HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Ohio Releases Next Generation MyCare Ohio Program RFA

- Arkansas to Transition Medicaid Managed Care Dental Program Back to Fee-for-Service

- Colorado Governor Signs Bills Addressing Housing, Nutrition Support Funding, Prescription Drug Access

- Florida Governor Signs Bill to Establish Rural Emergency Hospitals

- Indiana Receives Federal Approval to Transition LTSS to Managed Care

- Michigan Selects Eight PIHPs for Substance Abuse Recovery Incentives Pilot Program

- Minnesota Releases Medicaid, MinnesotaCare IHP RFP

- Tennessee Awards Medicaid Dental Contract to Renaissance Life & Health Insurance Company

- CMS Releases ACO Primary Care Flex Model RFA

- HHS Selects Ten Additional States to Participate in CCBHC Demonstration

- Evolent Health to Acquire AI Assets from Machinify

- Solarity Announces Strategic Growth Investment from Private Equity Firm TA Associates

- More News Here

In Focus
Ohio Releases Next Generation MyCare Ohio Program RFA
This week’s In Focus section delves into the Next Generation MyCare Ohio managed care program, spotlighting the request for applications (RFA) that the Ohio Department of Medicaid (ODM) released on May 31, 2024. The MyCare Ohio Program, which serves people who are dually eligible for both Medicaid and Medicare, is undergoing a substantial transformation. Transitioning from the financial alignment initiative (FAI) demonstration model used in 29 counties, it is evolving into a statewide, fully integrated dual eligible special needs plan (FIDE-SNP) model. This shift is more than procedural; it signifies a pivotal moment of transition to new federal D-SNP requirements.
Background
The MyCare Ohio Program launched in May 2014 as a Centers for Medicare & Medicaid Services (CMS) FAI demonstration. MyCare Ohio integrates Medicare and Medicaid benefits for dually eligible members enrolled in competitively selected MyCare Ohio managed care plans, providing one care coordinator and streamlined communication and services. It serves 150,000 individuals in 29 counties.
CMS is sunsetting all FAI demonstration programs on December 31, 2025, prompting ODM to convert to the FIDE-SNP model.
Next Generation RFA
The MyCare Ohio Program will convert to the Next Generation MyCare Ohio Program in January 2026. ODM is modeling portions of the program after the state’s Next Generation Medicaid managed care program. The Next Generation MyCare Ohio Program initially will be implemented in the 29 currently participating counties and then expand statewide, covering a total of 250,000 eligible individuals. Medicaid managed care organizations (MCOs) that serve the program will need to become CMS-approved FIDE-SNPs. MCOs awarded a Next Generation MyCare Ohio contract will need to notify CMS of their intent to establish a statewide FIDE-SNP in Ohio by fall 2024 to begin operations in January 2026.
ODM anticipates selecting up to four Next Generation MyCare Ohio MCOs to serve enrollees statewide, though a decision on the number of plans will be finalized as awards are made and based on what is most advantageous to the state.
MCOs will need to develop a member-focused strategy with care coordination as a priority. MCOs will also increase focus on behavioral health coordination. According to ODM, goals for the Next Generation program include:
- Focusing on the individual
- Improving individual and population wellness and health outcomes
- Creating a personalized care experience
- Supporting providers in continuously improving care
- Improving care for people with complex needs to promote independence in the community
- Increasing program transparency and accountability
Next Generation MyCare will advance these goals through a population health approach, designed to address inequities and disparities in care.
The program will enroll dually eligible individuals ages 21 and older. This is a change from the current program, which enrolls dual eligibles who are 18 years old and older. The eligible age increase is being made to align with the Medicaid early and periodic screening, diagnostic, and treatment (EPSDT) benefit.
The new program also will continue to offer all the same services available through Ohio’s home care, PASSPORT (long-term services and supports), and assisted living waivers.
Evaluation
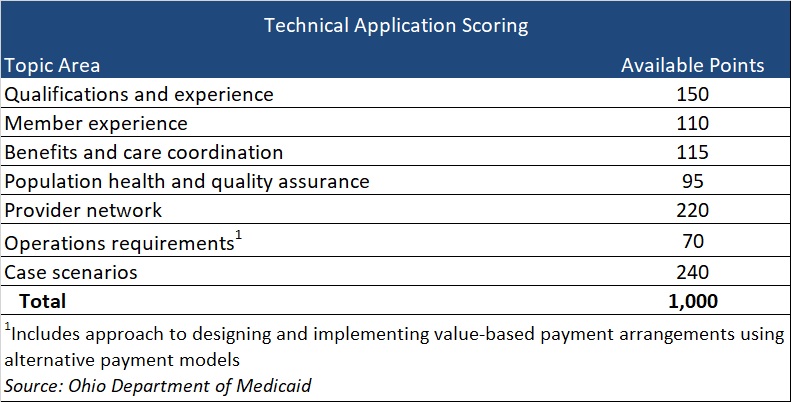
Applications initially will be reviewed to confirm the applicant meets the mandatory requirements. Applicants who meet the mandatory requirements will proceed to review and evaluation of responses to application questions that fall into seven topic areas, with a total of 1,000 available points (see Table 1). Of note, if an applicant is not currently serving as either a Next Generation MCO or a MyCare Ohio MCO, the applicant will receive zero points for qualifications and experience. Organizations that have yet to participate in at least one of these programs should consider the effect on their total score.
