HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Releases Report on Nonemergency Medical Transportation in Medicaid

- Medicaid Eligibility Redeterminations News: Arizona, District of Columbia, Florida, Idaho, Maryland, Michigan, Mississippi, New Jersey, Tennessee, Wyoming

- Florida Extends Deadline for Medicaid Managed Care ITN Responses

- Georgia Launches Partial Medicaid Expansion Program With Work Requirements

- Idaho Medicaid Managed Care Task Force Holds Hearing on Structure of Program Funding

- New Jersey Will Allocate $5 Million to Improve Housing for Individuals with Disabilities, Acute Medical Needs

- New York Releases Third-Party Liability Match, Recovery Services RFP

- North Carolina Further Delays Implementation of Behavioral Health IDD Tailored Plans

- Ohio Releases RFP for Medicaid Enterprise System Alternate Payment Model Logic, Reporting Tool

- Pennsylvania Medicaid to Cover Care Delivered on Streets to Homeless

- ACA Risk Adjustment Pool to Redistribute $15.2 Billion to Individual Plans

- AmeriHealth Caritas CEO Paul Tufano to Step Down

In Focus
CMS Releases Report on Nonemergency Medical Transportation in Medicaid
This week, our In Focus section reviews the Centers for Medicare & Medicaid Services (CMS) report to Congress on Non-emergency Medical Transportation (NEMT) in Medicaid, released June 20, 2023. CMS found that approximately 3 million to 4 million Medicaid beneficiaries used NEMT services annually between 2018 and 2021 and made recommendations related to Medicaid coverage of NEMT for medically necessary services.
Background
NEMT includes transportation services not limited to public transport, taxis, personal vehicle transport, non-emergency ambulances, air transport, and transportation network companies. Medicaid, unlike private insurers and Medicare, covers NEMT for any covered medical service for beneficiaries with an unmet transportation need. NEMT program administration varies from state to state and can be on a fee-for-service basis, carved out with third-party transportation brokers, or carved into the Medicaid risk-based managed care contracts. Under the Consolidated Appropriations Act, 2021, which made NEMT a statutory requirement, HHS must conduct and submit an analysis of nationwide Medicaid NEMT services to Congress. An initial report was submitted in June 2022.
Table 1. NEMT Service Delivery Models by State, 2018−2021
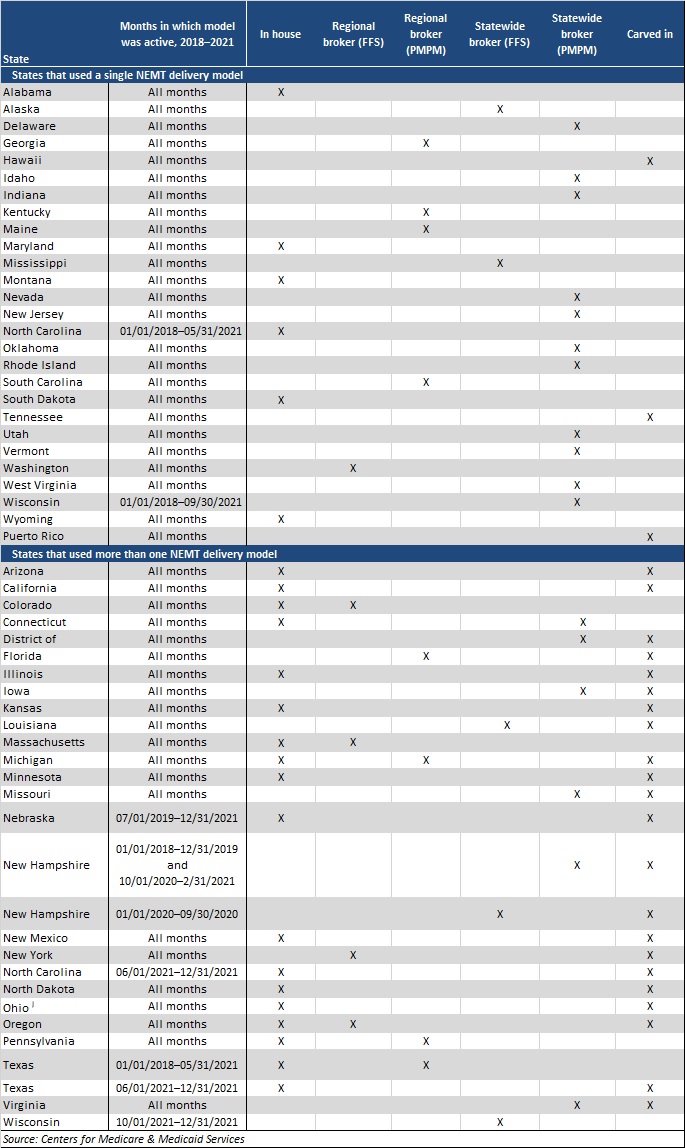
CMS conducted the analysis using Transformed Medicaid Statistical Information System (T-MSIS) data for calendar years 2018−2021. The analysis covered the number and percentage of Medicaid beneficiaries using NEMT, the average number of NEMT ride days, the types of medical services beneficiaries accessed when using NEMT, monthly trends in use of NEMT versus telehealth services before and during the COVID-19 public health emergency (PHE), and a comparison of the volume of NEMT services used by delivery model and state.
