HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Medicare Drug Negotiation Guidance: What You Need to Know

- Medicaid Expansion News: Alabama, Kansas, Mississippi, North Carolina

- Arkansas Assisted Living Providers Struggle Financially After Medicaid Reimbursement Rate Increases are Delayed

- California Expands Availability of Medi-Medi Plans for Dual Eligibles to Five More Counties

- California Seeks Federal Approval of Program Covering 6 Months of Rent for Homeless Medi-Cal Beneficiaries

- Redeterminations News: California, Illinois, Rhode Island

- Idaho House Rejects $4.7 Billion Fiscal 2024 Medicaid Budget

- Kentucky Governor Signs Legislation to Increase Medicaid Rates for Outpatient Procedures

- New York Senate Advances Proposal to Repeal Medicaid Managed Care Pharmacy Carve-out

- Most States Will Take 12-14 Months to Process Medicaid Redeterminations, KFF Survey Says

- PurposeCare Acquires Home Sweet Home

In Focus
Medicare Drug Negotiation Guidance: What You Need to Know
This week our In Focus section reviews the Centers for Medicare and Medicaid Services’ (CMS) announcement of initial guidance for the new Medicare Drug Price Negotiation Program for 2026. This initial guidance is one of many steps CMS described in the Medicare Drug Price Negotiation Program timeline for the first year of negotiation.
The Drug Price Negotiation Program was approved as part of the Inflation Reduction Act (IRA) (P.L. 117- 169) in August 2022. As discussed in our previous In Focus, the IRA includes several other policies aimed at addressing cost, affordability and access to prescription drugs within the Medicare program.
The Drug Negotiation Program allows the U.S. Department of Health and Human Services (HHS) to negotiate maximum fair prices (MFPs) for Part D drugs. Negotiations between HHS and prescription drug manufactures will begin in 2023 and continue into 2024 before negotiated prices go into effect Jan. 1, 2026.
For Medicare payment in 2026, HHS can negotiate prices for up to 10 Part D drugs that do not have generic or biosimilar competition. CMS can increase the number of Part D drugs selected for price negotiation each subsequent year. Starting in 2028, the agency can annually add up to 20 new Part B or Part D drugs to the program.
The published guidance describes CMS’ approach for identifying the drugs selected for the initial year of the program. However, CMS is finalizing these policies as announced for the initial drug negotiation year.
The initial guidance also details the requirements and procedures for implementing the process for the first set of negotiations. For example, the guidance details aspects related to the offer-counter-offer exchange process, confidentiality terms following an agreement, penalties for violations, and the dispute resolution process.
Key Considerations
The drug negotiation program presents numerous operational and policy questions for CMS, manufacturers, and the healthcare sector broadly. The program is expected to have a direct impact on prices and affordability for the Medicare program and its beneficiaries. Additionally, other public and commercial payers will want to consider the potential downstream impacts on their costs. Ongoing monitoring of HHS’ implantation of the drug negotiation program and the pharmaceutical industry’s response to the drug negotiation program will help health plans, providers, and other interested stakeholders navigate this new landscape.
What’s Next
In the short-run, CMS will benefit from feedback from stakeholders about the outstanding policy and operational issues the agency has identified. Comments can be submitted until April 14, 2023
CMS anticipates issuing revised guidance for the first year of negotiation in Summer 2023. By September 1, 2023, CMS plans to publish the first 10 Part D drugs selected for the initial program year. The negotiated maximum fair prices for these drugs will be published by September 1, 2024 and prices will be in effect starting January 1, 2026.