Table 1
Current Market
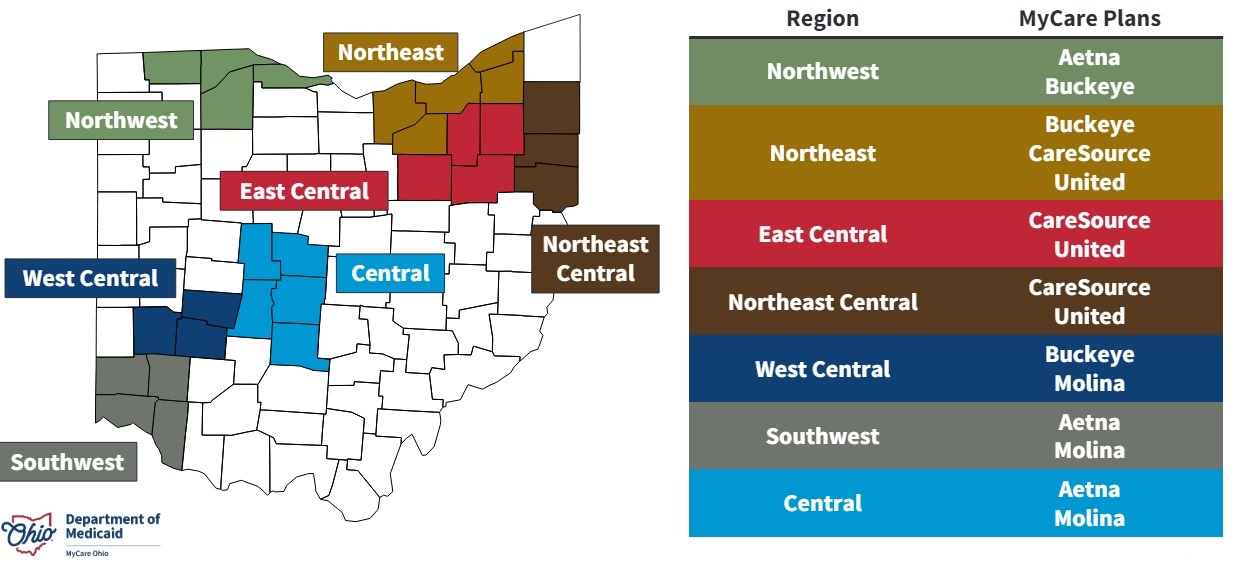
Five MCOs—CVS/Aetna, CareSource, Centene/Buckeye, Molina, and United—participate in the current MCOP, with two or three of them participating in each of the seven regions.
