiosity about how to solve the toughest problems. Our new podcast showcases our experts in that light, exploring how their journey has informed their approach and their point of view on some of the thornier problems affecting the industry. Today we released the first 4 episodes:
- Why is behavioral health so hard to fix? featuring Dr. Gina Lasky
- What would it take to make the ACA more affordable? featuring Liz Wroe
- Can continuous quality improvement transform healthcare equity? featuring Leticia Reyes-Nash
- Is food the missing link in healthcare’s cost crisis? featuring R.J. Briscione
Future episodes will be released on the 4th Wednesday of each month; upcoming episodes will feature experts in children’s behavioral health, value-based care, addiction and harm reduction, payment and pricing, healthcare data and technology, and more. Please remember to listen, like, and subscribe, wherever you get your podcasts. And, if you enjoy what you hear, help us spread the word to others who might be interested.
HMA Roundup
Alaska
Alaska Receives Extension for Behavioral Health Reform 1115 Demonstration. The Centers for Medicare & Medicaid Services (CMS) announced on March 26, 2024, that it has approved Alaska’s section 1115 demonstration extension, retitled as “Behavioral Health Reform”. The demonstration extension does not include any changes, instead just continues its existing authorities which include allowing the state to receive federal financial participation for providing substance use disorder (SUD) treatment services for short-term residents in settings that qualify as an institution for mental diseases and provides expanded services for those with serious mental illness, severe emotional disturbance, and SUDs. The extension approval is effective March 26, 2024, through December 31, 2028. Read More
California
California Approves Proposition 1 to Provide Funding Addressing Homelessness Crisis, Substance Misuse. The Los Angeles Times reported on March 20, 2024, that California voters approved Proposition 1, which provides a $6.4 billion bond to support 10,000 substance use disorder treatment and housing beds. It also alters an existing mental health services tax to fund treatment for drug addiction. The proposition furthers Governor Gavin Newsom’s efforts to address the state’s homelessness crisis. Read More
Colorado
Colorado Medicaid Program Takes Steps to Prevent Termination Amid Technological, Structural Issues. The Colorado Sun reported on March 22, 2024, that the Colorado Department of Health Care Policy and Financing sent a memo to Medicaid recipients that detailed several actions aimed at preventing individuals from losing services due to computer or paperwork issues. Officials noted that they will assist counties in reviewing terminations, process a backlog of claims, and pause terminations for two months after a recipient’s benefits are set to expire. The Department sent the memo after the Colorado Center on Law and Policy and the National Health Law Program filed a complaint against Colorado Medicaid, alleging that the program violated the rights of beneficiaries with disabilities, and requested that several federal agencies intervene to pause the state’s termination of coverage for beneficiaries with disabilities. The named federal agencies, the U.S. Department of Health and Human Services Office for Civil Rights and the U.S. Department of Justice, have not officially responded. Read More
Florida
Florida Governor Signs Legislative Package Aimed at Boosting Healthcare Workforce, Access. The Tampa Bay Times reported on March 21, 2024, that Florida Governor Ron DeSantis signed four of the six bills that comprise the $1.1 billion “Live Healthy” legislative package, which aims to boost the state’s healthcare workforce, improve access to mental and maternal health, and ease the process of shopping for care. Although the package expands access to free and low-cost primary care and testing clinics, it does not expand coverage to other services for uninsured individuals. Read More
Georgia
Georgia Submits Section 1115 Waiver Amendment for Personal Care Services. The Centers for Medicare & Medicaid Services (CMS) announced on March 27, 2024, that Georgia has submitted an amendment for the Planning for Healthy Babies Medicaid Section 1115 demonstration waiver aimed at addressing workforce shortages by allowing individuals to be reimbursed for medically necessary personal care services. Services must be rendered to medically fragile members under age 21 enrolled in the Georgia Pediatric Program. The Planning for Healthy Babies demonstration provides family planning and inter-pregnancy care services, including primary care and primary care case management, for eligible women. Public comments will be accepted through April 26. Read More
