HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Medicaid Managed Care Enrollment Update – Q4 2022

- Alaska Submits Section 1115 Waiver Request to Extend Medicaid SUD, Behavioral Health Program

- Redeterminations News: District of Columbia, Mississippi, Washington, Wyoming

- Medicaid Expansion News: New Hampshire, North Carolina, South Dakota

- New York Has Almost $10 Billion in Surplus Federal Funding for Basic Health Option

- Oregon Medicaid CCO Purchases Hotel to Create Housing for Individuals with Behavioral Health Needs

- Pennsylvania Governor Proposes $500 Million for Mental Health Services in Schools

- Washington Pauses Apple Health Reprocurement Efforts to Focus on Medicaid Redeterminations

- Biden’s Proposed Fiscal 2024 Budget Includes Mandatory Minimum Medicaid MLR

- Help at Home Acquires Prosper Home Care

In Focus
Medicaid Managed Care Enrollment Update – Q4 2022
This week, our In Focus section reviews recent Medicaid enrollment trends in capitated, risk-based managed care in 32 states.[1] Many state Medicaid agencies post monthly enrollment figures by health plan for their Medicaid managed care population to their websites. This data allows for the timeliest analysis of enrollment trends across states and managed care organizations. All 32 states highlighted in this review have released monthly Medicaid managed care enrollment data into the fourth quarter (Q4) of 2022. This report reflects the most recent data posted. HMA will continue tracking enrollment throughout the eligibility redetermination period. HMA has made the following observations related to the enrollment data shown on Table 1 (below):
- The 32 states in this report account for an estimated 71 million Medicaid managed care enrollees as of December 2022. Based on HMA estimates of MCO enrollment in states not covered in this report, we believe that nationwide Medicaid MCO enrollment was likely about 75 million in December 2022. As such, the enrollment data across these 32 states represents approximately 95 percent of all Medicaid MCO enrollment.
- Across the 32 states tracked in this report, Medicaid managed care enrollment is up 7.5 percent year-over-year as of December 2022.
- All states, besides Mississippi, saw increases in enrollment in December 2022, compared to the previous year, due to the gains from the COVID-19 pandemic. Mississippi Medicaid managed care enrollment fell because the state shifted members to FFS during the public health emergency.
- Twenty-three of the 32 states – Arizona, California, District of Columbia, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, Ohio, Oregon, Pennsylvania, Virginia, Washington, and West Virginia – expanded Medicaid under the Affordable Care Act and have seen increased Medicaid managed care enrollment since expansion.
- The 23 expansion states listed above have seen net Medicaid managed care enrollment increase by 3.5 million members, or 7.2 percent, in the past year, to 52.2 million members at the end of 2022.
- The nine states that have not yet expanded Medicaid as of December 2022 – Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, Tennessee, Texas, and Wisconsin – have seen Medicaid managed care enrollment increase 8.3 percent to 19 million members at the end of 2022.
Table 1 – Monthly MCO Enrollment by State – July 2022 through December 2022
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Arizona | 2,069,048 | 2,079,360 | 2,095,101 | 2,106,800 | 2,116,444 | 2,127,666 |
| +/- m/m | 8,527 | 10,312 | 15,741 | 11,699 | 9,644 | 11,222 |
| % y/y | 7.6% | 0.0% | 7.5% | 7.4% | 7.2% | 7.1% |
| California | 12,929,500 | 13,013,324 | 13,073,427 | 13,132,616 | 13,231,993 | 13,204,398 |
| +/- m/m | 215,506 | 83,824 | 60,103 | 59,189 | 99,377 | (27,595) |
| % y/y | 9.8% | 9.9% | 9.9% | 9.9% | 10.2% | 9.5% |
| D.C. | 246,957 | 247,704 | 248,577 | 249,617 | 250,676 | |
| +/- m/m | 3,223 | 747 | 873 | 1,040 | 1,059 | N/A |
| % y/y | 6.7% | 6.7% | 6.5% | 6.5% | 6.4% | |
| Florida | 4,385,965 | 4,432,233 | 4,465,670 | 4,502,297 | 4,537,121 | 4,581,266 |
| +/- m/m | 41,441 | 46,268 | 33,437 | 36,627 | 34,824 | 44,145 |
| % y/y | 10.9% | 10.9% | 10.7% | 10.7% | 10.7% | 11.0% |
| Georgia | 1,975,277 | 1,988,727 | 2,016,462 | 2,027,275 | 2,035,673 | |
| +/- m/m | 13,117 | 13,450 | N/A | N/A | 10,813 | 8,398 |
| % y/y | 9.8% | 9.5% | 9.0% | 8.7% | 8.3% | |
| Illinois | 2,890,332 | 2,884,029 | 2,900,232 | 2,929,584 | 2,965,007 | 3,000,717 |
| +/- m/m | (8,672) | (6,303) | 16,203 | 29,352 | 35,423 | 35,710 |
| % y/y | 5.1% | 4.5% | 4.1% | 4.4% | 5.1% | 5.5% |
| Indiana | 1,742,762 | 1,761,692 | 1,769,400 | 1,781,464 | 1,797,451 | 1,813,044 |
| +/- m/m | 6,906 | 18,930 | 7,708 | 12,064 | 15,987 | 15,593 |
| % y/y | 11.6% | 11.3% | 11.0% | 10.5% | 10.2% | 10.3% |
| Iowa | 795,534 | 799,748 | 807,296 | 812,481 | 814,490 | |
| +/- m/m | 2,642 | 4,214 | 7,548 | N/A | N/A | 2,009 |