The T-MSIS data has some limitations and may not capture all Medicaid NEMT provided to beneficiaries due to differences in billing practices across states and providers. For example, if states claim certain medical service expenditures as administrative expenditures, T-MSIS will not capture it. Further, the number of ride days undercounts the total number of NEMT rides, as beneficiaries may receive multiple NEMT rides in a day. Because of these and other limitations, the data represents a subset of the NEMT that the Medicaid program covers.
Findings
Approximately 3−4 million Medicaid beneficiaries used NEMT annually in 2018−2021, representing 4−5 percent of Medicaid beneficiaries. Alaska, Minnesota, Arizona, Maine, and Wisconsin had the highest percentage of Medicaid beneficiaries who used NEMT, with up to nearly 11 percent in Alaska in 2021.
States that used a capitated broker model to deliver NEMT saw the highest use of these services. However, on average, states that used in-house NEMT delivery model claimed a relatively high percentage of NEMT expenditures as administrative expenditures, and NEMT administrative expenditures generally are not captured in the T-MSIS data.
Figure 1. Number of NEMT Ride Days per 10,000 Beneficiaries, by Delivery Model and Beneficiary Subgroup, 2021
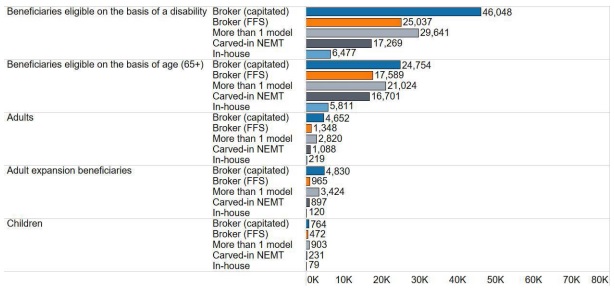
Medicaid enrollees with the highest NEMT usage rates included individuals in Money Follows the Person, receiving Section 1915c home- and community-based services, dually eligible for Medicare and Medicaid, and aging adults and people with disabilities. In addition, Medicaid members with certain physical and mental health conditions and those with a substance use disorder had higher rates of usage compared with the average Medicaid members. Medicaid enrollees in remote areas also used NEMT at the highest rates.
During the COVID-19 PHE, rates of NEMT dropped from 3.9 million beneficiaries, or 5 percent of all Medicaid members in 2019, to 3.5 million (4 percent) in 2020 and 3.3 million (4 percent) in 2021. In 2019−2020, the total number of annual NEMT ride days dropped by 37 percent, from 81.3 million to 53.1 million, but increased by more than 4 percent (to 55.5 million) in 2021. On average, the monthly number of NEMT ride days in 2021 remained about 30 percent below pre-PHE levels, and the number of beneficiaries using NEMT remained 23 percent below pre-PHE levels. The COVID-19 PHE caused telehealth to sharply increase. Throughout the PHE, telehealth was used more frequently than NEMT to access certain services.
Recommendations
CMS found that public transit was rarely used for NEMT, even though more than one-third of beneficiaries live in large, urban areas. In the report, CMS recommends that states should find opportunities to improve operations between NEMT and public transit networks to better coordinate services for beneficiaries.
CMS also recommends that states further examine the role of NEMT in improving the use of timely preventive care. Beneficiaries used NEMT to access preventive services at the highest rate of all service types examined. The analysis found some evidence that use of NEMT increases access to preventive services and is cost-effective, implying that increasing the uptake of NEMT may confer cost savings to states and the federal government.