Georgia Senate Committee Rejects Private Option Medicaid Expansion Bill. The Georgia Recorder reported on March 22, 2024, that the Georgia Senate Regulated Industries and Utilities Committee rejected a bill that would have allowed the state to obtain a waiver from the federal government to implement a “private option” expansion program called PeachCare Plus. Separately, the committee approved a bill that would scale back certificate-of-need regulations and form a comprehensive health coverage commission, which now heads to Governor Brian Kemp for his signature. Read More
Illinois
Illinois House Committee Advances Bill to Ban Step Therapy. Health News Illinois reported on March 22, 2024, that the Illinois House Human Services Committee has advanced a bill that would ban short-term, limited duration health plans, prior authorization requirements for inpatient mental healthcare, and the use of “step therapy” in prescription drug coverage. Under the bill, insurers will also be required to submit updated in-network care directories to ensure compliance with network adequacy and transparency standards. The bill now moves to the full House for further consideration. Read More
Kansas
Kansas House, Senate Hold Hearings on Medicaid Expansion. The Kansas Reflector reported on March 20, 2024, that the Kansas House and Senate separately held hearings to discuss the advantages and disadvantages of Medicaid expansion, marking the first time in four years that legislators have permitted hearings on the subject. The House Health and Human Services Committee hearing focused on House Bill 2556, and Committee Chair Rep. Brenda Landwehr (R-Wichita) indicated the committee may take action on the bill in the coming days. Read More
House Approves Funding that Would Shorten Waitlists for IDD, PD Medicaid Waivers. 13 WIBW reported on March 20, 2024, that the Kansas House agreed to include $34.6 million in its state budget proposal to eliminate 500 slots from the Intellectually and Developmentally Disabled (IDD) and Physically Disabled (PD) Medicaid waiver waitlists. The measure would also cap the IDD waitlist at 4,800 and the PD waitlist at 2,000. The Senate agreed to eliminate 250 slots from the waitlists. The chambers will next convene to discuss a compromise. Read More
Maryland
Maryland Submits Section 1115 Waiver Amendment for Pre-release Services. The Centers for Medicare & Medicaid Services announced on March 22, 2024, that Maryland has submitted a Section 1115 waiver amendment requesting coverage of pre-release services to incarcerated individuals who have substance use disorder or a serious mental illness through the state’s HealthChoice Medicaid program. Public comments are open through April 21, 2024.
Maryland Submits AHEAD Model Application to CMS. Maryland Matters reported on March 20, 2024, that Maryland submitted an application for the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) model to the Centers for Medicare & Medicaid Services (CMS), which comes in advance of the state’s total cost of care model expiring in December 2026. The AHEAD model will fund health quality, health equity, and health outcome initiatives. CMS plans to select up to five states in the first cohort of the program. If selected, Maryland will undergo an 18-month negotiation process and transition to the AHEAD model as early as January 2026. Read More
Massachusetts
Massachusetts Attorney Files Petition Over UnitedHealth’s Alleged False Medicaid Claims in Dual Eligible Program. Bloomberg Law reported on March 21, 2024, that Massachusetts attorney general Andrea Campbell is requesting that a state court compel UnitedHealthcare to comply with the state’s False Claims Act investigation, which includes providing documentation that was requested in July 2023. UnitedHealthcare has allegedly improperly inflated care levels for its Senior Care Options dual program in order to receive increased capitated payments. The judge hearing the motion is expected to rule within the next few months. Read More
Medicaid Acute Care Hospitals to Receive Up to $400 Million Annually for HRSN Initiatives. Modern Healthcare reported on March 21, 2024, that Massachusetts private acute care hospitals are working toward earning Medicaid incentives from a $400 million annual pool by assessing health disparities and addressing health related social needs (HRSN). The incentive program is authorized through a Section 1115 demonstration waiver, and expectations for earning the incentive payments will increase over time. The waiver, approved in 2012, authorizes $2.2 billion in Medicaid funding, with an additional $875 million through a hospital tax. In 2023, all acute care hospitals in the state met the requirements to receive incentive payments through the program. Read More