HMA and HMA companies will continue to analyze this and subsequent guidance. We have analytical capabilities and expertise to assist with tailored analysis for manufacturers, providers, patient groups, health plans, and other stakeholders. HMA has the ability to model policy impacts of the drug negotiation program, support the drafting of feedback to CMS as the program is designed and implemented, and provide technical assistance in considering how this new program may interact with other Medicare and Medicaid initiatives.
If you have questions about the Drug Negotiation Program or other aspects of the Inflation Reduction Act and how it will affect manufacturers, Medicare providers, Medicaid programs and patients, contact Kevin Kirby ([email protected]), Amy Bassano ([email protected]) or Andrea Maresca ([email protected]).
HMA Roundup
Alabama
Advocates Push for Medicaid Expansion. The Alabama Political Reporter reported on March 20, 2023, that Cover Alabama, an alliance of advocacy groups, plans to rally at the Alabama State Capitol Tuesday to push lawmakers to expand Medicaid. An estimated 280,000 Alabamans would benefit from expansion. Read More
Arkansas
Arkansas Assisted Living Providers Struggle Financially After Medicaid Reimbursement Rate Increases are Delayed. McKnight’s Senior Living reported on March 20, 2023, that assisted living providers in Arkansas are struggling financially after Governor Sarah Huckabee Sanders delayed increases to Medicaid reimbursement rates. The rates were established by the Department of Human Services and approved by lawmakers and the previous administration. Read More
California
California Expands Availability of Medi-Medi Plans for Dual Eligibles to Five More Counties. The California Department of Health Care Services announced on March 17, 2023, that it will expand the availability of Medi-Medi Plans for dual eligibles to five additional counties: Fresno, Kings, Madera, Sacramento, and Tulare, effective January 1, 2024. Medi-Medi Plans for dual eligibles are currently available in the state’s seven former Coordinated Care Initiative counties: Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Mateo, and Santa Clara. Medi-Medi is the name of California’s Medicare Advantage Exclusively Aligned Enrollment Dual Eligible Special Needs Plans (D-SNPs), which allow dual eligibles to enroll in a D-SNP for Medicare benefits and in a Medi-Cal managed care plan for Medicaid benefits both operated by the same parent organization. Read More
California Requests Flexibility on Medicaid Member Asset Limits During Redeterminations. The California Department of Health Care Services announced on March 17, 2023, the submission of a waiver flexibility request to make it easier for Non-Modified Adjusted Gross Income individuals to renew their Medi-Cal coverage during Medicaid redeterminations. The request would also allow individuals to remain covered until the state eliminates the asset limit on January 1, 2024. The state is requesting that the authority be retroactively effective from March 1, 2023, to December 31, 2023. Read More
California Seeks Federal Approval of Program Covering 6 Months of Rent for Homeless Medi-Cal Beneficiaries. Kaiser Health News reported on March 20, 2023, that California Governor Gavin Newsom is trying to get federal approval for a transitional rent program that would provide up to six months of rent for homeless Medi-Cal beneficiaries. Similar experimental programs in Oregon and Arizona have received federal approval. Read More
Idaho
House Rejects $4.7 Billion Fiscal 2024 Medicaid Budget. The Idaho Capital Sun reported on March 20, 2023, that the Idaho House rejected a proposed $4.7 billion fiscal 2024 Medicaid budget, which included funding for Medicaid expansion. The bill will need to be rewritten and passed out of the Joint Finance-Appropriations Committee before it moves to the House and Senate. Read More
Illinois
Illinois Launches Public Awareness Campaign Ahead of Medicaid Redeterminations. State of Reform reported on March 20, 2023, that the Illinois Department of Healthcare and Family Services (HFS) will launch a public awareness campaign to ensure Medicaid beneficiaries are ready for redeterminations. The campaign will include paid advertisements; print, digital, and broadcast communications; as well as grassroots outreach. HFS also created a toolkit to help providers and community organizations with outreach efforts. Read More