| % y/y | 5.9% | 5.8% | 6.4% | 6.0% | 6.1% | |
| Kansas | 489,309 | 490,911 | 492,640 | 497,257 | 499,143 | 500,814 |
| +/- m/m | 2,691 | 1,602 | 1,729 | 4,617 | 1,886 | 1,671 |
| % y/y | N/A | N/A | N/A | N/A | 8.3% | 6.3% |
| Kentucky | 1,494,068 | 1,487,387 | 1,509,274 | 1,518,906 | 1,528,484 | 1,534,657 |
| +/- m/m | 6,069 | (6,681) | 21,887 | 9,632 | 9,578 | 6,173 |
| % y/y | 5.5% | 5.3% | 5.6% | 5.8% | 6.7% | 6.1% |
| Louisiana | 1,821,644 | 1,828,015 | 1,833,457 | 1,841,693 | 1,858,092 | 1,860,170 |
| +/- m/m | 7,213 | 6,371 | 5,442 | 8,236 | 16,399 | 2,078 |
| % y/y | 4.6% | 4.5% | 4.4% | 4.7% | 5.2% | 5.8% |
| Maryland | 1,496,677 | 1,502,271 | 1,508,469 | 1,514,381 | 1,521,171 | 1,529,308 |
| +/- m/m | 8,205 | 5,594 | 6,198 | 5,912 | 6,790 | 8,137 |
| % y/y | 6.5% | 6.2% | 6.1% | 5.8% | 5.8% | 5.7% |
| Michigan | 2,280,243 | 2,294,432 | 2,299,913 | 2,309,913 | 2,319,951 | 2,324,046 |
| +/- m/m | 2,923 | 14,189 | 5,481 | 10,000 | 10,038 | 4,095 |
| % y/y | 3.8% | 3.6% | 3.5% | 3.7% | 4.5% | 4.3% |
| Minnesota | 1,261,112 | 1,262,073 | 1,278,954 | 1,286,890 | 1,293,858 | 1,299,194 |
| +/- m/m | 1,893 | 961 | 16,881 | 7,936 | 6,968 | 5,336 |
| % y/y | 7.3% | 6.7% | 7.4% | 7.5% | 7.5% | 7.5% |
| Mississippi | 367,137 | 363,387 | 364,612 | 355,694 | 367,902 | 396,880 |
| +/- m/m | (452) | (3,750) | 1,225 | (8,918) | 12,208 | 28,978 |
| % y/y | -22.7% | -19.9% | -17.4% | -17.3% | -12.5% | -3.9% |
| Missouri | 1,038,239 | 1,065,217 | 1,099,707 | 1,118,373 | 1,136,589 | 1,157,005 |
| +/- m/m | 26,520 | 26,978 | 34,490 | 18,666 | 18,216 | 20,416 |
| % y/y | 27.0% | 29.1% | 32.6% | 31.7% | 31.8% | 29.0% |
| Nebraska | 363,328 | 366,202 | 369,770 | 372,613 | 374,857 | 378,237 |
| +/- m/m | 2,740 | 2,874 | 3,568 | 2,843 | 2,244 | 3,380 |
| % y/y | 12.4% | 11.9% | 11.7% | 11.2% | 10.8% | 10.6% |
| Nevada | 687,362 | 689,139 | 697,752 | 675,465 | 685,736 | 692,890 |
| +/- m/m | 9,464 | 1,777 | 8,613 | (22,287) | 10,271 | 7,154 |
| % y/y | 9.3% | 9.0% | 9.3% | 4.2% | 5.2% | 5.7% |
| New Jersey | 2,100,947 | 2,113,930 | 2,125,181 | 2,130,868 | 2,144,514 | 2,158,966 |
| +/- m/m | 10,897 | 12,983 | 11,251 | 5,687 | 13,646 | 14,452 |
| % y/y | 7.4% | 7.4% | 7.2% | 7.0% | 7.1% | 7.0% |
| New Mexico | 809,991 | 811,732 | 812,995 | 813,630 | 814,466 | 815,798 |
| +/- m/m | 2,491 | 1,741 | 1,263 | 635 | 836 | 1,332 |
| % y/y | 4.2% | 3.7% | 3.4% | 3.0% | 2.6% | 2.3% |
| New York | 5,855,615 | 5,853,108 | 5,878,519 | 5,906,264 | 5,929,288 | 5,961,782 |
| +/- m/m | 39,970 | (2,507) | 25,411 | 27,745 | 23,024 | 32,494 |
| % y/y | 4.5% | 4.3% | 4.2% | 4.3% | 4.5% | 4.6% |
| North Carolina | 1,738,545 | 1,746,948 | 1,757,503 | 1,768,974 | 1,778,199 | 1,837,423 |
| +/- m/m | 9,047 | 8,403 | 10,555 | 11,471 | 9,225 | 59,224 |
| % y/y | 8.0% | 6.8% | 6.7% | 6.6% | 6.6% | 9.5% |
| Ohio | 2,964,731 | 2,963,616 | 2,960,922 | 2,958,666 | 2,961,983 | 2,973,763 |
| +/- m/m | (1,340) | (1,115) | (2,694) | (2,256) | 3,317 | 11,780 |
| % y/y | 3.4% | 2.6% | 1.9% | 1.4% | 1.0% | 0.9% |
| Oregon | 1,193,358 | 1,202,198 | 1,206,520 | 1,211,099 | 1,221,435 | 1,228,054 |
| +/- m/m | 3,920 | 8,840 | 4,322 | 4,579 | 10,336 | 6,619 |
| % y/y | 8.3% | 8.4% | 7.7% | 7.6% | 7.4% | 7.2% |
| Pennsylvania | 2,895,837 | 2,909,985 | 2,920,584 | 2,937,049 | 2,950,613 | 2,966,207 |
| +/- m/m | 13,973 | 14,148 | 10,599 | 16,465 | 13,564 | 15,594 |
| % y/y | 7.4% | 7.3% | 6.9% | 6.8% | 6.6% | 6.5% |
| South Carolina | 1,055,785 | 1,063,445 | 1,069,569 | 1,078,094 | 1,084,529 | 1,089,577 |
| +/- m/m | 5,226 | 7,660 | 6,124 | 8,525 | 6,435 | 5,048 |
| % y/y | 7.6% | 7.5% | 7.4% | 7.9% | 7.6% | 7.5% |
| Tennessee | 1,692,395 | 1,704,398 | 1,710,125 | 1,718,539 | 1,726,603 | 1,734,108 |
| +/- m/m | 6,737 | 12,003 | 5,727 | 8,414 | 8,064 | 7,505 |
| % y/y | 6.0% | 6.1% | 6.1% | 6.0% | 5.9% | 5.8% |
| Texas | 5,466,045 | 5,653,169 | ||||
| +/- m/m | N/A | N/A | N/A | N/A | N/A | N/A |
| % y/y | 8.6% | 10.6% | ||||
| Virginia | 1,572,923 | 1,582,973 | 1,589,722 | 1,598,875 | 1,608,840 | 1,619,311 |
| +/- m/m | 11,829 | 10,050 | 6,749 | 9,153 | 9,965 | 10,471 |
| % y/y | 11.3% | 11.0% | 10.0% | 9.6% | 10.1% | 9.8% |
| Washington | 1,884,734 | 1,898,983 | 1,904,127 | 1,913,230 | 1,927,690 | 1,959,278 |
| +/- m/m | 8,867 | 14,249 | 5,144 | 9,103 | 14,460 | 31,588 |
| % y/y | #DIV/0! | #DIV/0! | 5.8% | 5.9% | 6.0% | 7.2% |
| West Virginia | 519,992 | 524,042 | 524,922 | 527,226 | 530,494 | 533,194 |
| +/- m/m | 2,871 | 4,050 | 880 | 2,304 | 3,268 | 2,700 |
| % y/y | 6.5% | 6.8% | 6.4% | 5.9% | 5.9% | 5.7% |
| Wisconsin | 1,161,202 | 1,166,208 | 1,172,719 | 1,179,204 | 1,184,899 | 1,190,673 |
| +/- m/m | 5,263 | 5,006 | 6,511 | 6,485 | 5,695 | 5,774 |
| % y/y | 7.5% | 7.2% | 7.1% | 7.1% | 6.9% | 6.6% |
Note: In Table 1 above and the state tables below, “+/- m/m” refers to the enrollment change from the previous month. “% y/y” refers to the percentage change in enrollment from the same month in the previous year.
