HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Report Outlines Opportunities to Strengthen Behavioral Health Workforce

- California Medicaid Doctors Introduce Ballot Measure for Higher Pay

- Idaho to Release Dual Eligible, LTSS Managed Care Procurement in June 2024

- Illinois Governor Signs Medicaid Omnibus Bill

- Michigan Releases HIDE SNP RFP to Transition MI Health Link Dual Demo

- New Mexico Medicaid to Reimburse Tribal Community Health Workers

- Oregon Receives Federal Approval to Establish Basic Health Program

- Rhode Island Submits Addendum Request to Section 1115 Comprehensive Demonstration for HRSN Services

- Texas HHSC Rejects Protests Over Medicaid, CHIP Awards

- Texas Medicaid Application Delays May Cost State Millions in Federal Funding

- MACPAC Releases June 2024 Report to Congress

- Insurers Estimate $1.1 Billion in MLR Rebates Across Commercial Markets in 2024

- Addus HomeCare Signs Agreement to Acquire Gentiva Personal Care

- Elevance Wins Medicare Advantage Star Rating Lawsuit

- Judge Blocks DOJ from Dismissing Humana Medicare Advantage Lawsuit

- Judge Denies FTC Injunction to Block Novant Health’s Acquisition of North Carolina Hospitals

In Focus
Report Outlines Opportunities to Strengthen Behavioral Health Workforce
This week, our In Focus section highlights a report that the Center for Workforce Solutions (CWS) released on May 28, 2024, titled Crosswalk of National Behavioral Health Workforce Recommendations. CWS is a partnership between the National Council for Mental Wellbeing (National Council), Health Management Associates (HMA), and the College for Behavioral Health Leadership (CBHL), which is focused on advancing actionable strategies to address the shortage of mental health and substance use treatment workers.
Overview
Nationally, the demand for mental health and substance use treatment exceeds workforce capacity to deliver services. Payment, clinical, and regulatory models underlie what has become a national behavioral health workforce crisis. The CWS is invested in creating a national platform that supports cross-sector partners working at multiple levels of the system to collaboratively address the recommendations outlined in the report to achieve meaningful improvements in the delivery of behavioral health services. The report serves to elevate workforce solutions that exist and can be scaled as well as used to build the pathways for overcoming barriers to implementation.
The Framework for Driving Action
The CWS has created a framework for multisystemic levers of change (see Figure 1) required to drive action and has cross-walked more than 400 recommendations from published reports by federal and state policymakers, national associations, foundations, and other partners. Every action and step needs to be considered, designed, and implemented through an equity lens to ensure all people with behavioral health conditions have their needs met. These recommendations, organized by the framework levers, provide an actionable roadmap to addressing the behavioral health workforce crisis.
Figure 1

Recommendations for Using the Levers of Change
The recommendations focus on the intersection of the levers of change and how they affect the behavioral health workforce crisis:
- Workforce expansion is the key lever to building behavioral health resources that are more representative of communities and creating systems that are grounded in equity.
- Payment is a primary lever for addressing gaps in equity of behavioral health worker salaries, building pipelines for the future workforce and creating reimbursement policies that support an expanded workforce. Payment recommendations often are interconnected with policy and regulatory levers and may require changes at multiple levels.
- Clinical model changes and innovations in care are central to leveraging the workforce more efficiently and effectively as well as driving workforce satisfaction.
- The behavioral health field will continue to focus on better demonstrating quality and accountability.
- Regulation and policy are foundational levers that federal, state, and local governments use to create the pathways for the workforce changes other sectors will be expected to implement.
- Organizational culture affects the day-to-day experience of the behavioral health workforce.
Connect with Us
The HMA team will continue to partner with the CWS and other stakeholders to address concerns about the current state of the mental health and substance use treatment workforce.
Join the CWS on Tuesday, June 18, at 1:00 pm EDT for the next Workforce Solutions Jam, a monthly webinar series to build national momentum and encourage collaboration through the CWS. June’s theme is State Leadership for Workforce Innovation and Development. Register now: https://bit.ly/3yKF2iJ
For more information about the report and the recommendations described, contact our expert team members and authors of the report: Courtney Thompson, Paul Fleissner, Gina Lasky, PhD, MAPL, and Gina Eckart, MS LMHC.