Timeline
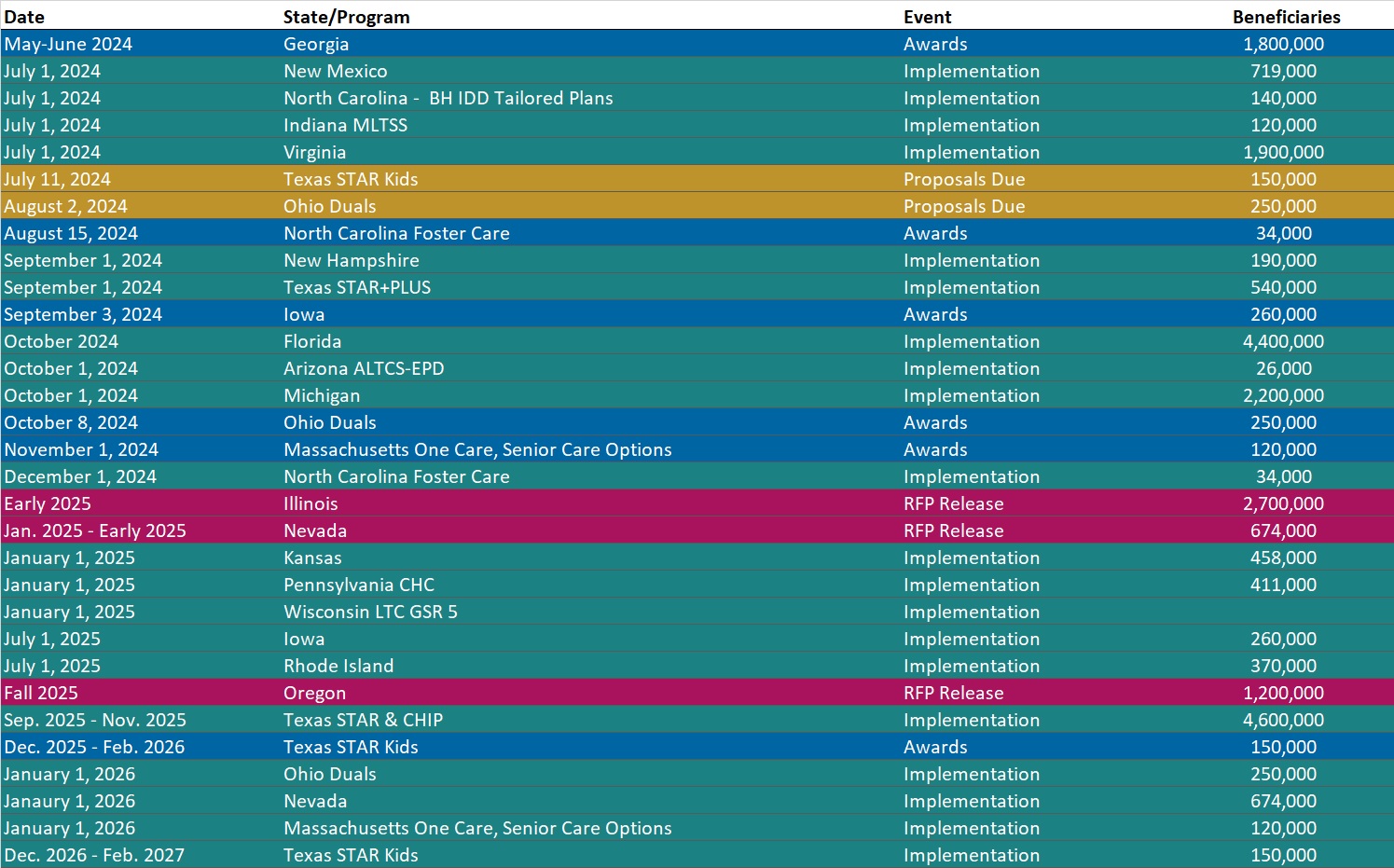
MCOs should submit a notice of intent to apply by June 21. Proposals are due August 2, and awards will be issued October 8. Implementation is scheduled for January 1, 2026.

Connect With Us
Ohio is one of several states transitioning from a FAI demonstration at the end of December 2025. Additionally, the 2025 Medicare Advantage Final Rule includes new policies affecting D-SNPs that could reshape the integrated care plan landscape in many states.
Health Management Associates (HMA) will host a webinar June 20, 2024, to review the current landscape and federal changes that will affect D-SNPs in 2025 and beyond. The session will feature an analysis of the new regulations and a discussion of the critical strategic and product impacts on Medicare organizations that offer D-SNPs or are considering offering D-SNPs. Attendees also will have the opportunity to engage with the panelists during a Q&A session.
More information on the webinar is available here. Contact HMA expert Sukey Barnum to learn more about the Ohio RFA and Holly Michaels Fischer, Greg Gierer, Dara Smith, and Tim Murray for details about the nationwide D-SNP rules and landscape.
