HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: More than 20 Medicaid, Medicare, Marketplace Plan Executives Are Confirmed Speakers at 2023 HMA Conference

- Medicaid, CHIP Enrollment is Nearly 93.9 Million in March 2023

- Medicaid Disenrollment News: Connecticut, Michigan, North Carolina, Oregon, South Carolina

- California Renews Managed Care Tax, With Funds to Bolster Medicaid, Hospitals

- Georgia Directs $118 Million to Medicaid Expansion in Fiscal 2024

- Idaho Awards Centene/Magellan Healthcare Behavioral Health Plan Contract

- Illinois Governor Creates State-based Insurance Exchange

- Illinois Requests Extension for Behavioral Health Transformation Section 1115 Waiver

- New Hampshire Extends Postpartum Medicaid Coverage

- Washington Extends Family Planning Only Demonstration Waiver by One Year

- Wisconsin to Renew Family Care, Family Care Partnership Waivers

- Wisconsin Launches Independent Living Supports Pilot Program

- MACPAC Projects Medicaid Managed Care Directed Payment Spending to Be $69.3 Billion Annually

- Drug Makers File Federal Lawsuit to Block Medicare From Negotiating Drug Prices

- UnitedHealth Group Wins Bidding Showdown to Acquire Amedisys

- CareSource to Acquire Radiant Alliance

In Focus
More than 20 Medicaid, Medicare, Marketplace Plan Executives Are Confirmed Speakers at 2023 HMA Conference
C-suite executives from AmeriHealth Caritas, Centene, Community Health Choice of California, Health Care Service Corp., Humana, UnitedHealthcare, and UMPC Health Plan are scheduled to speak on trends in publicly sponsored healthcare at HMA’s Sixth Annual Conference, October 30-31 in Chicago.
They join keynote speaker Alan Weil, editor-in-chief of Health Affairs, and other experts in addressing innovation, value, equity, and growth opportunities and challenges facing Medicaid, Medicare, and Marketplaces across multiple and varied plenary, breakout, and panel sessions. See below for a list of confirmed speakers to date.
The conference also will feature a preconference workshop on October 29, during which HMA behavioral health leaders will address national trends and challenges for system redesign and serving complex populations. Participants will work on solving provider and population challenges during group activities.
We’re excited to welcome hundreds of attendees from health plans, providers, state and federal government, investment firms, and community-based organizations to enjoy top-notch content, interface with leading experts, make new connections, and garner fresh ideas and best practices. Last year’s event drew more than 500 healthcare professionals.
Early bird registration ends July 31.
Confirmed Speakers to Date
Keynote Speaker
Alan Weil, Editor-in-Chief, Health Affairs
Managed Care Speakers to Date (in alphabetical order)
Karen Dale, Chief Diversity, Equity, and Inclusion Officer, AmeriHealth Caritas
Mitchell Evans, Market Vice President, Policy & Strategy, Medicaid & Dual Eligibles, Humana
John Lovelace, President, Government Programs, Individual Advantage, UPMC Health Plan
Eric Mattelson, Chief Actuary, Zing Health
Anne Rote, Medicaid President, Health Care Service Corp.
Tim Spilker, CEO, UnitedHealthcare Community & State
David Thomas, CEO, Markets & Medicaid, Centene
Jaimie White, SVP, Medicaid Operations, Humana
Lisa Wright, President and CEO, Community Health Choice
State Medicaid Directors to Date (in alphabetical order)
Jacey Cooper, State Medicaid Director, Chief Deputy Director for Health Care Programs, California Department of Health Care Services
Kelly Cunningham, Medicaid Administrator, Division of Medical Programs, Illinois Department of Healthcare and Family Services
Drew Snyder, Executive Director, Mississippi Division of Medicaid
Stacie Weeks, Administrator/Medicaid Director, Nevada Department of Health and Human Services Division of Health Care Financing and Policy
Healthcare, Provider, Policy Leaders to Date (in alphabetical order)
Richard Ayoub, CEO, Project Angel Food
Lynn Carr, Chief, Agency Operations, Medical Care Services, County of San Diego Health and Human Services Agency