HMA Roundup
Alaska
Alaska Faces Class Action Lawsuit Over Extended Wait Times for Medicaid Applications. Alaska Public Media reported on June 7, 2024, that a class action lawsuit has been filed in Alaska over the state’s failure to process Medicaid applications in a timely manner. The lawsuit requests that the state act on an application within 30 days or 90 days for people who require a disability determination. The state completed about 40 percent of new and renewing Medicaid applications on time during state fiscal year 2023. Read More
Arkansas
Arkansas Names Jennifer Daniel Brezée as DDS Director. The Arkansas Department of Human Services (DHS) announced on June 10, 2024, that it has named Jennifer Daniel Brezée as the new director of the Division of Developmental Disabilities Services (DDS). Brezée most recently served as the Senior Director of Operations at CareSource PASSE. Read More
California
California Medicaid Doctors Introduce Ballot Measure for Higher Pay. The Associated Press reported on June 11, 2024, that California doctors serving the Medicaid population introduced a ballot measure that would increase their rates. Doctors were promised higher pay starting in January 2025, but state officials have since pulled back on the proposal due to the increasing budget deficit. The measure will appear on the November ballot. Read More
Idaho
Idaho to Release Dual Eligible, LTSS Managed Care Procurement in June 2024. The Idaho Department of Health and Welfare, Division of Medicaid will release a procurement for the Medicare Medicaid Coordinated Plan (MMCP) and Idaho Medicaid Plus (IMPlus) programs in June 2024. The MMCP is a fully-integrated special needs plan (FIDE SNP) and IMPlus is a long term services and supports (LTSS) wrap around managed care program. Previously, these programs have not been procured through a competitive bid. Plans who are awarded must offer both MMCP and IMPlus, which collectively serve 26,000 individuals. Implementation is scheduled for January 2026. Incumbents are Blue Cross Blue Shield of Idaho and Molina. Read More
Illinois
Illinois Governor Signs Medicaid Omnibus Bill. Health News Illinois reported on June 10, 2024, that Illinois Governor JB Pritzker signed the Medicaid omnibus bill that will enhance rates for a several types of healthcare providers, establish payment rates for specialized mental health rehabilitation facilities, and exempt highly rated hospitals or physicians from prior authorization for at least one year. The bill also sets new reporting requirements for pharmacy benefit managers in the Medicaid program. Read More
Illinois Governor Signs Fiscal 2025 Budget. Health News Florida reported on June 6, 2024, that Illinois Governor JB Pritzker signed the $53.1 billion state budget plan for fiscal 2025, which includes $155 million to support safety-net hospitals serving low-income communities. The budget includes a $1 per hour wage increase for direct service professionals caring for individuals with intellectual and developmental disabilities and $290.3 million for the Department of Human Services to support homelessness services. It also includes $440 million for two programs that provide Medicaid-like coverage for some undocumented adults. Read More
Michigan
Michigan Releases HIDE SNP RFP to Transition MI Health Link Dual Demo. The Michigan Department of Health and Human Services released on June 6, 2024, the Highly Integrated Dual Eligible Special Needs Plan (HIDE SNP) request for proposals (RFP). This marks a significant step in the transition of the current MI Health Link financial alignment initiative dual demonstration program to meet new federal D-SNP requirements. The HIDE-SNP will integrate long-term service and supports (LTSS) and contracted managed care plans will provide all Medicare and most Medicaid covered benefits for their dual-eligible