HMA Roundup
Arkansas
Arkansas to Transition Medicaid Managed Care Dental Program Back to Fee-for-Service. The Arkansas Department of Human Services (DHS) announced on June 3, 2024, that it is ending its Medicaid managed care dental program and will return to a fee-for-service structure, which is expected to launch on November 1, 2024. Management of the program will shift to the DHS Division of Medical Services. Delta Dental of Arkansas and Managed Care of North America (MCNA) currently administer the program serving 572,047 beneficiaries. Read More
Arkansas Releases MES Procurement Support RFP. The Arkansas Department of Human Services (DHS) released on May 31, 2024, a request for proposals (RFP) for a procurement assistance contractor in anticipation of the state’s upcoming Medicaid Enterprise System (MES) Core and MES Decision Support System (DSS) procurements. The current MES Core contract ends December 1, 2028, and the current DSS contract ends July 1, 2027. Proposals are due July 10, and intent to award is anticipated for September 6. The contract will run for one year beginning on January 1, 2025, with up to six one-year renewals. Read More
Colorado
Colorado Governor Signs Bills Addressing Housing, Nutrition Support Funding, Prescription Drug Access. The Colorado State House Democrats reported on June 3, 2024, that Governor Jared Polis signed two major health-related bills into law. HB 24-1322, sponsored by Representatives Shannon Bird (D-Westminster) and Kyle Brown (D-Louisville), will redirect Medicaid funds to housing and nutrition programs. The bill requires the Colorado Department of Health Care Policy & Financing (HCPF) to pursue a Medicaid Section 1115 waiver to fund housing and nutrition services and to conduct a feasibility study to determine how Medicaid can pay for nutrition services. SB 24-110, sponsored by Senate Majority Leader Robert Rodriguez (D-Denver), prohibits HCPF from requiring prior authorization for certain antipsychotic medications. Read More
Florida
Florida CHIP Lawsuit Dismissed; Medicaid Redetermination Lawsuit Trial Date Approaches. Health Payer Specialist reported on June 3, 2024, that a judge dismissed Florida’s lawsuit against the U.S. Department of Health and Human Services over rules prohibiting states from dropping beneficiaries from the Children’s Health Insurance Plan if their parents did not pay premiums on time. Florida would have to challenge the regulations with the Centers for Medicare & Medicaid Services before filing a lawsuit. Separately, a lawsuit against the Florida Agency for Health Care Administration regarding Medicaid redeterminations is set to go to trial in late June or early July. The suit alleges Florida disenrolled adult beneficiaries without giving them proper notification. Read More
Florida Governor Signs Bill to Establish Rural Emergency Hospitals. Health News Florida reported on May 29, 2024, that Florida Governor Ron DeSantis signed a bill, sponsored by Senator Corey Simon (R-Tallahassee), that would establish the category of rural emergency hospitals in the state, consistent with federal law, which allows these hospitals to receive Medicare payments to provide emergency services, observation care, and outpatient services without providing inpatient care. The measure, which was passed unanimously by the state Legislature, will take effect July 1. Read More
Hawaii
Hawaii Receives Federal Approval to Provide Medicaid Coverage for Community Palliative Care. Hawaii News Now reported on June 4, 2024, that Hawaii has received federal approval through a state plan amendment to cover community palliative care through Medicaid. The new benefit will allow coverage for Medicaid beneficiaries with serious or terminal illnesses, including services for improving life quality and addressing physical and emotional needs. Read More
Indiana
Indiana Receives Federal Approval to Transition LTSS to Managed Care. The Indiana Capital Chronicle reported on June 4, 2024, that Indiana received federal approval for its Section 1915c Home and Community Based Services PathWays for Aging demonstration, which will transition Medicaid long-term services and supports (LTSS) to managed care, beginning July 1. Individuals served by the state’s expired Aged and Disabled Waiver that are 60 or older will be enrolled into PathWays for Aging, and individuals under the age of 60 served by that program will move to the Health and Wellness waiver. The state also received approval to pay for parental care of seriously disabled children through Structured Family Caregiving, which pays a per diem amount. Read More
Massachusetts
Massachusetts Lifts Asset Limit for the Medicare Savings Program. The Massachusetts Executive Office of Health and Human Services announced on May 31, 2024, that the Medicare Savings Program (MSP) asset limit has been lifted as of March 1. Read More
Michigan
Michigan Selects Eight PIHPs for Substance Abuse Recovery Incentives Pilot Program. The Michigan Department of Health and Human Services announced on June 4, 2024, that it approved eight pre-paid inpatient health plans (PIHPs) to participate in the Recovery Incentives Pilot, an evidence-based treatment program for substance use disorders offered by the state for Medicaid and Healthy Michigan beneficiaries. Participating PIHPs include NorthCare Network; Southwest Michigan Behavioral Health; Mid-State Health Network; Community Mental Health Partnership of Southeast Michigan; Detroit Wayne Integrated Health Network; Oakland Community Health Network; Macomb County Community Mental Health; and Region 10 PIHP. The Recovery Incentives Pilot is set to launch in October 2024 and will run for two years. Read More