Nebraska
Nebraska Legislature Passes Provider Tax Bill to Increase Medicaid Hospital Payment Rates. The Wahoo Newspaper reported on March 25, 2024, that the Nebraska Legislature passed a bill, sponsored by Senator Mike Jacobson (R-North Platte) and 19 co-sponsors, that could garner more than $1.4 billion in federal funding to raise Medicaid payment rates for inpatient and outpatient hospital care beginning July 1. The bill would require hospitals to pay an assessment of up to 6 percent of net patient revenue, which would serve as the match for federal funding. The bill, intended to reduce hospital closures, now moves to the Governor for signature. Read More
New York
New York Announces RFP For Development of 13 Certified Community Behavioral Health Clinics. The New York State Office of Mental Health, Office of Addiction Services and Supports, and the Department of Health, released in March 2024, a request for proposals (RFP) for the development of 13 new Certified Community Behavioral Health Clinics (CCBHCs) to operate within ten economic development regions to further develop an integrated behavioral health treatment system. Each awardee will implement the full CCBHC model, including all nine required behavioral health services. Awarded agencies will receive one-time startup funds in the amount of $265,000 which must be spent by June 30, 2026. Letters of intent are due May 30, with proposals due by July 1. Awards are expected August 7. The contract start date is October 1, 2024, with CCBHCs to be operational July 1, 2025. Read More
Governor Allocates $102 Million to Fund New Mental Health Care Programs. Crain’s New York Business reported on March 25, 2024, that New York Governor Kathy Hochul allocated $102 million to fund outpatient care programs for individuals with complex mental illness, including $92 million to support Critical Intervention Teams, a new program that aims to reduce hospital admissions, visits to emergency rooms, and standardize behavioral health hospitalizations. The remaining $10 million will support the expansion of 26 care teams serving unhoused youth in New York City. Read More
Comptroller’s Office Requests Additional Medicaid Auditor Staff in Revised Budget Request. Crain’s New York Business reported on March 25, 2024, that the New York State Comptroller’s Office updated its budget request to ask for an additional $5 million to hire 10 additional Medicaid auditors. The office noted that the program produces more than a $400 return on investment for each dollar spent as justification for the request. The governor’s office has not indicated if it will include the request in its final budget. Read More
Ohio
Ohio Medicaid Enrolled More than 124,000 Individuals Enrolled in Another State’s Program, Audit Finds. The Columbus Dispatch reported on March 26, 2024, that more than 124,000 people were simultaneously enrolled in Ohio’s Medicaid program and the Medicaid program of at least one other state, according to a report from Ohio State Auditor Keith Farber. The report, which examines data from 2019 through 2022, found that Ohio spent over $1 billion in payments for individuals also enrolled in another state’s Medicaid program. The report recommends that the Ohio Department of Medicaid utilize more technology during the enrollment process, include questions to determine residency of applicants, and implement a system to identify individuals enrolled in another state’s Medicaid program. The Department of Medicaid indicated that it has not been able to confirm the findings of the report and noted that the report does not account for increased requirements to maintain Medicaid enrollment during the pandemic. Read More
Oregon
Oregon to Utilize Tech Platform to Streamline CBO Payments for New HRSN Initiative. Technology provider Unite Us announced on March 26, 2024, that Oregon’s nine Medicaid Coordinated Care Organizations (CCOs) will adopt the company’s scalable payments solution to implement the newly launched health-related social needs (HRSNs) benefit under the state’s Section 1115 waiver demonstration. The platform will enable reimbursement for community-based organizations (CBOs) at scale for services rendered, while also measuring the success of social care funding initiatives. Read More
Puerto Rico