Below, we provide a state-specific analysis of recent enrollment trends in the states where HMA tracks data.
It is important to note the limitations of the data presented. First, not all states report the data at the same time during the month. Some of these figures reflect beginning-of-the-month totals, while others reflect an end-of-the-month snapshot. Second, in some cases the data is comprehensive in that it covers all state-sponsored health programs for which the state offers managed care; in other cases, the data reflects only a subset of the broader Medicaid managed care population. This is the key limiting factor in comparing the data described below and figures reported by publicly traded Medicaid MCOs. Consequently, the data we review in Table 1 and throughout the In Focus section should be viewed as a sampling of enrollment trends across these states rather than a comprehensive comparison, which cannot be developed based on publicly available monthly enrollment data.
State-Specific Analysis
Arizona
Medicaid Expansion Status: Expanded January 1, 2014
Enrollment in Arizona’s two Medicaid managed care programs grew to 2.1 million in December 2022, up 7.1 percent from December 2021.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Acute Care | 2,002,584 | 2,012,802 | 2,028,335 | 2,039,880 | 2,049,311 | 2,060,376 |
| ALTCS | 66,464 | 66,558 | 66,766 | 66,920 | 67,133 | 67,290 |
| Total Arizona | 2,069,048 | 2,079,360 | 2,095,101 | 2,106,800 | 2,116,444 | 2,127,666 |
| +/- m/m | 8,527 | 10,312 | 15,741 | 11,699 | 9,644 | 11,222 |
| % y/y | 7.6% | 7.5% | 7.4% | 7.2% | 7.1% |
California
Medicaid Expansion Status: Expanded January 1, 2014
Medi-Cal managed care enrollment was up 9.5 percent year-over-year to 13.2 million, as of December 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Two-Plan Counties | 8,356,137 | 8,409,817 | 8,446,514 | 8,481,885 | 8,548,096 | 8,588,418 |
| Imperial/San Benito | 100,384 | 101,117 | 101,633 | 102,064 | 102,881 | 103,437 |
| Regional Model | 364,066 | 366,437 | 368,624 | 370,361 | 373,402 | 375,473 |
| GMC Counties | 1,435,250 | 1,445,532 | 1,452,127 | 1,458,149 | 1,470,122 | 1,391,421 |
| COHS Counties | 2,561,831 | 2,578,747 | 2,593,003 | 2,608,731 | 2,625,795 | 2,634,112 |
| Duals Demonstration | 111,832 | 111,674 | 111,526 | 111,426 | 111,697 | 111,537 |
| Total California | 12,929,500 | 13,013,324 | 13,073,427 | 13,132,616 | 13,231,993 | 13,204,398 |
| +/- m/m | 215,506 | 83,824 | 60,103 | 59,189 | 99,377 | (27,595) |
| % y/y | 9.8% | 9.9% | 9.9% | 9.9% | 10.2% | 9.5% |
District of Columbia
Medicaid Expansion Status: Expanded January 1, 2014
Medicaid managed care enrollment in the District of Columbia was up 6.4 percent to almost 251,000 in November 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | |
| Total District of Columbia | 246,957 | 247,704 | 248,577 | 249,617 | 250,676 |
| +/- m/m | 3,223 | 747 | 873 | 1,040 | 1,059 |
| % y/y | 6.7% | 6.7% | 6.5% | 6.5% | 6.4% |
Florida
Medicaid Expansion Status: Not Expanded
Florida’s statewide Medicaid managed care program had seen an 11 percent rise in total covered lives over the last year to nearly 4.6 million beneficiaries as of December 2022. (Note that the managed LTC enrollment figures listed below are a subset of the Managed Medical Assistance (MMA) enrollments and are included in the MMA number; they are not separately added to the total to avoid double counting).
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| MMA | 3,908,539 | 3,948,929 | 3,978,098 | 4,010,534 | 4,041,816 | 4,080,381 |
| LTC (Subset of MMA) | 124,107 | 124,691 | 125,397 | 126,144 | 126,720 | 126,621 |
| SMMC Specialty Plan | 332,179 | 338,057 | 342,325 | 346,516 | 350,058 | 355,638 |
| FL Healthy Kids | 145,247 | 145,247 | 145,247 | 145,247 | 145,247 | 145,247 |
| Total Florida | 4,385,965 | 4,432,233 | 4,465,670 | 4,502,297 | 4,537,121 | 4,581,266 |
| +/- m/m | 41,441 | 46,268 | 33,437 | 36,627 | 34,824 | 44,145 |
| % y/y | 10.9% | 10.9% | 10.7% | 10.7% | 10.7% | 11.0% |
Georgia
Medicaid Expansion Status: Not Expanded
As of December 2022, Georgia’s Medicaid managed care program covered more than 2 million members, up 8.3 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Georgia | 1,975,277 | 1,988,727 | 2,016,462 | 2,027,275 | 2,035,673 | |
| +/- m/m | 13,117 | 13,450 | 10,813 | 8,398 | ||
| % y/y | 9.8% | 9.5% | 9.0% | 8.7% | 8.3% |
Illinois
Medicaid Expansion Status: Expanded January 1, 2014
Illinois enrollment across the state’s managed care programs was up 5.5 percent to 3 million as of December 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| HealthChoice | 2,800,420 | 2,793,124 | 2,809,689 | 2,839,342 | 2,874,700 | 2,909,303 |
| Duals Demonstration | 89,912 | 90,905 | 90,543 | 90,242 | 90,307 | 91,414 |
| Total Illinois | 2,890,332 | 2,884,029 | 2,900,232 | 2,929,584 | 2,965,007 | 3,000,717 |
| +/- m/m | (8,672) | (6,303) | 16,203 | 29,352 | 35,423 | 35,710 |
| % y/y | 5.1% | 4.5% | 4.1% | 4.4% | 5.1% | 5.5% |
Indiana