BCBS-MI Names Tricia Keith President, CEO Beginning in January 2025. Health Payer Specialist reported on May 17, 2024, that Blue Cross Blue Shield of Michigan has named Tricia Keith president and chief executive, effective January 1, 2025. Keith currently serves as executive vice president, COO, and president of emerging markets for BCBS of Michigan. Read More
Minnesota
Minnesota Releases Medicaid, MinnesotaCare IHP RFP. The Minnesota Department of Human Services released on May 31, 2024, a Request for Proposals (RFP) for providers interested in participating in the state’s Integrated Health Partnerships (IHP) Demonstration, an accountable care model that serves Medicaid and MinnesotaCare. The program, which currently has 25 IHPs serving more than 530,000 beneficiaries, offers two tracks: Track 1 (non-risk) and Track 2 (upside and downside risk). Letters of intent are due August 2 and proposals are due August 14. Awards are expected September 6, 2024. Contracts will run from January 1, 2025, through December 31, 2028, and may not exceed a total of five years. Read More
Missouri
Missouri Reinstates Medicaid Premium Payments for Three Programs. Fox4 reported on May 29, 2024, that Missouri is reinstating Medicaid premiums for the Children’s Health Insurance Program, Ticket to Work Program, and the Spend Down Program. Beneficiaries must pay May invoices in order to be covered beginning June 1, and those that fail to pay the premiums will be disenrolled. Read More
Missouri Disenrolls 197,525 Medicaid Beneficiaries During Redeterminations From June Through April. Missouri Independent reported on May 31, 2024, that Missouri has disenrolled 197,525 Medicaid beneficiaries based on eligibility redeterminations from June 2023 to April 2024. Of those disenrolled, 110,938 were children. The state has nearly 18,000 pending eligibility cases as of April. Read More
Montana
Montana Owes Providers $8.5 Million in Delayed Payments Amid Medicaid Unwinding. The Daily Montanan reported on June 3, 2024, that 21 Montana healthcare facilities are owed an estimated $8.5 million in delayed Medicaid reimbursements. The delayed payments largely stem from the Medicaid redetermination process, according to a survey conducted by the Montana Healthcare Association. The average delays for processing new Medicaid applications are three to six months long and reimbursements related to new applications go back 90 days. Read More
Nevada
HMA Releases Report Examining Nevada’s MAABD Program. Nevada Medicaid released on May 30, 2024, a report by Health Management Associates (HMA) evaluating Nevada’s Medical Assistance for the Aged, Blind, and Disabled (MAABD) program, with particular focus on the long-term services and supports (LTSS) landscape, stakeholder engagement, and program recommendations. The MAABD program provides LTSS to elderly individuals or people who have physical disabilities and has faced challenges, including high costs, underfunding, and geographic gaps in services. To address these challenges, HMA recommends developing aligned short and long-term quality strategies, separating MLTSS and fully integrated dual eligible special needs (FIDE-SNP) programs for adults aged 65 or over, implementing the Program of All-Inclusive Care for the Elderly (PACE) model of care, and enrolling MAABD individuals 64 and under into Medicaid managed care contracts in 2030. Read More
New York
New York MCOs Made Medicaid Payments to Unverified Providers Totaling $1.5 Billion, Audit Finds. Crain’s New York Business reported on June 5, 2024, that five managed care organizations (MCOs) spent $1.5 billion on payments to physicians, hospitals, and pharmacies that were not vetted to be reimbursed through Medicaid, according to an audit by New York Comptroller Thomas DiNapoli. The audit, which reviewed claims from January 2018 through June 2022, also found that the MCOs paid $916 million in claims for services by in-network providers whose IDs did not match with a Medicaid enrolled provider and $833 million in claims for services by providers whose Medicaid application was denied or withdrawn. Read More
New York Senate Advances Bill to Provide Medicaid Reimbursement, Support for Emergency Medical Services. The New York State Senate reported on May 29, 2024, that it has passed a bill package to provide Medicaid reimbursements to medical service agencies for point-of-response treatment without requiring further medical evaluations. The legislation will also expand the ability of ambulances to administer life-saving blood transfusions, recognize general ambulance services as essential, and provide financial relief to New York’s emergency service first responders. Read More
North Dakota
North Dakota Completes Medicaid Redeterminations, Disenrolling 40 Percent of Beneficiaries. KFYR TV reported on June 4, 2024, that North Dakota has completed its 13-month Medicaid redetermination process, with about four in 10 Medicaid beneficiaries losing coverage. In total, the state conducted reviews for 134,000 beneficiaries. Read More
Tennessee
Tennessee Awards Medicaid Dental Contract to Renaissance Life & Health Insurance Company. Renaissance Life & Health Insurance Company of America announced on May 30, 2024, that Tennessee has awarded it a contract to serve as the statewide Medicaid Dental Benefits Manager (DBM) for five separate state DBM programs. The state’s five DBM programs cover adult and child TennCare enrollees, children enrolled in the CoverKids program, and adults with intellectual or developmental disabilities. The contract is anticipated to begin July 1, 2025. Read More