Liz Goodman, Chief Legal and Public Affairs Officer, Commonwealth Care Alliance
Jesse Hunter, Operating Partner, Welsh, Carson, Anderson & Stowe
Monica Johnson, Director of the 988 & Behavioral Health Crisis Coordinating Office, SAMHSA
Peter Lee, Health Care Policy Catalyst; former Executive Director, Covered California
Kate Massey, Executive Director, MACPAC (Medicaid and CHIP Payment and Access Commission)
Julie Morita, MD, Executive Vice President, Robert Wood Johnson Foundation
Bryan Buckley, Director for Health Equity Initiatives, National Committee for Quality Assurance
James R. Stringham, VP/CEO. Banner Government Health Plans, Banner Health
HMA offers attractive group rates and government discounts as well as sponsorship opportunities that help strengthen brand awareness and provide invaluable exposure and access to healthcare sector leaders. Visit the conference website for a complete list of sponsorship opportunities.
Contact Carl Mercurio for details.
[email protected]
(212) 575-5929
HMA Roundup
California
California Renews Managed Care Tax, With Funds to Bolster Medicaid, Hospitals. Politico reported on June 24, 2023, that California Governor Gavin Newsom reached an agreement with lawmakers to renew a tax on managed care organizations, with the funds to be used to bolster Medicaid and hospitals. The tax is expected to generate $19 billion, plus billions more in matching federal funds. The original tax expired in 2022. Read More
Connecticut
Connecticut Disenrolls 46,000 Medicaid Beneficiaries Following May Redeterminations. CT News Junkie reported on June 26, 2023, that Connecticut disenrolled more than 46,000 Medicaid beneficiaries following May redeterminations. About a third of the disenrolled membership have enrolled in coverage through the state Exchange or the Covered Connecticut premium assistance program. Read More
Delaware
Delaware Senate Approves Additional $49 Million for Fiscal 2024 to Address Growth in Medicaid Expenditures. The Associated Press reported on June 28, 2023, that the Delaware Senate passed the fiscal 2024 operating budget, which includes an additional $48.7 million to address the expected growth in Medicaid expenditures. A supplemental bill also includes $69.1 million in one-time funding for Medicaid. The budget package now goes to Governor John Carney for his signature. Read More
District of Columbia
DC Council Considers Bill to Require Medicaid Coverage of Infertility Treatment. The Washington Post reported on June 27, 2023, that the DC Council is considering a bill that would require Medicaid to cover the infertility treatment and diagnosis, three rounds of in vitro fertilization, and medical costs related to an embryo transfer to a surrogate. The Council passed the bill, but needs to vote again on a technical amendment before it goes to Mayor Muriel Bowser for her signature. The measure also requires federal regulatory approval. Read More
Georgia
Georgia Directs $118 Million to Medicaid Expansion in Fiscal 2024. The Georgia Budget and Policy Institute (GBPI) reported on June 27, 2023, that the Georgia fiscal 2024 budget directs about $118 million in total state funds to Pathways to Coverage, the state’s Medicaid expansion program for individuals up to 100 percent of poverty who meet certain work requirements. The funding will cover about 47,500 expansion members, GBPI says. In contrast, GBPI notes, a full expansion to 500,000 eligible individuals up to 138 percent of poverty would cost the state 80 percent less per person. Read More
Idaho
Idaho Awards Centene/Magellan Healthcare Behavioral Health Plan Contract. The Idaho Department of Health and Welfare announced on June 27, 2023, that it has awarded Centene/Magellan Healthcare the Idaho Behavioral Health Plan (IBHP) contract, worth $1.2 billion. The new contract will integrate inpatient, residential, and outpatient behavioral health services into a single comprehensive behavioral plan and serve 425,000 Medicaid and non-Medicaid members. Currently IBHP is a pre-paid ambulatory health plan served by United’s Optum. The contract will run for four-years. United/Optum and Elevance/Beacon Health also bid for the contract. Read More