enrollees through capitated, D-SNP only contracts. Specialty Medicaid behavioral health services will remain carved out and will continue to be provided by Regional Pre-Paid Inpatient Health Plans (PIHPs). Proposals are due August 1. The implementation phase is slated to begin in January 2026, initially covering limited regions of the state before expanding statewide by January 2027. Incumbents CVS/Aetna, AmeriHealth Caritas, HAP/CareSource, Centene/Meridian Health Plan, Molina, and Upper Peninsula Health Plan currently serve 35,000 dual eligibles. Plans will be awarded by region, ranging from two to eight plans for each region. Read More
Missouri
Missouri Faces Federal Funding Cuts Over Medicaid Application Delays. Modern Healthcare reported on June 11, 2024, that the Centers for Medicare & Medicaid Services (CMS) may withhold federal Medicaid funding for Missouri and Texas due to the extent of the states’ delays in processing Medicaid applications. Approximately 40 percent of Medicaid applications in Texas, Missouri, and four other states took longer than the 45 days federal law allows. Read More
New Hampshire
New Hampshire Releases Medicaid Enterprise Systems (MES) Systems Integration RFP. The New Hampshire Department of Health and Human Services released on June 7, 2024, a request for proposals (RFP) for a Systems Integrator (SI) vendor to support a multi-year initiative to implement a Medicaid Enterprise System (MES). As part of the MES implementation, the state will replace its current Medicaid Management Information System (MMIS) and integrate the MMIS modules, including electronic visit verification system, claims processing, data warehouse, provider management, and the pharmacy benefits management system. Proposals are due July 16. The contract term will run for five years, with up to five one-year renewals. Read More
New Hampshire Stakeholders Fail to Reach Deal on Hospital Provider Tax Payments. The Concord Monitor reported on June 7, 2024, that New Hampshire’s hospitals may lose millions of dollars after lawmakers, hospitals, and Governor Chris Sununu were unable to reach a compromise on state payments for uncompensated care. Hospitals currently pay the state nearly $320 million in Medicaid Enhancement Taxes (METs) annually, which is eligible for a federal match that results in hospitals receiving 91 percent of that total to cover uncompensated care costs. Hospitals rejected the governor’s proposal to distribute the 91 percent MET match differently, which would have given some of the funds to non-hospital Medicaid providers who do not pay METs, including community mental health centers and substance use disorder clinics. The current arrangement expires at the end of June. Governor Sununu directed DHHS Commissioner Lori Weaver in a letter to tell the Centers for Medicare & Medicaid Services that the state would be returning only 80 percent of the MET revenue to hospitals. Read More
New Mexico
New Mexico Medicaid to Reimburse Tribal Community Health Workers. KRQE reported on June 6, 2024, that the New Mexico Medicaid program will begin reimbursing community health workers as part of an effort to address health disparities. The workers, known as “Tribal health representatives,” help ensure access to care in rural communities. Read More
Oregon
Oregon Receives Federal Approval to Establish Basic Health Program. The Centers for Medicare & Medicaid Services announced on June 7, 2024, that it has approved Oregon’s blueprint to establish a basic health program (BHP). Enrollees will receive comprehensive benefits and will not be charged premiums or be required to participate in other cost sharing. Oregon will transition individuals with incomes of 138-200 percent of the federal poverty level from the Oregon Health Plan Section 1115 waiver demonstration to the BHP, beginning July 1, 2024. Read More