National
CMS Releases ACO Primary Care Flex Model RFA. The Centers for Medicare & Medicaid Services (CMS) released on May 30, 2024, a request for applications (RFA) for participation in the Accountable Care Organizations (ACO) Primary Care (PC) Flex Model, which is a new voluntary payment model that will focus on advanced primary care delivery for low revenue ACOs participating in the Medicare Shared Savings Program. Model participants will receive a one-time advanced shared savings payment and monthly prospective population-based payments. The ACO PC Flex Model aims to support care delivery transformation, innovation, and team-based approaches to improve quality and reduce costs of care. The model will begin on January 1, 2025. ACOs that participate will jointly participate in the Shared Savings Program. The deadline to submit an application to the Shared Savings Program is June 17, 2024. Read More
HHS Selects Ten Additional States to Participate in CCBHC Demonstration. The U.S. Department of Health and Human Services (HHS) announced on June 4, 2024, that ten additional states were selected for participation in a two-year Certified Community Behavioral Health Clinic (CCBHC) Medicaid Demonstration Program, aimed at increasing access to crisis and behavioral health care in communities. The ten states are Alabama, Illinois, Indiana, Iowa, Kansas, Maine, New Hampshire, New Mexico, Rhode Island, and Vermont. Read More
CMS Releases 2022 Quality Payment Program Performance Information. The Centers for Medicare & Medicaid Services (CMS) released on May 30, 2024, the 2022 Quality Payment Program performance information through the Medicare.gov compare tool and in the Provider Data Catalog (PDC). The Medicare.gov compare tool allows patients and caregivers to compare Medicare providers and groups on Merit-based incentive payment system (MIPS), qualified clinical data registry, and consumer assessment of healthcare providers and systems measure. The PDC includes CMS’ required reports on the final scores of MIPS-eligible clinicians, names of eligible providers in Advanced Alternative Payment Models (APMs), and the performance and names of certain APMs. The information is available for doctors, clinicians, groups, virtual groups, and Accountable Care Organizations. Read More
CMS BPCI Advanced Model Resulted in Medicare Savings Totaling $465 Million. The Centers for Medicare & Medicaid Services (CMS) reported on May 30, 2024, that the Bundled Payments for Care Improvement Advanced (BPCI Advanced) Model resulted in an estimated $465 million net savings to Medicare during Model Year 4 (2021), according to its fifth annual BPCI Advanced evaluation report. The net savings offset the combined losses in the first 3 model years, which totaled $179.5 million. BPCI Advanced is a voluntary bundled payment model that tests whether linking payments for the multiple services beneficiaries receive during an episode of care leads to improved quality of care and lower costs for Medicare. Read More
Medicaid Unwinding Shows Significant Racial Disparities in Procedural Disenrollments. The New York Times reported on June 3, 2024, that Black and Hispanic people were twice as likely as white people to lose Medicaid due to procedural reasons, such as failure to complete paperwork, during the Medicaid redetermination process, according to a study from JAMA Internal Medicine. The study did not determine whether Black and Hispanic people were more likely to lose Medicaid overall. As of May, Medicaid enrollment has declined by 13 million nationwide. Read More
Medicaid, CHIP Enrollment Drops by Nearly 655,000 in February 2024, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) reported on May 31, 2024, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was approximately 83.4 million in February 2024, a decrease of 654,280 since January 2024. Medicare enrollment was nearly 67.1 million, up 69,037 from January 2024, including nearly 33.8 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
CMS Extends State Reporting on Medicaid Renewals, Enrollment Amid Eligibility Redeterminations. The Centers for Medicare & Medicaid Services (CMS) released on May 30, 2024, a State Health Official (SHO) letter announcing that it is extending state reporting for certain Medicaid and Children’s Health Insurance Program (CHIP) metrics that states were required to report when they resumed normal Medicaid eligibility processes. Specifically, state reporting on renewal outcomes will continue after the Consolidated Appropriations Act, 2023 requirements end on June 30, 2024. Read More
Managed Care Plans in Five State’s Differ in EPSDT Service Prior Authorization Requirements, GAO Finds. The Government Accountability Office (GAO) released on May 29, 2024, a report which found that selected Medicaid managed care plans in five states had similar processes for authorizing Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) services but differed in the services requiring prior authorization. The selected plans were from the District of Columbia, Florida, Massachusetts, Missouri, and Utah. The states’ oversight of managed care plans’ prior authorizations generally included reviewing plans’ policies and processes, data collection on approval and denials, and a review of a subset of denied authorizations. The GAO has recommended that the Centers for Medicare & Medicaid Services set expectations for monitoring the appropriateness of plans’ prior authorization decisions and clarify whether managed care plans can require prior authorization for EPSDT services when the state does not have such requirements. Read More