Medicaid Expansion Status: Expanded in 2015 through HIP 2.0
As of December 2022, enrollment in Indiana’s managed care programs—Hoosier Healthwise, Hoosier Care Connect, and Healthy Indiana Program (HIP)—was more than 1.8 million, up 10.3 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Hoosier Healthwise | 845,910 | 852,904 | 857,952 | 863,973 | 869,613 | 876,606 |
| Hoosier Care Connect | 102,805 | 102,819 | 102,537 | 102,253 | 102,200 | 102,150 |
| HIP | 794,047 | 805,969 | 808,911 | 815,238 | 825,638 | 834,288 |
| Indiana Total | 1,742,762 | 1,761,692 | 1,769,400 | 1,781,464 | 1,797,451 | 1,813,044 |
| +/- m/m | 6,906 | 18,930 | 7,708 | 12,064 | 15,987 | 15,593 |
| % y/y | 11.6% | 11.3% | 11.0% | 10.5% | 10.2% | 10.3% |
Iowa
Medicaid Expansion Status: Expanded January 1, 2014
Iowa launched its statewide Medicaid managed care program in April of 2016. Enrollment across all populations was nearly 814,500, as of December 2022. Enrollment was up 6.1 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Traditional Medicaid | 507,266 | 510,618 | 516,556 | 520,234 | 521,118 | |
| Iowa Wellness Plan | 237,910 | 239,261 | 242,555 | 244,724 | 246,385 | |
| hawk-i | 50,358 | 49,869 | 48,185 | 47,523 | 46,987 | |
| Total Iowa | 795,534 | 799,748 | 807,296 | 812,481 | 814,490 | |
| +/- m/m | 2,642 | 4,214 | 7,548 | 2,009 | ||
| % y/y | 5.9% | 5.8% | 6.4% | 6.0% | 6.1% |
Kansas
Medicaid Expansion Status: Not Expanded
Kansas Medicaid managed care enrollment was nearly 501,000 as of December 2022, up 6.3 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Kansas | 489,309 | 490,911 | 492,640 | 497,257 | 499,143 | 500,814 |
| +/- m/m | 2,691 | 1,602 | 1,729 | 4,617 | 1,886 | 1,671 |
| % y/y | 8.3% | 6.3% |
Kentucky
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, Kentucky covered more than 1.5 million beneficiaries in risk-based managed care. Total enrollment was up 6.1 percent from the prior year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Kentucky | 1,494,068 | 1,487,387 | 1,509,274 | 1,518,906 | 1,528,484 | 1,534,657 |
| +/- m/m | 6,069 | (6,681) | 21,887 | 9,632 | 9,578 | 6,173 |
| % y/y | 5.5% | 5.3% | 5.6% | 5.8% | 6.7% | 6.1% |
Louisiana
Medicaid Expansion Status: Expanded July 1, 2016
Medicaid managed care enrollment in Louisiana was more than 1.86 million as of December 2022, up 5.8 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Louisiana | 1,821,644 | 1,828,015 | 1,833,457 | 1,841,693 | 1,858,092 | 1,860,170 |
| +/- m/m | 7,213 | 6,371 | 5,442 | 8,236 | 16,399 | 2,078 |
| % y/y | 4.6% | 4.5% | 4.4% | 4.7% | 5.2% | 5.8% |
Maryland
Medicaid Expansion Status: Expanded January 1, 2014
Maryland’s Medicaid managed care program covered more than 1.5 million lives as of December 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Maryland | 1,496,677 | 1,502,271 | 1,508,469 | 1,514,381 | 1,521,171 | 1,529,308 |
| +/- m/m | 8,205 | 5,594 | 6,198 | 5,912 | 6,790 | 8,137 |
| % y/y | 6.5% | 6.2% | 6.1% | 5.8% | 5.8% | 5.7% |
Michigan
Medicaid Expansion Status: Expanded April 1, 2014
As of December 2022, Michigan’s Medicaid managed care was up 4.3 percent to 2.3 million.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Medicaid | 2,239,937 | 2,251,810 | 2,256,800 | 2,265,219 | 2,274,763 | 2,279,473 |
| MI Health Link (Duals) | 40,306 | 42,622 | 43,113 | 44,694 | 45,188 | 44,573 |
| Total Michigan | 2,280,243 | 2,294,432 | 2,299,913 | 2,309,913 | 2,319,951 | 2,324,046 |
| +/- m/m | 2,923 | 14,189 | 5,481 | 10,000 | 10,038 | 4,095 |
| % y/y | 3.8% | 3.6% | 3.5% | 3.7% | 4.5% | 4.3% |
Minnesota
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, enrollment across Minnesota’s multiple managed Medicaid programs was nearly 1.3 million, up 7.5 percent from the prior year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Parents/Kids | 748,197 | 748,513 | 758,100 | 763,044 | 767,798 | 770,918 |
| Expansion Adults | 272,666 | 273,387 | 278,421 | 281,284 | 284,073 | 288,680 |
| Senior Care Plus | 24,190 | 24,252 | 25,344 | 25,914 | 26,415 | 26,740 |
| Senior Health Options | 43,429 | 43,686 | 43,920 | 44,162 | 44,248 | 44,324 |
| Special Needs BasicCare | 64,656 | 64,484 | 65,562 | 65,763 | 65,987 | 66,171 |
| Moving Home Minnesota | 11 | 11 | 10 | 10 | 9 | 11 |
| Minnesota Care | 107,963 | 107,740 | 107,597 | 106,713 | 105,328 | 102,350 |
| Total Minnesota | 1,261,112 | 1,262,073 | 1,278,954 | 1,286,890 | 1,293,858 | 1,299,194 |
| +/- m/m | 1,893 | 961 | 16,881 | 7,936 | 6,968 | 5,336 |
| % y/y | 7.3% | 6.7% | 7.4% | 7.5% | 7.5% | 7.5% |
Mississippi
Medicaid Expansion Status: Not Expanded
MississippiCAN, the state’s Medicaid managed care program, had membership down 3.9 percent to nearly 397,000 as of December 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Mississippi | 367,137 | 363,387 | 364,612 | 355,694 | 367,902 | 396,880 |
| +/- m/m | (452) | (3,750) | 1,225 | (8,918) | 12,208 | 28,978 |
| % y/y | -22.7% | -19.9% | -17.4% | -17.3% | -12.5% | -3.9% |
Missouri
Medicaid Expansion Status: Expansion Enrollment began in October 2021