Kansas
Advocates Push for Medicaid Expansion. The Topeka Capital-Journal reported on March 15, 2023, that advocates in Kansas held a rally at the statehouse to urge the legislature to pass Medicaid expansion. Governor Laura Kelly included Medicaid expansion in her budget proposal, but Republican lawmakers oppose the legislation. A poll from fall 2022 by Fort Hays State University found that 72 percent of Kansans support expansion. Read More
Kentucky
Governor Signs Legislation to Increase Medicaid Rates for Outpatient Procedures. The Associated Press reported on March 20, 2023, that Kentucky Governor Andy Beshear signed legislation to expand the Medicaid Hospital Rate Improvement Program to include outpatient care, which will increase Medicaid payments for those procedures. Currently, the program only includes inpatient care. The bill is intended to help rural hospitals that are struggling financially. Read More
Maryland
House Passes Bill to Allow Medicaid Coverage of Additional Gender-affirming Procedures. HuffPost reported on March 18, 2023, that the Maryland House passed a bill that would allow Medicaid to cover additional gender-affirming procedures. Currently, the state’s Medicaid program only covers some gender-affirming care, including mental health services, hormone replacement therapy, and gender reassignment surgery for patients 18 and older who meet specific qualifications. The bill now moves to the Senate. Read More
Maryland to Maintain Medicaid Reimbursement Rates for Evaluation, Management Services. The Maryland Department of Health announced on March 20, 2023, that it will maintain current Medicaid reimbursement rates for evaluation and management (E&M) services. For the first time, Medicaid’s rates paid to physicians are more than Medicare for E&M visits, the state says. E&M services include routine medical examinations, counseling, and hospital visits. Read More
Mississippi
Governor Signs Postpartum Medicaid Extension Legislation. Mississippi Today reported on March 16, 2023, that Mississippi Governor Tate Reeves signed legislation to extend postpartum Medicaid coverage from 60 days to 12 months. More than two-thirds of births in Mississippi are covered by Medicaid. Read More
Mississippi Residents Express Support for Medicaid Expansion in Poll. Mississippi Today reported on March 15, 2023, that 75 percent of Mississippians support Medicaid expansion, according to a poll from Mississippi Today and the Sienna College Research Institute. The poll also found that 71 percent of Mississippians believe lawmakers should address the state’s hospital crisis with additional funding. Read More
New Hampshire
New Hampshire HCBS Providers to Leave CFI Program Unless State Increases Reimbursement Rates. The New Hampshire Bulletin reported on March 22, 2023, Ascentria Care Alliance and Waypoint of New Hampshire have indicated they will exit the state’s Choices for Independence (CFI) program unless reimbursement rates are increased. CFI is a Medicaid program covering in-home housekeeping and personal care services. The two organizations, which serve 600 individuals, are seeking rate increases well above New Hampshire Governor Chris Sununu’s proposed 3.1 percent increase. Read More
New York
Senate Advances Proposal to Repeal Medicaid Managed Care Pharmacy Carve-out. Crain’s New York reported on March 15, 2023, that the New York Senate advanced a proposal to repeal the upcoming Medicaid managed care pharmacy carve-out. The transition is currently set to begin on April 1 and was included in Governor Kathy Hochul’s budget proposal. Read More
North Carolina
Senate Approves Medicaid Expansion Bill. ABC11 reported on March 15, 2023, that the North Carolina Senate gave final approval to a Medicaid expansion bill. The bill also includes changes to hospital certificate of need rules. The bill now moves to the House. Read More
Oklahoma
Oklahoma Requests Postpartum Medicaid Coverage Extension through 1115 Waiver. The Centers for Medicare & Medicaid Services announced on March 16, 2023, that Oklahoma submitted a Medicaid 1115 waiver amendment request to extend postpartum SoonerCare coverage from 60 days to 12 months. The amendment also requests extending coverage to pregnant women who are within 185 percent of the federal poverty level instead of 133 percent. The federal comment period is open until April 16. Read More