Illinois
Illinois Requests Extension for Behavioral Health Transformation Section 1115 Waiver. The Centers for Medicare & Medicaid Services (CMS) announced on June 28, 2023, that Illinois submitted an extension application for the five year renewal of the Behavioral Health Transformation Section 1115 Demonstration Waiver. The goals of the waiver are to improve Medicaid services for substance use disorder and address structural factors affecting behavioral health outcomes. The extension would be effective July 1, 2023, through December 31, 2023, while Illinois works towards approval of the five year renewal. The state has requested that the waiver, previously approved by CMS in 2018, be renamed the “Illinois Healthcare Transformation Section 1115 Demonstration.” The federal public comment period will be open from June 28, 2023, through July 28, 2023. Read More
Illinois Governor Creates State-based Insurance Exchange. WQAD/Capitol News Illinois reported on June 27, 2023, that Illinois Governor JB Pritzker signed House Bill 579 to create a state-based health insurance Exchange. The legislation also gives the state Department of Insurance the authority to modify or reject proposed rate increases. Under the plan, an initial version would be operational on the federal platform by plan year 2025, with a final version on a state-based platform ready for the 2026 plan year. Read More
All Kids Misclassifies About 5 Percent of Undocumented Enrollees, Audit Finds. Health News Illinois reported on June 26, 2023, that the Illinois Children’s Health Insurance Program (CHIP) All Kids misclassified about five percent of undocumented enrollees, resulting in lost federal funds of at least $8.2 million between fiscal 2019 and 2022, according to a state Auditor General report. All Kids spent another $1.2 million on services for 1,328 ineligible individuals between 2018 and 2020. Read More
Kansas
Kansas Overpaid Medicaid MCOs $1.3 Million from 2019 to 2021, Audit Finds. The Kansas Reflector reported on June 21, 2023, that the Kansas Department of Health and Environment overpaid Medicaid managed care organizations (MCOs) more than $1.3 million, according to an audit from the state Office of the Medicaid Inspector General. The audit found that the state did not properly process beneficiaries who moved out of state, which led to the overpayments. The timeframe for the audit was January 1, 2019, through December 31, 2021. Read More
Maine
Maine Senate Rejects Bill to Extend Medicaid Coverage to Eligible Noncitizen Adults. The Sun Journal reported on June 27, 2023, that the Maine Senate rejected a bill, passed by the House, to extend Medicaid coverage to all eligible adults, regardless of immigration status. The bill, LD 199, was sponsored by House Speaker Rachel Talbot Ross (D-Portland). Maine previously provided public health benefits to noncitizens until 2011. Lawmakers recently extended Medicaid coverage to pregnant individuals and children under age 21 who are noncitizens. Read More
Michigan
Michigan Offers One Month Grace Period to Reenroll in Medicaid Following June Redeterminations Period. The Detroit Free Press reported on June 23, 2023, that Michigan will give Medicaid beneficiaries a one-month grace period until July 31 to re-enroll in the program following June redeterminations. The additional time will benefit nearly 218,000 beneficiaries who had a June 30 deadline. Read More
New Hampshire
New Hampshire Extends Postpartum Medicaid Coverage. New Hampshire Public Radio reported on June 26, 2023, that New Hampshire will extend postpartum Medicaid coverage from 60 days to 12 months through a provision in the enacted state budget. The budget also includes provisions requiring Medicaid to cover doulas, lactation services, and donor breastmilk; provide funding for family resource centers; and expand mental health services for young kids. Read More
New Jersey