Missouri managed care enrollment in the Medicaid and CHIP programs was nearly 1.2 million in December 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Medicaid | 758,928 | 757,312 | 769,419 | 775,076 | 782,863 | 787,611 |
| Total CHIP | 28,949 | 28,937 | 29,026 | 29,121 | 29,231 | 29,402 |
| Total AEG | 199,963 | 228,361 | 250,131 | 262,612 | 272,574 | 287,692 |
| Total SHK | 50,399 | 50,607 | 51,131 | 51,564 | 51,921 | 52,300 |
| Total Missouri | 1,038,239 | 1,065,217 | 1,099,707 | 1,118,373 | 1,136,589 | 1,157,005 |
| +/- m/m | 26,520 | 26,978 | 34,490 | 18,666 | 18,216 | 20,416 |
| % y/y | 27.0% | 29.1% | 32.6% | 31.7% | 31.8% | 29.0% |
Nebraska
Medicaid Expansion Status: Expanded October 1, 2020
As of December 2022, Nebraska’s Medicaid managed care program enrolled 378,000 members, up 10.6 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Nebraska | 363,328 | 366,202 | 369,770 | 372,613 | 374,857 | 378,237 |
| +/- m/m | 2,740 | 2,874 | 3,568 | 2,843 | 2,244 | 3,380 |
| % y/y | 12.4% | 11.9% | 11.7% | 11.2% | 10.8% | 10.6% |
Nevada
Medicaid Expansion Status: Expanded January 1, 2014
Nevada’s Medicaid managed care enrollment was up 5.7 percent to nearly 693,000 as of December 2022.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Nevada | 687,362 | 689,139 | 697,752 | 675,465 | 685,736 | 692,890 |
| +/- m/m | 9,464 | 1,777 | 8,613 | (22,287) | 10,271 | 7,154 |
| % y/y | 9.3% | 9.0% | 9.3% | 4.2% | 5.2% | 5.7% |
New Jersey
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, New Jersey Medicaid managed care enrollment was up 7 percent to nearly 2.2 million.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total New Jersey | 2,100,947 | 2,113,930 | 2,125,181 | 2,130,868 | 2,144,514 | 2,158,966 |
| +/- m/m | 10,897 | 12,983 | 11,251 | 5,687 | 13,646 | 14,452 |
| % y/y | 7.4% | 7.4% | 7.2% | 7.0% | 7.1% | 7.0% |
New Mexico
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, New Mexico’s Centennial Care program covered nearly 816,000 members, up 2.3 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total New Mexico | 809,991 | 811,732 | 812,995 | 813,630 | 814,466 | 815,798 |
| +/- m/m | 2,491 | 1,741 | 1,263 | 635 | 836 | 1,332 |
| % y/y | 4.2% | 3.7% | 3.4% | 3.0% | 2.6% | 2.3% |
New York
Medicaid Expansion Status: Expanded January 1, 2014
New York’s Medicaid managed care programs collectively covered nearly 6 million beneficiaries as of December 2022, a 4.6 percent increase from the previous year. The Medicaid Advantage program ended in December 2021.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Mainstream MCOs | 5,399,089 | 5,395,489 | 5,418,915 | 5,446,409 | 5,467,467 | 5,494,358 |
| Managed LTC | 255,999 | 256,538 | 258,236 | 257,360 | 260,087 | 264,965 |
| Medicaid Advantage | 0 | 0 | 0 | 0 | 0 | 0 |
| Medicaid Advantage Plus | 34,357 | 34,355 | 34,689 | 34,764 | 34,717 | 35,061 |
| HARP | 164,514 | 165,067 | 165,024 | 166,063 | 165,340 | 165,713 |
| FIDA-IDD (Duals) | 1,656 | 1,659 | 1,655 | 1,668 | 1,677 | 1,685 |
| Total New York | 5,855,615 | 5,853,108 | 5,878,519 | 5,906,264 | 5,929,288 | 5,961,782 |
| +/- m/m | 39,970 | (2,507) | 25,411 | 27,745 | 23,024 | 32,494 |
| % y/y | 4.5% | 4.3% | 4.2% | 4.3% | 4.5% | 4.6% |
North Carolina
Medicaid Expansion Status: Not Expanded
As of December 2022, enrollment in North Carolina’s Medicaid managed care program was 1.8 million, up 9.5 percent from the prior year. North Carolina implemented Medicaid managed care on July 1, 2021.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total North Carolina | 1,738,545 | 1,746,948 | 1,757,503 | 1,768,974 | 1,778,199 | 1,837,423 |
| +/- m/m | 9,047 | 8,403 | 10,555 | 11,471 | 9,225 | 59,224 |
| % y/y | 8.0% | 6.8% | 6.7% | 6.6% | 6.6% | 9.5% |
Ohio
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, enrollment across all four Ohio Medicaid managed care programs was nearly 3 million, up 0.9 percent from the prior year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| CFC Program | 1,800,781 | 1,800,038 | 1,798,135 | 1,796,327 | 1,798,873 | 1,804,860 |
| ABD/Duals | 348,071 | 348,176 | 347,461 | 347,371 | 347,473 | 347,839 |
| Group 8 (Expansion) | 815,879 | 815,402 | 815,326 | 814,968 | 815,637 | 821,064 |
| Total Ohio | 2,964,731 | 2,963,616 | 2,960,922 | 2,958,666 | 2,961,983 | 2,973,763 |
| +/- m/m | (1,340) | (1,115) | (2,694) | (2,256) | 3,317 | 11,780 |
| % y/y | 3.4% | 2.6% | 1.9% | 1.4% | 1.0% | 0.9% |
Oregon
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, enrollment in the Oregon Coordinated Care Organization (CCO) Medicaid managed care program was more than 1.2 million, up 7.2 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Oregon | 1,193,358 | 1,202,198 | 1,206,520 | 1,211,099 | 1,221,435 | 1,228,054 |
| +/- m/m | 3,920 | 8,840 | 4,322 | 4,579 | 10,336 | 6,619 |
| % y/y | 8.3% | 8.4% | 7.7% | 7.6% | 7.4% | 7.2% |
Pennsylvania
Medicaid Expansion Status: Expanded January 1, 2015
As of December 2022, Pennsylvania’s Medicaid managed care enrollment was nearly 3 million, up 6.5 percent in the past year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Pennsylvania | 2,895,837 | 2,909,985 | 2,920,584 | 2,937,049 | 2,950,613 | 2,966,207 |