Rhode Island
Rhode Island Submits Addendum Request to Section 1115 Comprehensive Demonstration for HRSN Services. The Center for Medicare & Medicaid Services (CMS) announced on June 7, 2024, that Rhode Island submitted an addendum to its extension request for its section 1115 Rhode Island Comprehensive Demonstration. The addendum aims to provide health-related social needs (HRSN) services, contingency management (CM) services, and 90 days of pre-release coverage for incarcerated individuals. The federal comment period is open through July 7. Read More
Texas
Texas HHSC Rejects Protests Over Medicaid, CHIP Awards. The Texas Tribune reported on June 6, 2024, that the Texas Health and Human Services Commission (HHSC) rejected protests against the Medicaid STAR and CHIP procurement awards, which reduced the number of plans serving the programs, including eliminating three major health plans run by the state’s nonprofit children’s hospitals, and reduced the number of regions in which each plan can participate in. Plan are expected to appeal. HHSC Executive Commissioner Cecile E. Young is responsible for issuing the final decision. Read More
Texas Medicaid Application Delays May Cost State Millions in Federal Funding. KXAN reported on June 10, 2024, that the Centers for Medicare & Medicaid Services (CMS) may withhold federal Medicaid funding for Texas due to the extent of the state’s delays in processing Medicaid applications. Approximately 40 percent of Medicaid applications in the state took longer than the 45 days federal law allows, according to a letter CMS sent to the Texas Health and Human Services Commission (HHSC). CMS is requiring that HHSC share data on applications and staffing so they can review the agency’s efficacy in running the Medicaid program. HHSC provided a corrective action proposal on May 29, 2024, and estimates it can come into compliance by September 1, 2025. Read More
Vermont
Vermont Governor Signs Legislation to Review Doula Regulation Practices. WCAX3 reported on June 11, 2024, that Vermont Governor Phil Scott signed legislation to conduct a statewide review into best practices for doula regulations, considering registration, certification, or licensure. The review will inform whether the state will provide Medicaid coverage for doula services. Read More
Wisconsin
Wisconsin Disenrolls 30,000 Medicaid Beneficiaries During April Redeterminations. The Wisconsin Department of Health Services announced that it has disenrolled 29,905 Medicaid beneficiaries during April eligibility redeterminations. Of those disenrolled, 10,598 lost coverage due to ineligibility and 19,307 lost coverage for procedural reasons. Read More
National
CMS Releases National Health Expenditure Projections For 2023 Through 2032. The Centers for Medicare & Medicaid Services’ (CMS) Office of the Actuary released on June 12, 2024, its projections of National Health Expenditures (NHE) and health insurance enrollment for the years 2023-2032. It is projected that the average rate of growth for Medicaid spending will be 5.2 percent and 7.4 percent for Medicare. The average annual growth in NHE is projected to be 5.6 percent. Read More
MACPAC Releases June 2024 Report to Congress. The Medicaid and CHIP Payment and Access Commission (MACPAC) released its June 2024 Report to Congress on Medicaid and CHIP. The report focused on three issues of interest to Congress: demographic data in Medicaid; improving the transparency of financing the non-federal share of Medicaid and CHIP; recommendations for how states can optimize and oversee state Medicaid agency contracts with Medicare Advantage dual eligible special needs plans; and enrollment trends in Medicare Savings Programs. Read More