Puerto Rico Medicare Advantage Plans Questioned on High Supplemental Benefits Spending. Health Payer Specialist reported on March 25, 2024, that U.S. Department of Health and Human Services (HHS) Secretary Xavier Becerra has sent a letter to Puerto Rico Medicare Advantage (MA) plans requesting detailed financial data regarding payments made to hospitals and healthcare providers, as well as information on supplemental benefits expenses. The letter indicated concerns around MA plans using federal payments to expand its supplemental benefits, rather than increasing provider reimbursements. Becerra stated that spending on supplemental benefits is higher than in any other state. The MA plans include Elevance Health, MHH Healthcare, Guidewell/Florida Blue, and Humana. Read More
Rhode Island
Rhode Island Senate Considers Bill to Establish a Prescription Drug Affordability Board. The Boston Globe reported on March 21, 2024, that Rhode Island Senator Alana DiMario (D-Narragansett) sponsored a bill that would establish a drug cost review commission to evaluate costs from manufacturers and consider imposing more affordable prices. The bill also requires more transparency from manufacturers and establishes an upper-payment limit. The bill was held in the Senate Health and Human Services committee for further study. Read More
Rhode Island Receives CMS Approval for 1115 Waiver Amendment Permitting HCBS in Acute Hospital Settings. The Centers for Medicare & Medicaid Services approved on March 21, 2023, Rhode Island’s request to amend the state’s section 1115 Rhode Island Comprehensive Demonstration to allow the provision of home and community-based personal care services in acute care hospital settings. The amendment additionally expands eligibility for waiver services for adults at risk for long-term care, includes updates reflecting the state’s approval of one-year Medicaid postpartum coverage, adds remote supports and monitoring as services, and expands education requirements for providers. The amendment is effective through the current demonstration expiration date of December 31, 2024. Read More
Vermont
Vermont Submits AHEAD Model Application to CMS. The VT Digger reported on March 27, 2024, that Vermont submitted an application for the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) model to the Centers for Medicare & Medicaid Services (CMS), which would fund health quality, health equity, and health outcome initiatives. CMS plans to select up to five states in the first cohort of the program, and each state would receive $12 million. Implementation of the program could begin as early as January 2026 and run for nine years. Vermont’s All-Payer Accountable Care Organization Model is currently set to expire at the end of 2024, though officials plan to extend the program for one year, which would align with the potential transition to the AHEAD model. Read More
Virginia
Virginia Rescinds Notice of Intent to Award for Statewide Medicaid Managed Care Procurement. The Virginia Department of Medical Assistance Services (DMAS) announced on March 19, 2024, that it is withdrawing the Notice of Intent to Award (NOIA) for the Cardinal Care Medicaid managed care program procurement. The NOIA, released in February, named incumbents CVS/Aetna, Elevance/Anthem, Sentara/Optima Health, United Healthcare, and non-incumbent Humana, as awardees. The NOIA is under review, and a new NOIA will be posted in the coming days. The contract, currently set to begin on July 1, 2024, will run for six-years with two two-year renewal options.
National
Biden Administration Issues Final Rule to Streamline Medicaid, CHIP Enrollment. The Centers for Medicare & Medicaid Services (CMS) announced on March 27, 2024, that the Biden Administration has issued a final rule aimed at streamlining and removing barriers for Medicaid and Children’s Health Insurance Program (CHIP) enrollment and renewals. Provisions under the final rule include eliminating limits and waiting periods for CHIP coverage; prohibiting locking children out of CHIP coverage if a family is unable to pay premiums; prohibiting states from conducting renewals more frequently than every 12 months; and providing a minimum 90-day reconsideration period after procedural terminations. Read More
GAO Finds Over $100 Billion in Improper Medicaid, Medicare Payments in Fiscal 2023. U.S Government Accountability Office (GAO) announced on March 26, 2024, that the federal government has made an estimated $236 billion in payment errors during fiscal 2023, including $50.3 billion under Medicaid and $51.1 billion under Medicare. Improper payments in Medicaid have decreased by $30 billion when compared to fiscal 2022. The GAO has recommended that Medicaid improve oversight of claims paid to ineligible medical providers with suspended or revoked licenses and that Medicare improve communication around its prior authorization program . Read More