| +/- m/m | 13,973 | 14,148 | 10,599 | 16,465 | 13,564 | 15,594 |
| % y/y | 7.4% | 7.3% | 6.9% | 6.8% | 6.6% | 6.5% |
South Carolina
Medicaid Expansion Status: Not Expanded
South Carolina’s Medicaid managed care programs collectively enrolled nearly 1.1 million members as of December 2022, which represents an increase of 7.5 percent in the past year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Medicaid | 1,041,909 | 1,049,706 | 1,056,026 | 1,064,548 | 1,071,016 | 1,076,146 |
| Total Duals Demo | 13,876 | 13,739 | 13,543 | 13,546 | 13,513 | 13,431 |
| Total South Carolina | 1,055,785 | 1,063,445 | 1,069,569 | 1,078,094 | 1,084,529 | 1,089,577 |
| +/- m/m | 5,226 | 7,660 | 6,124 | 8,525 | 6,435 | 5,048 |
| % y/y | 7.6% | 7.5% | 7.4% | 7.9% | 7.6% | 7.5% |
Tennessee
Medicaid Expansion Status: Not Expanded
As of December 2022, TennCare managed care enrollment totaled 1.7 million, up 5.8 percent from the prior year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Tennessee | 1,692,395 | 1,704,398 | 1,710,125 | 1,718,539 | 1,726,603 | 1,734,108 |
| +/- m/m | 6,737 | 12,003 | 5,727 | 8,414 | 8,064 | 7,505 |
| % y/y | 6.0% | 6.1% | 6.1% | 6.0% | 5.9% | 5.8% |
Texas
Medicaid Expansion Status: Not Expanded
Texas’ state fiscal year begins in September and program-specific enrollment is only reported at the end of each state fiscal quarter. As of November 2022, Texas Medicaid managed care enrollment was nearly 5.7 million across the state’s six managed care programs, up 10.6 percent from the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| STAR | 4,559,293 | 4,748,820 | ||||
| STAR+PLUS | 559,746 | 568,456 | ||||
| STAR HEALTH | 45,760 | 46,228 | ||||
| Duals Demo | 34,336 | 33,673 | ||||
| CHIP | 97,153 | 85,773 | ||||
| STAR KIDS | 169,757 | 170,219 | ||||
| Total Texas | 5,466,045 | 5,653,169 | ||||
| +/- m/m | ||||||
| % y/y | 8.6% | 10.6% |
Virginia
Medicaid Expansion Status: January 1, 2019
Virginia Medicaid managed care enrollment was up 9.8 percent in December 2022 to 1.6 million members.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Virginia | 1,572,923 | 1,582,973 | 1,589,722 | 1,598,875 | 1,608,840 | 1,619,311 |
| +/- m/m | 11,829 | 10,050 | 6,749 | 9,153 | 9,965 | 10,471 |
| % y/y | 11.3% | 11.0% | 10.0% | 9.6% | 10.1% | 9.8% |
Washington
Medicaid Expansion Status: Expanded January 1, 2014
Washington’s Medicaid managed care enrollment increased 7.2 percent to nearly 2 million as of December 2022, compared to the previous year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total Washington | 1,884,734 | 1,898,983 | 1,904,127 | 1,913,230 | 1,927,690 | 1,959,278 |
| +/- m/m | 8,867 | 14,249 | 5,144 | 9,103 | 14,460 | 31,588 |
| % y/y | #DIV/0! | #DIV/0! | 5.8% | 5.9% | 6.0% | 7.2% |
West Virginia
Medicaid Expansion Status: Expanded January 1, 2014
As of December 2022, West Virginia’s Medicaid managed care program covered 533,000 members, up 5.7 percent year-over-year.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| Total West Virginia | 519,992 | 524,042 | 524,922 | 527,226 | 530,494 | 533,194 |
| +/- m/m | 2,871 | 4,050 | 880 | 2,304 | 3,268 | 2,700 |
| % y/y | 6.5% | 6.8% | 6.4% | 5.9% | 5.9% | 5.7% |
Wisconsin
Medicaid Expansion Status: Not Expanded
Across Wisconsin’s three Medicaid managed care programs, December 2022 enrollment totaled nearly 1.2 million, up 6.6 percent from the year before.
| Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 | Dec-22 | |
| BadgerCare+ | 1,042,456 | 1,047,217 | 1,053,361 | 1,059,587 | 1,065,182 | 1,070,788 |
| SSI | 61,841 | 61,916 | 62,065 | 62,129 | 62,165 | 62,293 |
| LTC | 56,905 | 57,075 | 57,293 | 57,488 | 57,552 | 57,592 |
| Total Wisconsin | 1,161,202 | 1,166,208 | 1,172,719 | 1,179,204 | 1,184,899 | 1,190,673 |
| +/- m/m | 5,263 | 5,006 | 6,511 | 6,485 | 5,695 | 5,774 |
| % y/y | 7.5% | 7.2% | 7.1% | 7.1% | 6.9% | 6.6% |
More Information Available from HMA Information Services
More detailed information on the Medicaid managed care landscape is available from HMA Information Services (HMAIS), which collects Medicaid enrollment data, health plan financials, and the latest on expansions, waivers, duals, ABD populations, long-term care, accountable care organizations, and patient-centered medical homes. HMAIS also includes a public documents library with copies of Medicaid RFPs, responses, model contracts, and scoring sheets.
HMAIS enhances this publicly available information with an overview of the structure of Medicaid in each state, as well as proprietary Medicaid Managed Care RFP calendars.
For additional information on how to subscribe to HMA Information Services, contact Carl Mercurio at 212-575-5929 or [email protected].
[1] Arizona, California, District of Columbia, Florida, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, Ohio, Oregon, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, Washington, West Virginia, Wisconsin.