New Jersey Legislature Considers Amended Bill Requiring Medicaid Reimbursement for Behavioral Health Services in Schools. The New Jersey Spotlight News reported on June 27, 2023, that the New Jersey legislature is considering an amended bill that would require Medicaid reimbursement for behavioral services offered to eligible students in schools, regardless of participation in individualized education plans (IEP) or if the services are free to the general student population. The bill, originally introduced last year in the Assembly Appropriations Committee and amended this month, is sponsored by Assembly members Louis Greenwald (D-Burlington), Angelica Jimenez (D-Bergen), and Reginald Atkins (D-Union). Read More
North Carolina
North Carolina Could Disenroll 300,000 Medicaid Members Following Redeterminations. Insurance Newsnet reported on June 26, 2023, North Carolina could disenroll 300,000 Medicaid beneficiaries following eligibility redeterminations. The state began the redeterminations process on April 1. Read More
Northern Mariana Islands
Northern Mariana Islands Remains Short of Medicaid Funding. Marianas Variety reported on June 22, 2023, that the Commonwealth of the Northern Mariana Islands (CNMI) needs to allocate $7.8 million to generate enough federal Medicaid matching funds to continue medical coverage through September. CNMI already suspended coverage of dental, outpatient physical therapy, and home health aides, effective June 1. Read More
Oregon
Oregon to Disenroll 24,000 Medicaid Beneficiaries During June Redeterminations. The Lund Report reported on June 26, 2023, that Oregon will disenroll about 24,000 Medicaid beneficiaries during June redeterminations, the first month the state is disenrolling beneficiaries. According to state officials, about 80 percent of beneficiaries are expected to remain enrolled at the end of the redeterminations process. Read More
South Carolina
South Carolina Awards $45.5 Million in Behavioral Health Crisis Stabilization Grants to 13 Hospitals. The South Carolina Department of Health and Human Services announced on June 27, 2023, the award of $45.5 million to 13 hospitals, with funds earmarked for building specialized hospital-based emergency department units dedicated to behavioral health. The funding comes from the state’s behavioral health crisis stabilization grant program, which was announced in March. Read More
South Carolina Disenrolls 118,313 Medicaid Members During May Redeterminations. The South Carolina Department of Human Services announced on June 9, 2023, that South Carolina disenrolled 118,313 Medicaid beneficiaries following May eligibility redeterminations. About 95 percent were disenrolled for procedural reasons. Read More
Washington
Washington Extends Family Planning Only Demonstration Waiver by One Year. The Washington State Health Authority announced on June 27, 2023, that federal regulators have extended the Washington Family Planning Only (FPO) 1115 demonstration waiver through June 30, 2024, pending review by the Centers for Medicare & Medicaid Services (CMS) of the state’s application for a five-year renewal. FPO covers a preventive family planning visits, cervical cancer screenings, and reproductive health services. Income eligibility is 260 percent of the federal poverty level. Read More
Vermont
Vermont Legislature Overrides Governor’s Veto of Budget. The Brattleboro Reformer reported on June 21, 2023, that the Vermont legislature overrode Governor Phil Scott’s vetoes of a budget bill, which includes Medicaid rate increases and investments in housing and childcare. Read More
Wisconsin
Wisconsin to Renew Family Care, Family Care Partnership Waivers. The Wisconsin Department of Health Services (DHS) announced on June 27, 2023, that it is seeking renewal for the state’s Family Care and Family Care Partnership Section 1915 waivers, which provide Medicaid managed long-term care and long-term services and supports for the aged and disabled. The waivers are expected to take effect in January 1, 2025, and last for five years. Current incumbents serving the Family Care program are Community Care, Inclusa, Lakeland Care, and My Choice Wisconsin, and serving Family Care Partnership are Community Care, Humana/iCare, and My Choice Wisconsin. DHS will gather stakeholder input this year and hold a 30-day public comment period in June 2024. The proposed waiver renewals are expected to be summitted to the Centers for Medicare & Medicaid Services in September 2024. Read More