Insurers Estimate $1.1 Billion in MLR Rebates Across Commercial Markets in 2024. KFF reported on June 5, 2024, that insurers estimate they will issue $1.1 billion in medical loss ratio (MLR) rebates under the Affordable Care Act across all commercial markets in 2024 based on preliminary self-reported data. Approximately one-third of this amount will come from the individual market. Individual and small group markets, including the Marketplace, require an 80 percent MLR, whereas large group markets require an 85 percent MLR. Since 2012, insurers have paid out $11.8 billion in rebates. Read More
CMS Releases Guidance on Medicaid Managed Care Monitoring, Oversight. The Centers for Medicare & Medicaid Services (CMS) released on June 12, 2024, guidance to provide tools for improving the monitoring and oversight of managed care in Medicaid and the Children’s Health Insurance Program (CHIP). The guidance also reinforces state compliance in separate CHIP mental health and substance use disorder parity requirements. Read More
Attorneys General Requests Supreme Court to Uphold States’ Authority to Regulate PBMs. Modern Healthcare reported on June 11, 2024, that a bipartisan coalition of 32 attorneys general filed an amicus brief urging the U.S. Supreme Court to reconsider an August 2023 ruling which held that federal laws supersede state laws when regulating Pharmacy Benefit Managers (PBMs). The coalition is specifically requesting that the court review a decision from the U.S. Court of Appeals for the Tenth Circuit, which invalidated Oklahoma’s Patient’s Right to Pharmacy Choice Act. The act sought to regulate PBM pharmacy networks and ban discounts for individuals shopping at preferred pharmacies, among other controls. Read More
Supreme Court to Hear Case on DSH Payments. Reuters reported on June 10, 2024, that the U.S. Supreme Court will hear a lawsuit alleging that Medicare underpays hospitals that serve low-income populations by an estimated $1.5 billion per year. The 200 hospitals across 32 states are requesting the court to overturn a U.S. Court of Appeals decision that upheld how the U.S. Department of Health and Human Services (HHS) calculates the Medicare disproportionate share hospital (DSH) funding. Hospitals argue that HHS only uses the number of Medicare patients who actually receive supplemental security income in their calculations, and does not include those who are eligible but do not receive the benefit, when determining DSH funding. Read More
White House Partners with Google, Microsoft to Strengthen Rural Hospital Cyber Security. Modern Healthcare reported on June 10, 2024, that the White House is partnering with Microsoft and Google to strengthen rural hospitals cybersecurity. The partnership will provide reduced-cost or free services to at least 1,800 rural hospitals. Microsoft is making free training and support available. Google will launch a pilot program with four or five rural hospitals to develop personalized security packages. Read More
HHS Must Pay Native American Tribes Overhead Costs for Administering Healthcare Programs, Court Rules. Reuters reported on June 6, 2024, that the U.S. Supreme Court ruled that the Department of Health and Human Services (HHS) must pay Native American Tribes for overhead costs when they administer their own healthcare programs, including Medicare and Medicaid. The ruling confirms that HHS has been underfunding Tribes and affirms decisions by the 9th and 10th U.S. Circuit Courts of Appeals. Funding for HHS’s Indian Health Service division could be between $800 million and $2 billion annually. The San Carlos Apache Tribe in Arizona and the Northern Arapaho Tribe in Wyoming were the plaintiffs in the case. Read More
Industry News
Addus HomeCare Signs Agreement to Acquire Gentiva Personal Care. Hospice care provider Addus HomeCare Corporation announced on June 10, 2024, a definitive agreement to acquire the personal care operations of Georgia-based Gentiva for approximately $350 million. Gentiva’s personal care company operates in seven states including Arizona, Arkansas, California, Missouri, North Carolina, Tennessee, and Texas. Read More