HMA Roundup
Alaska
Alaska Submits Section 1115 Waiver Request to Extend Medicaid SUD, Behavioral Health Program. Alaska submitted on March 1, 2023, a Section 1115 waiver request to extend the current Medicaid substance use disorder (SUD) and behavioral health program demonstration. The request to the Centers for Medicare & Medicaid Services seeks to maintain the waiver, with only minimal changes. The demonstration’s goal is to implement a data-driven, integrated behavioral health system of care for Alaskans with serious mental illness, severe emotional disturbance, and/or substance use disorders. Alaska has not yet been able to fully implement the waiver programs and is seeking to do so with this extension. The public comment period ends April 9, 2023. Read More
District of Columbia
District of Columbia Starts Public Awareness Campaign Ahead of Medicaid Redeterminations. The District of Columbia Department of Health Care Finance announced on March 8, 2023, that it has begun outreach, urging Medicaid beneficiaries to update contact information and renew coverage during the upcoming eligibility redeterminations process. Grassroots outreach will be through neighborhood and citywide events, virtual meetings, an advertising campaign that directs beneficiaries on steps to renew, and a toolkit to assist in outreach from community-based organizations and government agencies. Read More
Mississippi
Mississippi Hires Staff, Contractors to Assist With Medicaid Redeterminations. Mississippi Today reported on March 14, 2023, that the Mississippi Division of Medicaid has hired 22 new workers and 100 contractors to assist with Medicaid redeterminations. The state launched an awareness campaign in January and invited community partners to assist in urging beneficiaries to update contact information. The state has not published its public health emergency unwinding plan yet. Read More
Mississippi Hospitals Expect Big Cut in Supplemental Payments Under Proposed Change. Mississippi Today reported on March 9, 2023, that Mississippi hospitals expect supplemental payments from the state Hospital Access Program will drop to about $40 million from an expected $450 million this year because of a proposed change to the payment model. The Mississippi Division of Medicaid submitted the proposal to federal regulators, seeking to peg payments to the difference between commercial and Medicaid rates. Read More
Montana
House Committee Adds Budget Provision to Extend Postpartum Medicaid Coverage. The Montana Free Press reported on March 14, 2023, that the Montana House Appropriations Committee added a provision to the state budget bill to extend postpartum Medicaid coverage from 60 days to 12 months. The budget now moves to the House floor for a debate. Read More
New Hampshire
New Hampshire Senate Gives Preliminary Approval to Continuing Medicaid Expansion. The Associated Press reported on March 9, 2023, that the New Hampshire Senate gave preliminary approval to a bill to continue Medicaid expansion in the state. The bill now heads to the Finance Committee. Read More
New York
New York Has Almost $10 Billion in Surplus Federal Funding for Basic Health Option. Crain’s New York reported on March 9, 2023, that New York has $9.9 billion in surplus federal funding for its Essential Plan basic health program option. The Basic Health Program, included in the Affordable Care Act, provides states with 95 percent of the federal subsidy available to enrollees who purchase silver plans through the Exchange. The funding can only be used for enrollees in the Essential Plan. Read More
Legislature Recommends 10 Percent Increase in Medicaid Reimbursement Rates for Hospitals. Crain’s New York reported on March 15, 2023, that the New York State Assembly and Senate both recommended a 10 percent increase in Medicaid reimbursement rates for hospitals in their budget resolutions. Governor Kathy Hochul’s budget proposal included an increase of five percent. The Senate and Assembly also both proposed increasing the Medicaid reimbursement rates for nursing homes. Read More
Senate Passes Bill to Create Directory of Doulas for Medicaid Beneficiaries. WNY News Now reported on March 8, 2023, that the New York Senate passed a bill that would require the state to maintain a directory for doulas accepting Medicaid. The bill now moves to the Assembly. Read More
North Carolina
Senate Gives Initial Approval to Medicaid Expansion Bill. The Associated Press reported on March 14, 2023, that the North Carolina Senate gave initial approval to a Medicaid expansion bill. The bill also includes changes to hospital certificate of need rules. The bill will require a second Senate vote and a House vote before it goes to Governor Roy Cooper, who is expected to sign it. Read More
Senate Passes Bill to Contract With Statewide Health Plan for Children in Foster Care. The Winston-Salem Journal reported on March 8, 2023, that the North Carolina Senate passed a bill (Senate Bill 156) to contract with a statewide, prepaid health plan for children in foster care. The plan would cover physical and behavioral health services. Any qualified vendor can submit a bid, including any of the state’s six contracted managed care organizations. Currently, Medicaid coverage for children in foster care is handled at the county level. The bill now moves to the House. Read More
North Dakota
North Dakota Seeks Public Comments on Ending Medicaid Technology Dependent Waiver. The North Dakota Department of Health and Human Services announced on March 8, 2023, that it is seeking public comments on an amendment to terminate the state’s Medicaid 1915(c) Technology Dependent waiver. No individuals are currently participating. Public comments will be accepted until March 31. Read More
Oklahoma
House Passes Bill to Extend Postpartum Medicaid Coverage. KOCO reported on March 14, 2023, that the Oklahoma House passed a bill to extend postpartum Medicaid coverage from 60 days to 12 months by instructing the Oklahoma Health Care Authority to seek a federal Medicaid waiver. The bill also extends coverage to women who are within 205 percent of the federal poverty level instead of 133 percent. The bill now goes to the state Senate. Read More
Oregon
Oregon Medicaid CCO Purchases Hotel to Create Housing for Individuals with Behavioral Health Needs, Health Care Professionals. OPB reported on March 12, 2023, that Medicaid coordinated care organization (CCO) CareOregon purchased a hotel for $8 million and plans to turn it into housing for individuals with behavioral health needs and health care professionals. CareOregon’s Columbia Pacific CCO will run the building in partnership with Clatsop Behavioral Health. Read More
Pennsylvania
Governor Proposes $500 Million for Mental Health Services in Schools in Fiscal 2024 Budget. Pennsylvania Governor Josh Shapiro proposed on March 7, 2023, $500 million to increase mental health services in schools in his fiscal 2024 budget. He is also proposing $4 million to create three community-based programs to reduce or prevent admissions to state facilities, an additional $17.6 million toward reducing the waiting list for home and community-based services, and $1.9 million in resources for long-term care facilities. Read More
South Dakota
Lawmakers Propose Fiscal 2024 Budget with Medicaid Expansion. The Argus Leader reported on March 9, 2023, that South Dakota lawmakers proposed a fiscal 2024 budget that includes Medicaid expansion as well as funding increases for hospitals and certain community support providers. Read More
Washington
Washington Pauses Apple Health Reprocurement Efforts to Focus on Medicaid Redeterminations. The Washington Health Care Authority (HCA) announced on March 13, 2023, that it will pause reprocurement efforts for the Apple Health Medicaid managed care program while it focuses on Medicaid redeterminations. It has been over 10 years since the state last procured Medicaid managed care plans. HCA announced last year that it was aiming for new contracts to be implemented January 1, 2025. Read More