Wisconsin State Assembly Considers Bill to Extend Postpartum Medicaid Coverage. WTMJ reported on June 24, 2023, that the Wisconsin State Assembly is considering bipartisan legislations attached to the state budget bill to extend postpartum Medicaid coverage from 60 days to 12 months. The State Assembly is expected to vote on the budget in July. Read More
Wisconsin Launches Independent Living Supports Pilot Program. The Wisconsin Department of Health Services announced on June 22, 2023, the launch of the Independent Living Supports Pilot program, which will use funding from the American Rescue Plan Act to provide eligible individuals with the resources they need to stay in their homes instead of a long-term care facility. Enrollees will have access to the benefits for up to 12 months. The program will be available in 16 counties. Read More
Wisconsin Legislature Rejects Extension of Medicaid Postpartum Coverage to One Year. The Milwaukee Journal Sentinel reported on June 22, 2023, that the Wisconsin Joint Committee on Finance voted against extending Medicaid postpartum coverage from two months to one year. The proposal would have expanded Medicaid postpartum coverage to approximately 5,000 women annually. Read More
National
Medicaid, CHIP Enrollment is Nearly 93.9 Million in March 2023. The Centers for Medicare & Medicaid Services (CMS) announced on June 27, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was nearly 93.9 million in March 2023, an increase of 494,664 from February 2023. Medicare enrollment was more than 65.7 million, up 99,194 from February 2023, including nearly 31.8 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
U.S. Lawmakers Urge CMS to Expand Proposed Rule to Streamline Prior Authorizations in Medicaid, Medicare, Exchange Plans. HealthLeaders reported on June 23, 2023, that a bipartisan group of 294 lawmakers is urging federal regulators to expand a proposed rule to streamline prior authorization in Medicaid, Medicare Advantage, and Exchange plans. In a letter commenting on the proposed rule, lawmakers called for electronic prior authorizations for routine services, requiring plans to respond to prior authorization requests within 24 hours for urgent care, and requiring detailed transparency metrics. Read More
MACPAC Projects Medicaid Managed Care Directed Payment Spending to Be $69.3 Billion Annually. The Medicaid and CHIP Payment and Access Commission (MACPAC) projected in a June 2023 issue brief that annual directed payments in Medicaid managed care will be $69.3 billion for the 249 distinct arrangements approved as of February 2023. Directed payment arrangements are available in 40 states, District of Columbia, and Puerto Rico. Read More
Study Finds Geographic Disparities in Medicaid Access to Opioid Addiction Medication. A JAMA study published on June 23, 2023, found geographic disparities in Medicaid access to opioid addiction medication. For example, 75 percent to 80 percent of Medicaid patients in New England received opioid addiction medication, compared to less than 40 percent of patients in the Midwest and South. About 55 percent of Medicaid enrollees received opioid addiction medication nationally. Read More
Lawmakers Seek Approval of Rule Extending Medicaid, CHIP, Exchange Coverage to DACA Recipients. The Hill reported on June 23, 2023, that 80 Democratic lawmakers have asked federal regulators to approve and implement a proposed rule that would allow individuals in the Deferred Action for Childhood Arrivals (DACA) to access Medicaid, Children’s Health Insurance Program (CHIP), and Exchange coverage. The request, made in a letter as part of the rule’s public comment period, asks the Centers for Medicare & Medicaid Services (CMS) to implement the rule November 1, 2023. Read More