Oregon
Oregon to Begin Continuous Medicaid Enrollment for Children Under 6 in May. Kaiser Health News reported on March 17, 2023, that Oregon will begin continuous Medicaid enrollment for children from birth to six years old in May through a Medicaid 1115 waiver. The waiver received federal approval in September 2022. Oregon is the first state to receive federal approval, but California, New Mexico, and Washington are working on similar policies. Read More
Rhode Island
Rhode Island Expects Half of Medicaid Renewals to Be Passive. Rhode Island Governor Dan McKee announced on March 16, 2023, that the state expects about half of Medicaid renewals to be passive and require no action from the enrollee. The state is working with community partners and advocates to conduct outreach efforts ahead of eligibility redeterminations. The state is also offering mini grants to community partners to reach those most at risk during the renewal process. Read More
Texas
Representative Files Bill to Extend Postpartum Medicaid Coverage. NBC DFW reported on March 17, 2023, that Texas Representative Toni Rose (D-Dallas) filed a bill to extend postpartum Medicaid coverage from 60 days to 12 months. The bill was heard by the House Health Care Reform Select Committee, who will decide whether or not to advance it for a full House vote. Read More
National
HHS Issues Initial Guidance on Medicare Drug Price Negotiation Program. The U.S. Department of Health and Human Services (HHS) issued on March 15, 2023, initial guidance detailing key requirements and parameters for the new Medicare Drug Price Negotiation Program, which will begin on January 1, 2026. The Centers for Medicare & Medicaid Services is looking to publish a list of the first 10 Medicare Part D drugs in the program by September 1, 2023, and have negotiated maximum fair prices for those drugs to be published by September 1, 2024. Prices will be effective in 2026. Public comments will be accepted until April 14. Read More
Medicaid Expansion Reduced Racial Gaps in Health Coverage, Report Finds. Yahoo Finance reported on March 18, 2023, that Medicaid expansion has reduced racial gaps in health insurance coverage, according to a report from the Commonwealth Fund. The report found that before Medicaid expansion went into effect, 40.2 percent of the Hispanic/Latino population, 24.4 percent of the Black population, and 14.5 percent of the white population were uninsured, with those numbers falling to 24.5 percent, 13.5 percent, and 8.2 percent, respectively in 2021. Read More
Most States Will Take 12-14 Months to Process Medicaid Redeterminations, KFF Survey Says. Kaiser Family Foundation (KFF) reported on March 16, 2023, that 43 out of 49 states will take 12 to 14 months to complete the Medicaid redeterminations process and return to routine operations, according to a survey done by KFF and the Georgetown University Center for Children and Families. The survey also found that 43 states have continued to process ex parte renewals over the past year, and 27 have been flagging individuals who may no longer be eligible. A projected 18 percent of Medicaid beneficiaries will be disenrolled across the approximately one-third of responding states able to report estimates. Read More
SAMHSA Awards CCBHC Planning Grants to 15 States. Behavioral Health Business reported on March 21, 2023, that the Substance Abuse and Mental Health Services Administration (SAMHSA) awarded 15 states $1 million planning grants to help develop and apply for the Medicaid certified community behavioral health clinics (CCBHCs) demonstration. Ten will be able to join the demonstration in 2024 and the rest could join in 2026. Read More
U.S. Senators Introduce Bill to Expand Access to Dental, Vision, Hearing Services for Medicaid, Medicare Beneficiaries. U.S. Senator Bob Casey (D-PA) announced on March 16, 2023, the introduction of the Medicare and Medicaid Dental, Vision, and Hearing Benefit Act. The act will allow Medicare to cover dental, vision, and hearing benefits, and increases the federal Medicaid match to states to 90 percent for these optional services. Read More