West Virginia
Legislature Passes Hospital Certification of Need Bill. The Associated Press reported on March 9, 2023, that the West Virginia House passed a bill to eliminate certificate of need requirements for hospitals seeking to improve or add services if the hospital spends less than $100 million on facility or medical equipment acquisitions, expansions, or improvements. Currently, the minimum is $5 million. The bill already passed the Senate. Read More
Wyoming
Wyoming Could Disenroll Up to 15,000 Medicaid Beneficiaries When Redeterminations Begin. The Casper Star Tribune reported on March 9, 2023, that 10,000 to 15,000 Medicaid beneficiaries in Wyoming could lose coverage when redeterminations begin, according to a spokesperson for the state Department of Health. The state began contacting beneficiaries and resuming eligibility screenings in early March. During the public health emergency Medicaid enrollment in the state increased from 58,500 to more than 77,000. Read More
National
AHIP Leads Coalition to Offer Support During Redeterminations. Becker’s Payer Issues reported on March 9, 2023, that a new coalition, Connecting to Coverage Coalition (CCC), led by AHIP and 15 other healthcare organizations, will offer support to individuals and stakeholders during the Medicaid redetermination period. CCC will offer a website with resources for Medicaid members to navigate the process and offer healthcare navigators with toolkits and best practices for connecting with members. Read More
Biden’s Proposed Fiscal 2024 Budget Includes Mandatory Minimum Medicaid MLR. Modern Healthcare reported on March 9, 2023, that President Biden’s fiscal 2024 budget proposal would require all Medicaid and CHIP managed care plans to meet a minimum medical loss ratio (MLR) of 85 percent. The proposed budget also reduces out-of-pocket costs for Medicare enrollees and includes $150 million for home and community-based services, $100 million for crisis response programs, and $400 million for the Health Resources and Services Administration and Substance Abuse and Mental Health Services Administration programs. Read More
CMS Releases Guidance to State Medicaid Agencies on Third-Party Liability Requirements. The Centers for Medicare & Medicaid Services (CMS) released on March 8, 2023, guidance to state Medicaid agencies on two new third-party liability (TPL) requirements. The first concerns a new law that bars liable third-party payers from refusing payment solely because an item or service did not receive prior authorization. The second concerns allowing a state to create a lien over injury settlement proceeds attributable to future medical expenses. Read More
HHS Says 27 Prescriptions May Have Lower Coinsurance through Inflation Rebate Program. The U.S. Department of Health and Human Services (HHS) announced on March 15, 2023, that 27 prescription drugs may have lower Medicare Part B beneficiary coinsurance, starting on April 1, through the Medicare Prescription Drug Inflation Rebate Program. HHS will also discourage drug companies from increasing prices faster than inflation. The rebate program will save eligible beneficiaries between $2 and $390 per average dose. Read More
HHS Secretary Becerra Urges States to Minimize Medicaid Coverage Losses During Redeterminations. CNN reported on March 9, 2023, that HHS Secretary Xavier Becerra sent letters to state governors urging them to adopt measures to minimize coverage losses during the Medicaid redetermination period. If states do not comply, they will risk losing enhanced federal Medicaid funding for the remainder of the year. States will also be required to report monthly renewals and terminations, among other metrics. Read More
MACPAC Makes Recommendations on Medicaid Data Collection, Drug Coverage. The Medicaid and CHIP Payment and Access Commission (MACPAC) recommended on March 15, 2023, that federal regulators improve the collection of race and ethnicity data in Medicaid, increase transparency and improve the collection of nursing facility payment data, give state Medicaid programs greater flexibility in following Medicare drug coverage decisions, and examine payment policy for the nation’s safety net hospitals. MACPAC made the recommendations in its March 2023 Report to Congress on Medicaid and Children’s Health Insurance Program. Read More
Researchers Develop Medicare Advantage Health Equity Dashboard. HealthITAnalytics reported on March 10, 2023, that researchers developed a dashboard, presenting health equity performance data on Medicare Advantage plans. Details on the Health Equity Summary Score were published in The American Journal of Managed Care. Read More
U.S. Senator Introduces Bill to Increase Medicaid Funding for HCBS. The Senate Special Committee On Aging announced on March 9, 2023, that Senator Bob Casey (D-PA) introduced the Home and Community-based Services (HCBS) Access Act, which aims to reduce waiting lists for home care services. The bill would increase Medicaid funding for HCBS, provide grant funding to states, provide training and support for family caregivers, and provide other resources for states. Read More
Industry News
Help at Home Acquires Prosper Home Care. Help at Home announced on March 7, 2023, its acquisition of Georgia-based Prosper Home Care. Help at Home provides in-home personal care services across 10 locations in Georgia. Read More
Plaintiffs Appeal Decision in Behavioral Class Action Lawsuit. Modern Healthcare reported on March 13, 2023, that plaintiffs appealed a ruling in a class-action lawsuit against UnitedHealth Group, which found the company is not required to adhere to established clinical guidelines when deciding whether to deny certain behavioral health claims. The American Medical Association, American Psychiatric Association, multiple states, and other stakeholders have submitted briefs in support of the plaintiff appeal. Read More
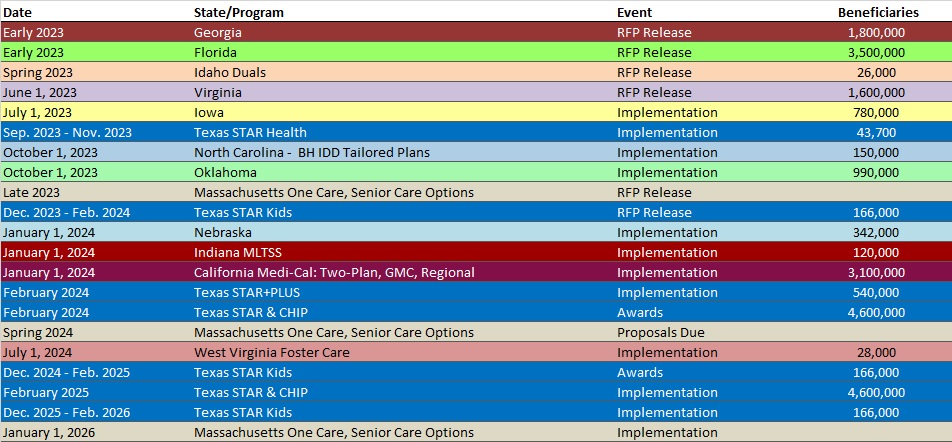
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- California Medicaid Managed Care Enrollment is Up 9.6%, 2022 Data
- California Dual Demo Enrollment is Down 3.7%, 2022 Data
- Kentucky Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- Minnesota Medicaid Managed Care Enrollment is Up 0.7%, Jan-23 Data
- Mississippi Medicaid Managed Care Enrollment is Flat, Feb-23 Data
- Missouri Medicaid Managed Care Enrollment is Up 1.6%, Jan-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- South Carolina Medicaid Managed Care Enrollment is Up 7.7%, 2022 Data
- South Carolina Dual Demo Enrollment is Down 11.5%, 2022 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 6.6%, 2022 Data
Public Documents:
Medicaid Program Reports, Data, and Updates:
- Arizona End of Continuous Enrollment Toolkit, Feb-23
- California Medi-Cal Dental Managed Care Rate Certifications, 2021-23
- California Medi-Cal Managed Care Rate Certifications, 2022-23
- District of Columbia Plan for Unwinding Continuous Coverage, Mar-23
- Minnesota Plan to Unwind Continuous Eligibility Coverage, Jan-23
- Nevada External Quality Review Technical Reports, SFY 2014-22
- North Dakota End of Medicaid Continuous Enrollment Plan, Mar-23
- Ohio Encounter Data Study for Managed Care Plans, 2022
- Texas Foster Care Rate Modernization Report, Feb-23
- Texas HHS Presentations to Legislative Committees, Feb-23
- Texas Long-term Care Regulatory Annual Reports, FY 2018-22
- Texas Quarterly Reports from the HHS Ombudsman Managed Care Assistance Team, FY 2019-23
- Wisconsin External Quality Review Annual Technical Reports, 2014-21
- Wisconsin Medicaid Managed Care Quality Strategies, 2018-21
- Wisconsin Medicaid MCO Actuarial Rate Certifications and Capitation Rates, 2018-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