Biden Issues Executive Order to Strengthen Access to Contraception. On June 23, 2023, President Biden issued an executive order aimed at strengthening access to contraception, including the potential for new initiatives that cover family planning services and supplies through state Medicaid programs and through Medicaid managed care. The order also aims to improve access for women of reproductive age with disabilities on Medicare and for others in federal healthcare programs. Read More
Home Health Act of 2023 Would Reduce CMS Rate Setting Power. Home Health Care News reported on June 22, 2023, that Senators Debbie Stabenow (D-MI) and Susan Collins (R-ME) introduced the Preserving Access to Home Health Act of 2023, which would block cuts to home health payments beginning in 2024 and reduce the rate setting power of the Centers for Medicare & Medicaid Services (CMS). CMS has already reduced home health payments by 3.9 percent and is expected to propose the same percentage cut this summer. Read More
House Panel Holds Hearing Over Future of MIPS. CQ reported on June 22, 2023, that a House panel held an initial hearing on the future of the Medicare Merit-Based Incentive Payment System (MIPS). Members of the House Energy and Commerce Oversight and Investigations subcommittee questioned the efficacy of MIPS. Separately, the Medicare Payment Advisory Commission has already recommended that MIPS be eliminated. Read More
CMS Issues Guidance on Adults With IDD Supported by Aging Caregivers. Disability Scoop reported on June 22, 2023, that the Centers for Medicare & Medicaid Services (CMS) issued guidance aimed at helping states better serve adults with intellectual and developmental disabilities (IDD) who are supported by aging caregivers. Suggestions include outreach to caregivers, taking advantage of waiver opportunities, and utilizing the Social Security’s Disabled Adult Child program to forecast the need for home and community-based services. Of the 7.43 million individuals with IDD in the U.S., only 21 percent were receiving services as of 2018. Read More
CMS Proposes Program to Speed Medicare Coverage for Breakthrough Devices. STAT reported on June 22, 2023, that the Centers for Medicare and Medicaid Services (CMS) has proposed a voluntary program called Transitional Coverage for Emerging Technologies (TCET), which would accelerate approval of Medicare coverage for breakthrough medical devices to no more than six months following approval by the Food and Drug Administration (FDA). The public will have 60 days to comment on the proposal. Read More
Drug Makers File Federal Lawsuit to Block Medicare From Negotiating Drug Prices. Reuters reported on June 21, 2023, that the Pharmaceutical Research and Manufacturers of America joined two other pharmacy trade groups in filing a federal lawsuit to block Medicare from negotiating drug prices. The other groups are the National Infusion Center Association and the Global Colon Cancer Association. This is the fourth lawsuit challenging the law. Read More
Industry News
FTC Proposes Stronger Regulations for Mergers, Acquisitions. Modern Healthcare reported on June 27, 2023, that the Federal Trade Commission (FTC) released a proposed rule that would increase regulations on companies looking to merge. The rule proposes requiring merging parties to disclose minority investors, information on prior acquisitions, supplier agreements, subsidies from foreign entities, and workforce data. Read More
InTandem Capital Partners Forms Pediatric Dentistry, Orthodontic Company. InTandem Capital Partners announced on June 27, 2023, the creation of beBright, comprised of 17 pediatric dentistry and orthodontic offices in Minnesota, Nebraska and Tennessee. Read More
Comvest Partners Acquires Your Behavioral Health. Comvest Partners announced on June 27, 2023, the acquisition of Your Behavioral Health, a California-based behavioral health provider with 17 facilities in Southern California. Read More
UnitedHealth Group Wins Bidding Showdown to Acquire Amedisys. Health Payer Specialist reported on June 26, 2023, that UnitedHealth Group has reached an agreement to acquire Amedisys for $101 per share. Amedisys had previously agreed to be acquired by Option Health Care for $97.38 per share. The acquisition still needs shareholder and regulatory approvals. Read More