HHS Announces Lower Coinsurance Rate for 41 Medicare Part B Drugs. The U.S. Department of Health and Human Services (HHS) announced on March 26, 2024, that 41 drugs available through Medicare Part B will have a lower coinsurance rate between April 1 and June 30 if respective drug companies raise prices faster than the rate of inflation. Drug companies are required to pay rebates when prices increase faster than inflation rates under the Inflation Reduction Act. Approximately 763,700 Medicare beneficiaries use one or more of the 41 drugs. Rebates are expected to save individuals between $1 and $3,575 per dose depending on individual coverage. Read More
House Advances Fiscal 2024 Spending Package With Additional Funding for Health Centers, Key Health Programs. CBS News reported on March 22, 2024, that the U.S. House of Representatives passed a $1.2 trillion fiscal 2024 spending package, which covers about 70 percent of the federal government, and includes $117 billion for Health and Human Services Department operations. Specifically, the package would allocate an additional $1.9 billion for community health centers, as well as $1.4 billion for health professions workforce development, $4.6 billion for substance use disorder prevention and treatment, and $1.2 billion for maternal and child health programs. The package also provides $9.2 billion for the Centers for Disease Control, $46.8 billion for the National Institutes of Health, and a one-year extension of the President’s Emergency Plan for AIDS Relief. The budget now moves to the Senate. Read More
CMS Signals New Guidance on Medicare Part D Coverage of Obesity Drugs. Fierce Healthcare reported on March 21, 2024, that the Centers for Medicare & Medicaid Services (CMS) is expected to allow Medicare Part D to cover obesity drugs for medically accepted uses. Under the guidance, the Medicare Part D program will cover obesity drugs (GLP-1s) when the drugs are approved for other indications. For example, Novo Nordisk’s Wegovy is approved by the Food and Drug Administration to reduce risk of stroke or heart attack in people with cardiovascular disease and a body mass index over a certain threshold. The forthcoming CMS decision could pave the way for broader coverage of GLP-1s. Read More
HHS Releases New Reports Outlining ACA Marketplace Enrollment Trends. The U.S. Department of Health and Human Services (HHS) issued on March 22, 2024, four new reports outlining current enrollment trends within the Affordable Care Act (ACA) Marketplaces during its first ten years. Approximately 45 million individuals are enrolled through the Marketplaces and Medicaid expansion as of the 2024 open enrollment period, representing a 46 percent increase in enrollment compared to 2021. Additionally, an estimated 1.7 million Black individuals and 3.4 million Latino individuals are enrolled in Marketplace plans through HealthCare.gov during the 2023 open enrollment period, representing a 95 percent and 103 percent increase since 2020. Read More
Medicaid Disenrollments Exceed 18 Million Nationwide. Health Payer Intelligence reported on March 25, 2024, that more than 18 million Medicaid beneficiaries have been disenrolled nationwide since eligibility redeterminations resumed in April 2023. The majority of disenrollments were due to procedural reasons while more than 35 million beneficiaries’ eligibility redeterminations have either not been completed or have not been reported. Read More
Industry News
Kaiser, Town Hall Ventures Launch PACE Joint Venture. Modern Healthcare announced on March 27, 2024, that Kaiser Permanente and healthcare investment firm Town Hall Ventures launched a joint venture, Habitat Health, that will provide services through the Program of All-Inclusive Care for the Elderly (PACE). The first two PACE programs will launch in Los Angeles and Sacramento in 2025. Neither company disclosed financial details of the venture. Read More
United/Optum to Acquire Steward Health Care’s Physician Network. Modern Healthcare reported March 26, 2024, that UnitedHealth’s Optum subsidiary has submitted a regulatory filing with the Massachusetts Health Policy Commission to acquire Dallas-based health system Steward Health Care’s physician group, Stewardship Health, which spans across nine states. Under the proposed transaction, Optum would acquire all of the issued and outstanding stock of Stewardship Health. The Health Policy Commission will have 30 days to assess the potential impact of an Optum-Steward transaction. Read More