Republican Lawmakers Introduce Legislation to Bolster Access, Transparency in 340B Drug Pricing Program. Fierce Healthcare reported on May 29, 2024, that U.S. Representative Larry Bucshon (R-IN) introduced a bill to reform the 340B Drug Discount Program, which includes new hospital eligibility requirements and transparency requirements tasking grantee organizations to reporting how savings from the discounts are being used. The bill also codifies definitions of 340B patients and contract pharmacies and will prohibit hospitals from denying 340B patients access to the medications based on their ability to pay. Read More
CMS Releases Updates to Annual Guidance on Medicaid, CHIP Core Set Reporting. The Centers for Medicare & Medicaid Services (CMS) released on May 30, 2024, a State Health Official (SHO) letter which includes updates for mandatory annual state reporting of the Core Set of Children’s Health Care Quality Measures for Medicaid and CHIP (Child Core Set) and the behavioral health measures on the Core Set of Adult Health Care Quality Measures for Medicaid (Adult Core Set). The letter includes guidance on mandatory reporting regulations; core set measures; populations and the population exemption process; stratification categories; measures subject to stratification; and annual updates to the 2025 Child and Adult Core Sets. Read More
Safety-net Clinics Cut Services, Staff Amid Medicaid Eligibility Redeterminations. KFF Health News reported on May 30, 2024, that safety-net clinics nationwide have cut services and staff amid the Medicaid eligibility redeterminations process, which has resulted in coverage termination for more than 22 million people. As a result, health centers have increasingly provided care without receiving payments. Approximately one in 10 community health centers have reduced staff and services or limited appointments. Read More
Industry News
SCAN Health Plan Wins Medicare Advantage Star Rating Lawsuit. Modern Healthcare reported on June 4, 2024, that SCAN Health Plan won a federal lawsuit that alleged the Centers for Medicare & Medicaid Services (CMS) improperly calculated SCAN’s Medicare Advantage Star ratings. The ratings are based on a curve in comparison with rival plans. SCAN took issue with the way regulators removed outlier plans from the comparison last year during a statistical update called the Tukey Outer Fence Outlier Deletion Method. The company’s rating fell from 4.5 to 3.5, causing them to lose $250 million in quality bonus payments. Read More
UnitedHealth Acquisition of Amedisys Stalls After Private Equity Firm Backs Out. Health Payer Specialist reported on June 3, 2024, that UnitedHealth Group’s proposed $3.3 billion acquisition of Amedisys has been stalled after a private equity firm reconsidered its offer to buy more than 100 locations from United. Read More
Ensign Group Acquires Skilled Nursing Facilities in Arizona, Colorado. The Ensign Group announced on June 4, 2024, that it has acquired the real estate and operations of Wellsprings of Gilbert, a 32-bed skilled nursing facility located in Gilbert, Arizona, effective June 1, 2024. Ensign also acquired the operations at The Springs at St. Andrews Village, a 58-bed skilled nursing facility located in Aurora, Colorado. Ensign now has 312 healthcare operations across 14 states. Read More
Evolent Health to Acquire AI Assets from Machinify. Evolent Health announced on June 4, 2024, that it has signed an agreement to acquire artificial intelligence utilization management products and team assets of Machinify. The agreement also includes the license for Machinify’s artificial intelligence (AI) clinical review software called Machinify Auth. Machinify currently reviews over $200 billion worth of medical claims annually using its AI technology. This acquisition is expected to close in the third quarter of 2024. Read More
PracticeTek, Total Dental Complete Acquisition of Ora. PracticeTek, a healthcare technology solutions provider, announced on June 3, 2024, that it has finalized its acquisition of Ora, in collaboration with Total Dental. Ora is an all-in-one dental practice management platform. Read More
Solarity Announces Strategic Growth Investment from Private Equity Firm TA Associates. Solarity, a solutions provider for acute and ambulatory healthcare providers, announced on June 4, 2024, that it has received a strategic growth investment from private equity firm TA Associates. TA Associates will be the new lead investor, joining Solarity’s existing private equity partner BV Investment Partners. Financial terms of the transaction were not disclosed. Read More
LaVie Care Centers Files for Chapter 11 Bankruptcy Protection. Modern Healthcare reported on June 3, 2024, that Atlanta-based LaVie Care Centers, which operates 43 skilled nursing facilities across five states, filed for Chapter 11 bankruptcy protection. The company listed between $500 million and $1 billion in assets and between $1 billion and $10 billion in liabilities in its filing. The company plans to continue operating its current portfolio of nursing homes in Mississippi, North Carolina, Pennsylvania, Virginia, and Florida. Read More