Hospital-At-Home Initiatives, Partnerships Continue to Grow. Modern Healthcare reported on June 22, 2023, that hospital-at-home model initiatives and partnerships continue to grow. The Centers for Medicare & Medicaid Services (CMS) stated that 283 hospitals in 37 states have been approved for hospital-at-home programs, which provide acute care services at home. Many hospitals are partnering with outside providers to implement the programs. Read More
CareSource to Acquire Radiant Alliance. Health Payer Specialist reported on June 22, 2023, that CareSource plans to acquire not-for-profit Radiant Alliance, which provides hospice and housing to elderly individuals. Radiant is a new entity being formed by Metta Healthcare’s Ohio Hospice, Pure Healthcare, and United Church Homes. Read More
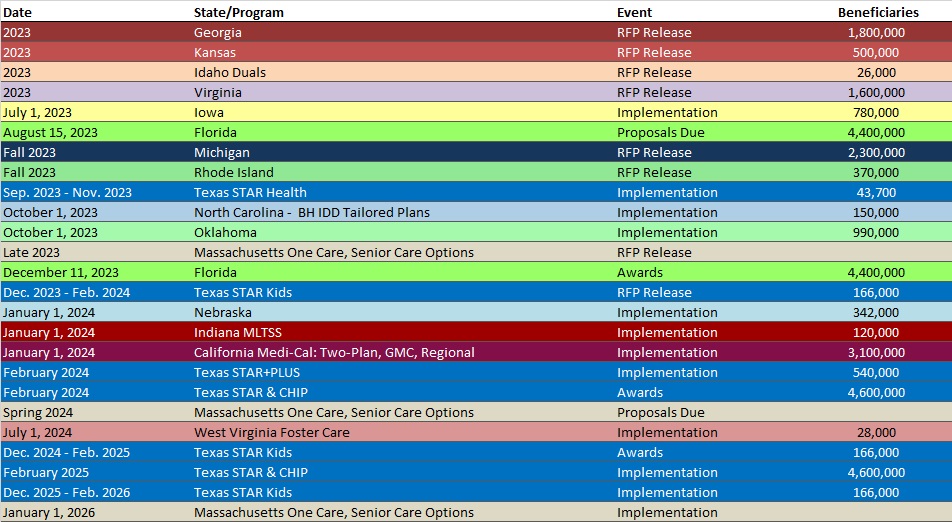
RFP Calendar
Company Announcements
AbsoluteCare Announcement:
Dr. Jerome Adams Joins AbsoluteCare’s Board of Directors. AbsoluteCare, a concierge, PCP-driven care model serving the most medically complex and compromised members, is pleased to welcome the 20th Surgeon General of the United States, Dr. Jerome Adams, to our board. Read More
MCG White Paper:
Early Detection and Prevention of Behavioral Health Conditions in Children and Adolescents. Learn about the prevalence of mental illness among children and adolescents and the long-term benefits of early intervention for initial episodes of psychosis. Download it here
MCG Press Release:
MCG, Regence, and MultiCare Connected Care Receive 2023 KLAS Points of Light Award. MCG Health, Regence Health Plans, and MultiCare Connected Care, were recently recognized by KLAS with the 2023 Points of Light award for their innovative collaboration which produced a scalable, prior authorization automation workflow based on the HL7 Da Vinci Project’s implementation guides. Read More
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Colorado SNP Membership at 58,325, Mar-23 Data
- Florida SNP Membership at 492,683, Mar-23 Data
- Idaho SNP Membership at 16,673, Mar-23 Data
- Indiana SNP Membership at 117,269, Mar-23 Data
- Louisiana SNP Membership at 149,560, Mar-23 Data
- Michigan SNP Membership at 119,668, Mar-23 Data
- Mississippi SNP Membership at 92,286, Mar-23 Data
- Missouri SNP Membership at 100,432, Mar-23 Data
- Montana SNP Membership at 4,952, Mar-23 Data
- North Dakota SNP Membership at 223, Mar-23 Data
- Puerto Rico SNP Membership at 312,645, Mar-23 Data
- South Carolina Medicaid Managed Care Enrollment is Up 2.6%, May-23 Data
- South Carolina Dual Demo Enrollment is Down 10.6%, Apr-23 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 2.5%, May-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Massachusetts MassHealth ACO RFR, Award, Responses, and Scoring, 2022
- Minnesota Medicaid Families, Children Medical Assistance and MinnesotaCare in Greater Minnesota RFP, Awards, Proposals, and Scoring, 2022
- Minnesota Senior Health Options (MSHO) and Minnesota Senior Care Plus (MSC+) RFP, Awards, Proposals, and Scoring, 2021-22
- Puerto Rico External Quality Review Organization RFP, Awards and Scoring, 2021-22
- Puerto Rico Medicaid Enterprise Project Management Office RFO, Proposals, Scoring, and Award, 2022
- Puerto Rico MES MMIS Phase III RFP, Proposals, Scoring, and Award, 2021
Medicaid Program Reports, Data, and Updates:
- Illinois Covering All Kids Performance Audit, Jun-23
- Kansas OMIG Medicaid Performance Audit, Jun-23
- Kentucky PHE Medicaid Unwinding Monthly Report to CMS, May-23
- Massachusetts PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- Missouri CHIP and SMHB Annual Reports, 2016-22
- Oklahoma PHE Medicaid Redeterminations Monthly Report to CMS, Apr-23
- Pennsylvania Managed Care External Quality Review Reports, 2022
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Jun-23
- Pennsylvania MLTSS Subcommittee Meeting Materials, 2021-23
- Pennsylvania Physical HealthChoices Databooks, CY 2018-24
- South Carolina PHE Medicaid Redeterminations Monthly Reports to CMS, May-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