UnitedHealth Group Begins Processing Medical Claims Backlog, Resumes Software Services. Reuters reported on March 22, 2024, that UnitedHealth Group’s Change Healthcare unit will resume operations for some software services, including the processing of a medical claims backlog of more than $14 billion following a cyberattack last month. The company has increased financial assistance to providers affected by the incident from $2 billion to $2.5 billion and extended the repayment period to 45 days. The company indicated that Assurance, its software for preparing medical claims, is back online while its largest clearinghouse, Relay Exchange, will resume operations the weekend of March 23. Read More
BrightSpring Finalizes Acquisitions in Maryland, Michigan, Montana. BrightSpring Health Services, a provider of home and community-based services, announced on March 26, 2024, the acquisition of a home health operation in Maryland, a behavioral therapy company in Michigan, and a long-term care pharmacy in Montana. The Maryland acquisition is effective January 1; the Michigan acquisition, consisting of the remaining 30 percent equity interest, is effective March 1; and the Montana acquisition of a pharmacy serving assisted living facilities, group homes, and mental health patients, is effective March 19. Read More
Sila Realty Trust Acquires Five Arizona, Texas Healthcare Properties Leased by Tenet in $85.5 Million Deal. Modern Healthcare reported on March 22, 2024, that Sila Realty Trust has acquired five healthcare properties leased by Tenet Healthcare in Arizona and Texas in a $85.5 million transaction. The facilities include four micro-hospitals, each with eight inpatient beds and a 13-bed emergency department, and a freestanding emergency department containing 13 beds. The seller was not disclosed. Read More
Best Life Brands Acquires Home Access Solutions Provider Next Day Access. Home Health Care News reported on March 25, 2024, that Michigan-based Best Life Brands has acquired Next Day Access, a provider of residential and commercial home access solutions. Best Life Brands had more than 600 franchise locations in the U.S. and Canada prior to the acquisition. Read More
Healthly Invests in Access Senior Healthcare. Healthly announced on March 25, 2024, that it has invested in Access Senior Healthcare, a California restricted licensure health plan, to provide value-based economics across 10 health plan partners. Access Senior Healthcare serves more than 175 primary care physicians and 700 specialists in California. The chief executives of Healthly and Access Senior Healthcare will each maintain their respective positions. Healthly has also entered into a management services agreement with Access Medical IPA and Access Santa Monica, two independent physician associations. Read More
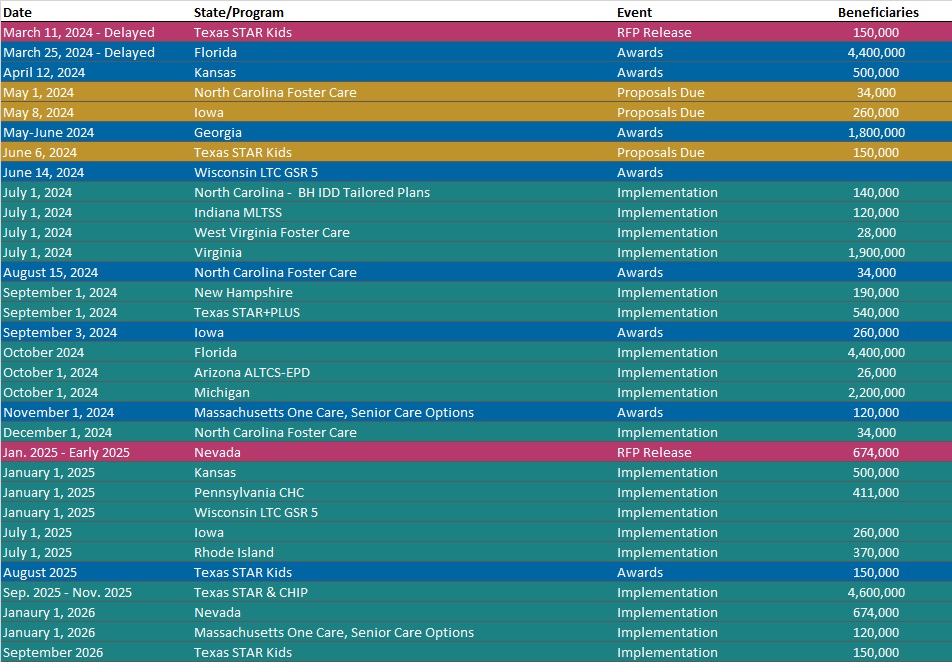
RFP Calendar
HMA News & Events
HMA Webinar:
Substance Use Disorder (SUD) Ecosystem of Care: Empowering Change in the SUD Ecosystem. Wednesday, April 10, 2024, 12 PM ET. Join us for part 2 in our webinar series “Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives.” As covered in the first webinar, we have an imperative to think and act differently to change the trajectory of not just the long-standing opioid epidemic, but other existing and emerging harmful substance use and addiction. Grounded in equity, empowering change in the SUD ecosystem requires person-centered and community driven approaches to respond to individual wants and needs. We must meet each person where they are as well as consider how the ecosystem of each community can be leveraged to drive change. Register Here
Leavitt Partners, an HMA company, Webinar:
The Future of Medicare Advantage Supplemental Benefits. Thursday, April 4, 2024, 12 PM ET. More than 30 million Americans are enrolled in MA plans and more than half of Medicare-eligible beneficiaries participate in the program—a number that was less than 30 percent just a decade ago. One reason Medicare beneficiaries opt to participate in MA plans is the ability to offer supplemental benefits, including dental, vision, hearing, transportation services, OTC items, an in-home support services. Initially limited to a core set of offerings, over the years, MA supplemental benefits have undergone significant changes that have led to a broader range of allowable benefits, an expansion of how benefits can be targeted, and, growth in the number of plans offering such benefits. Register Here