HHS to Require UnitedHealth to Disclose Data Related to Cyberattack. Modern Healthcare reported on May 31, 2024, that the U.S. Department of Health and Human Services will require UnitedHealth Group to inform people about privacy breaches resulting from the Change Healthcare cyberattack under the Health Insurance Portability and Accountability Act (HIPAA). UnitedHealth will need to disclose what data was compromised, how the company responded to the attack, how the company can be contacted, and what individuals can do to protect themselves, if requested by affected entities. Read More
UnitedHealth Forecasts Potential Disruption in Medicaid Program Following Redeterminations. Fierce Healthcare reported on May 31, 2024, that UnitedHealth forecasted a disruption in its Medicaid business after noting a potential inconsistency between patient utilization and rate payments at an investor conference. Concerns are partially due to the impact of redeterminations; UnitedHealth has not attributed any upcoming issues to the Change Healthcare cyberattack. Read More
DOJ Opposes Steward Health Care’s Bankruptcy Plan. Modern Healthcare reported on May 30, 2024, that the U.S. Department of Justice (DOJ) has objected to Steward Health Care’s proposed bankruptcy plan, stating that it needs additional time to review the sale of Steward’s assets. The plan would allow Steward to borrow up to $300 million from Medical Properties Trust and sell all its assets. The DOJ has expressed concern that the plan, particularly Optum’s bid to purchase the company, does not allow enough time for a full antitrust review. Read More
HouseWorks Acquires AccordCare’s Connecticut Personal Care Division. HouseWorks Holdings, a northeast-based personal care services platform, announced on May 29, 2024, that it has acquired the Connecticut Personal Care division of AccordCare, a national provider of home care and certified home health. The Connecticut Personal Care Division, which includes Companions and Homemakers as well as Companions Forever, will retain respective branding. Combined, these brands are the largest provider of Medicaid home care services in Connecticut. Read More
RFP Calendar
Company Announcements
MCG Announcement:
MCG Thought Leaders to Explore AI’s Role in Streamlining Prior Authorization at AHIP 2024. MCG Health, part of the Hearst Health network, has announced that two of its health IT experts will be featured speakers at the upcoming AHIP 2024 conference. Their June 11 session will discuss the appropriate use of artificial intelligence (AI) in prior authorization processes as well as insights from the recent CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F). Read More
HMA News & Events
HMA Webinars:
Medicare Physician Fee Schedule Reform – Structural Topics and Recommendations. Thursday, June 13, 2024, 12 PM ET. HMA recently released a report on the Medicare Physician Fee Schedule (PFS) with background on the structure of the program, and recommendations for reforms that could be considered. We’d like to invite you to a webinar that will provide background and context about the PFS for interested parties who may be less familiar with the payment system and why the stakeholder community got to the point of needing to “fix” the fee schedule. We will discuss pressing policy and payment concerns, provide an overview of key structural issues within the PFS that should be considered and balanced when making policy changes to the payment system, highlight different stakeholder perspectives, and offer recommendations within CMS authority. Register Here
D-SNP Growth and Integration: Key Implications of the 2025 CMS Final Rule. Thursday, June 20, 2024, 11 AM ET. Join us for an informative webinar where HMA experts will review the upcoming changes from the 2025 Final Rule that will impact Dual Special Needs Plans (D-SNPs) in 2025 and beyond. The session will feature an analysis of the new regulations and a discussion of the critical strategic and product impacts on Medicare organizations offering D-SNPs or considering offering D-SNPs. Attendees will also have the opportunity to engage with the panelists during a Q&A session. Don’t miss this chance to stay informed and ahead of the curve with expert guidance from HMA. Register Here
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
- Updated Section 1115 Medicaid Demonstration Inventory
- Updated Illinois State Overview
- Updated Utah State Overview
Medicaid Data
Medicaid Enrollment:
- California Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- California SNP Membership at 543,503, Mar-24 Data
- Delaware SNP Membership at 19,663, Mar-24 Data
- Hawaii Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Illinois Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Kansas Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Maryland Medicaid Managed Care Enrollment Is Down 1.7%, Feb-24 Data
- Massachusetts Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Michigan Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Minnesota Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Mississippi Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Missouri Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Montana Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Oklahoma Medicaid Enrollment is Down 4.5%, Feb-24 Data
- Utah Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Utah SNP Membership at 28,049, Mar-24 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Arkansas MES Procurement Support RFP, May-24
- Minnesota Integrated Health Partnerships (IHP) Demonstration RFP and Appendices, May-24
- Ohio Next Generation MyCare RFA, May-24
Medicaid Program Reports, Data, and Updates:
- Indiana HCBS Pathways for Aging Program 1915c Waiver Documents, 2023-24
- Nevada Medicaid ABD Program Analysis Project, May-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