Waivers Help Keep Individuals with Autism on Medicaid, Study Finds. Health Payer Intelligence reported on March 22, 2023, that adolescents with autism were more likely to remain enrolled in Medicaid into adulthood if their state has an autism spectrum disorder 1915(c) waiver, according to a JAMA Network study. The study used Medicaid data from 2008 to 2016 from 47 states and the District of Columbia. Read More
Industry News
MedArrive, Ouma to Offer Maternal TeleHealth Services to Medicaid Members. MHealth Intelligence reported on March 21, 2023, MedArrive and Ouma Health will jointly offer maternal telehealth services to Medicaid beneficiaries. MedArrive operates a mobile care management network. Ouma provides maternity telehealth services. Read More
PurposeCare Acquires Home Sweet Home. PurposeCare announced on March 21, 2023, the acquisition of Michigan-based Home Sweet Home, an independent home health care agency. PurposeCare provides home-based care services to dual eligibles. The acquisition will expand its services to an additional 400 patients and more than 300 caregivers. Read More
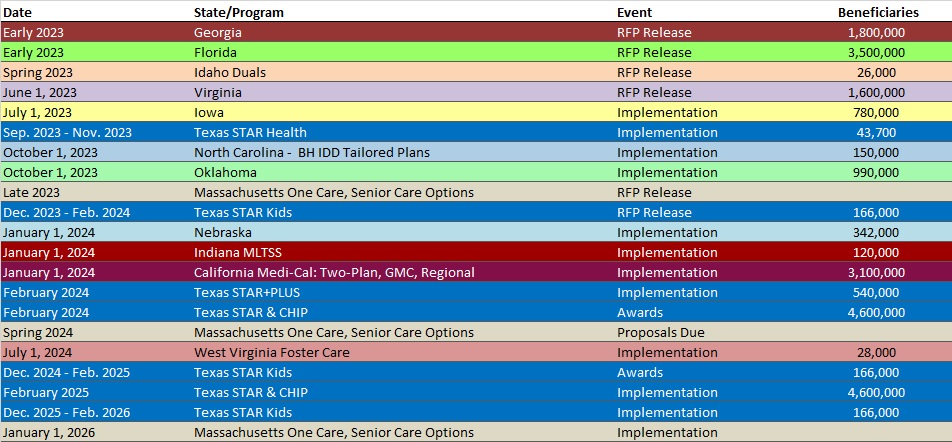
RFP Calendar
Company Announcements
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPERS
Proposed MA Risk Adjustment Model – Good News for Some, Detrimental for Others. On February 1, 2023, CMS released the 2024 Advance Notice, which details planned changes to the Part C and Part D capitation and risk adjustment methodology for calendar year (CY) 2024. As part of the Advance Notice, CMS is proposing to implement a revised version of the CMS-HCC risk adjustment model for the aged/disabled population. CMS estimated the new risk score model would drive an average impact of -3.12% to MA plan revenue in 2024. The actual revenue impact is expected to vary considerably across MA plans and risk-bearing providers. This paper dives into the drivers of the wide variation in MA plan and risk-bearing provider specific results. Read More
Proposed MA Risk Adjustment – Don’t Miss Out on the Nuanced Impacts to County Level Benchmark Rates. The average geographic adjustment factor is one of the main components of the Part C benchmark rates. A county AGA factor is calculated by taking the five-year average of geographic indices divided by a five-year enrollment weighted average risk score. This paper summarizes the potential impact to Part C benchmark rates due to the proposed CMS-HCC risk adjustment model released in the February 1, 2023, 2024 Advance Notice. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Up 0.5%, Jan-23 Data
- Iowa Medicaid Managed Care Enrollment is Up 2%, Feb-23 Data
- Nevada Medicaid Managed Care Enrollment is Up 5.7%, 2022 Data
- North Carolina Medicaid Managed Care Enrollment is Up 0.5%, Jan-23 Data
- North Dakota Medicaid Expansion Enrollment is Up 2%, Feb-23 Data
- Oregon Medicaid Managed Care Enrollment is Up 0.5%, Jan-23 Data
- South Carolina Medicaid Managed Care Enrollment is Up 0.6%, Jan-23 Data
- South Carolina Dual Demo Enrollment is Down 6%, Jan-23 Data
- Virginia Medicaid MLTSS Enrollment is Up 0.5%, Jan-23 Data
- Virginia Medicaid Managed Care Enrollment is Up 0.9%, Jan-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Iowa Hawki Dental Contract and Amendments, SFY 2019-23
- New Mexico Turquoise Care Managed Care Cancelled RFP and Evaluation Materials, Feb-23
Medicaid Program Reports, Data, and Updates:
- Illinois Medicaid Advisory Committee Meeting Materials, Nov-22
- Nevada Governor’s Proposed Budget, FY 2023-25
- New Mexico Medicaid Advisory Committee and Subcommittee Meeting Materials, Feb-23
- North Carolina Governor’s Recommended Budget, FY 2023-25
- Oregon Health Plan Section 1115 Annual Reports, 2018-22
- Rhode Island Medicaid Unwinding Presentation, Mar-23
- South Carolina Medical Care Advisory Committee Meeting Materials, Feb-23
- Texas Update on Psychotropic Medications for Children in Foster Care Report, FY2002-21
- Virginia Commonwealth Coordinated Care Plus Data Books and Capitation Rates, 2016-23
- Virginia External Quality Review Technical Reports, CY 2018-21
- Virginia Medallion 4.0 Rate Reports, 2019-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