Elevance Wins Medicare Advantage Star Rating Lawsuit. Modern Healthcare reported on June 10, 2024, that Elevance Health won a federal lawsuit alleging the Centers for Medicare & Medicaid Services (CMS) did not follow proper procedures when calculating the Medicare Advantage Star rating for one of the plan’s subsidiaries, Anthem Blue Cross and Blue Shield (BCBS) of Georgia, causing the plan to lose $500 million in quality bonus payments. CMS modified its rating procedures in 2020 when the agency announced its plan to implement the Tukey Outer Fence Outlier Deletion Method. However, CMS omitted the policy in a proposed rule and then reintroduced it in the preamble of a subsequent rule. CMS will recalculate Anthem BCBS’s Star rating. SCAN Health Plan recently won a similar lawsuit over Star ratings. Read More
Judge Blocks DOJ from Dismissing Humana Medicare Advantage Lawsuit. Modern Healthcare reported on June 7, 2024, that a federal judge denied the U.S. Department of Justice’s (DOJ) attempt to dismiss Humana’s legal challenge against the U.S. Department of Health and Human Services over Medicare Advantage (MA) auditing standards. Humana’s September 2023 lawsuit alleges that the Centers for Medicare & Medicaid Services (CMS) updated auditing standards, which would allow the agency to claw back overpayments to MA plans, violated the Administrative Procedure Act. Humana claims CMS did not properly explain the reason behind the update or have authority to retroactively apply the standards to audits beginning in 2018. The DOJ attempted to dismiss the case since CMS had not yet begun auditing Medicare Advantage insurers’ 2018 data and Humana had not been harmed. Read More
Change Healthcare Data Breach Lawsuits Centralized in Minnesota. Reuters reported on June 7, 2024, that the federal Judicial Panel on Multidistrict Litigation centralized 49 lawsuits against UnitedHealth Group’s Change Healthcare in Minnesota, where United is headquartered. The lawsuits, stemming from consumers and providers, allege that Change’s payment processing system failed to protect personal information during the February cyber attack. Those involved in the lawsuits are seeking damages for providers’ loss of wages and consumers’ cost of credit monitoring or identity theft. Read More
Judge Denies FTC Injunction to Block Novant Health’s Acquisition of North Carolina Hospitals. Modern Healthcare reported on June 5, 2024, that a federal judge ruled against the Federal Trade Commission (FTC) injunction to block Novant Health’s $320 million acquisition of two hospitals in North Carolina from Community Health Systems. The injunction was issued earlier this year after the FTC deemed the deal would harm competition in the market. Novant can move forward with its plan to purchase the hospitals. Read More
RFP Calendar
HMA News & Events
HMA Webinars:
Medicare Physician Fee Schedule Reform – Structural Topics and Recommendations. Thursday, June 13, 2024, 12 PM ET. HMA recently released a report on the Medicare Physician Fee Schedule (PFS) with background on the structure of the program, and recommendations for reforms that could be considered. We’d like to invite you to a webinar that will provide background and context about the PFS for interested parties who may be less familiar with the payment system and why the stakeholder community got to the point of needing to “fix” the fee schedule. We will discuss pressing policy and payment concerns, provide an overview of key structural issues within the PFS that should be considered and balanced when making policy changes to the payment system, highlight different stakeholder perspectives, and offer recommendations within CMS authority. Register Here
Workforce Solutions Jam | Aligning Across Levers of Change. Addressing the workforce crisis requires a comprehensive approach that aligns and “pulls” multiple levers of change in concert and over time to create meaningful impact. A combination of infrastructure development and the implementation of workforce strategies has shown promising results in one State via a collaborative and intentional approach to advancing workforce solutions. Register Here
D-SNP Growth and Integration: Key Implications of the 2025 CMS Final Rule. Thursday, June 20, 2024, 11 AM ET. Join us for an informative webinar where HMA experts will review the upcoming changes from the 2025 Final Rule that will impact Dual Special Needs Plans (D-SNPs) in 2025 and beyond. The session will feature an analysis of the new regulations and a discussion of the critical strategic and product impacts on Medicare organizations offering D-SNPs or considering offering D-SNPs. Attendees will also have the opportunity to engage with the panelists during a Q&A session. Don’t miss this chance to stay informed and ahead of the curve with expert guidance from HMA. Register Here
Supporting Family Caregivers: The Changing Policy and Practice Landscape. Thursday, June 27, 2024, 12 PM ET. Over the past decade, the U.S. has seen significant federal and state policy initiatives to improve and expand assistance for the millions of family members who help care for older adults, and those who support people with intellectual and developmental disabilities (I/DD) across the lifespan. The pandemic, combined with workforce shortages, accelerated these efforts. In this webinar with national family caregiving experts, we’ll discuss policy and practice advances, and their potential impact on enabling more Americans to live at home and in the community. Register Here
Wakely, an HMA Company, White Papers:
Is PC Flex Right for Your ACO? The Primary Care Flex (PC Flex) model is a new Center for Medicare and Medicaid Innovation (CMMI) model developed to further test how alternative payments for primary care services (PCS) can empower Accountable Care Organizations (ACOs) to use more innovative, team-based, person-centered, and proactive approaches to care that positively impact health care outcomes, quality, and costs of care. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
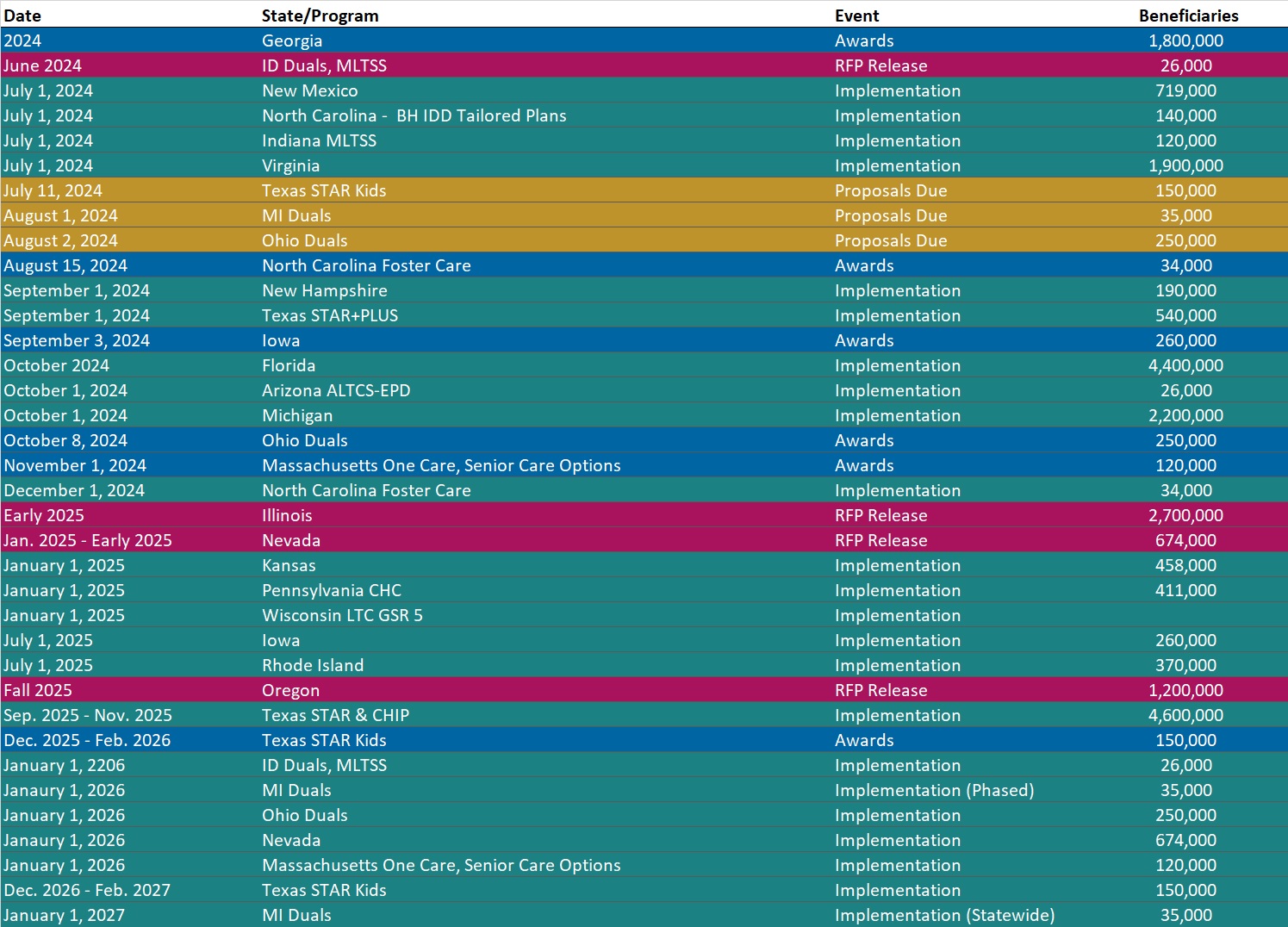
- Updated Medicaid Managed Care RFP Calendar: 50 States and DC
- Updated National Medicaid Dental Benefits Management RFP Calendar
- Updated Virginia State Overview
Medicaid Data
Medicaid Enrollment:
- Arizona SNP Membership at 147,042, Mar-24 Data
- Arkansas SNP Membership at 105,843, Mar-24 Data
- Connecticut SNP Membership at 108,881, Mar-24 Data
- District of Columbia Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Georgia Medicaid Managed Care Enrollment is Down 6.9%, Jun-24 Data
- Hawaii Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Illinois SNP Membership at 39,911, Mar-24 Data
- Massachusetts Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Minnesota SNP Membership at 59,484, Mar-24 Data
- North Dakota Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Virginia SNP Membership at 116,418, Mar-24 Data
- Virginia Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Michigan HIDE SNP RFP, Jun-24
- New Hampshire Medicaid Enterprise Systems (MES) Systems Integration RFP, Jun-24
Medicaid Program Reports, Data, and Updates:
- Oregon Basic Health Program Blueprint Approval, Jun-24
- Pennsylvania MLTSS Subcommittee Meeting Materials, 2021-24
- Rhode Island Comprehensive Demonstration Section 1115 Waiver Documents, 2013-24
- Texas Medicaid Managed Care Oversight and Quality Presentation, Jun-24
- Texas Medicaid Managed Care Procurement Process Presentation, Jun-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