Finally, CMS recommends that states increase awareness of the NEMT benefit. Medicaid beneficiaries’ knowledge of the benefit is low. CMS urges states to work with health plans and providers to share information with beneficiaries about the availability of NEMT.
HMA Roundup
Arizona
Arizona Disenrolls Nearly 200,000 Medicaid Beneficiaries Following Redeterminations. AHCCCS News reported on July 10, 2023, that the Arizona Health Care Cost Containment System (AHCCCS) has disenrolled nearly 200,000 Medicaid beneficiaries since redeterminations began in April. Of the 1.1 million renewals initiated, 41 percent have maintained coverage, 18 percent have been discontinued, and 41 percent are currently under review. About 25 percent of disenrolled individuals are utilizing the 90-day grace period to complete their renewal. Read More
District of Columbia
District of Columbia Disenrolls 3,000 Medicaid Beneficiaries Following May Redeterminations. The Washington City Paper reported on July 6, 2023, that the District of Columbia has disenrolled about 3,000 Medicaid beneficiaries following May redeterminations. Read More
Florida
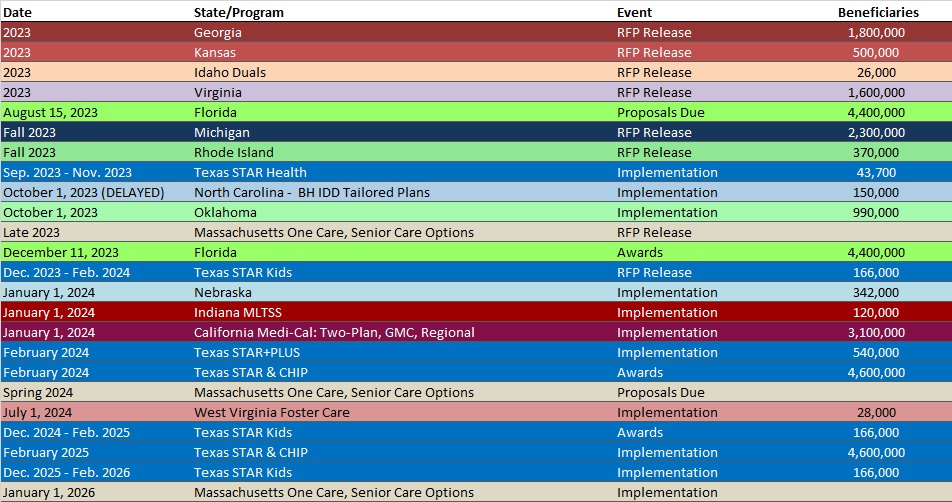
Florida Extends Deadline for Medicaid Managed Care ITN Responses. Florida Politics reported on July 7, 2023, that Florida’s Agency for Health Care Administration has released an addendum to its Statewide Medicaid Managed Care Invitation to Negotiate (ITN), extending the deadline for replies from August 15 to August 22. The addendum also answers previously submitted questions, adds accountable care organizations to the list of potential partners, and prohibits the use of flat-rate payment arrangements between managed care plans and providers. Contracts are expected to be worth between $120 billion and $150 billion over six years, and awards will be announced December 11. Read More
Florida Declines Federal Waivers Aimed at Mitigating Medicaid Coverage Losses During Redeterminations. WUSF reported on July 7, 2023, that Florida is one of two states that has not pursued federal waivers aimed at mitigating Medicaid coverage losses from procedural errors during the redeterminations process. The other is Montana. The waivers allow states to immediately renew coverage for people with little or no income, provide aid to those completing renewal forms, and delay administrative terminations for a month. Read More
Georgia
Georgia Launches Partial Medicaid Expansion Program With Work Requirements. The Georgia Department of Community Health announced on July 5, 2023, the launch of the state’s Pathways to Coverage Medicaid expansion program, which requires 80 hours of work or volunteering per month in order to qualify for coverage. The program covers individuals ages 19 to 64 with household incomes of up to 100 percent of the Federal Poverty Level. Read More
Idaho
Idaho Medicaid Managed Care Task Force Holds Hearing on Structure of Program Funding. The Idaho Capital Sun reported on July 10, 2023, that Idaho legislators on the Medicaid Managed Care Task Force held its first hearing on the potential restructuring of how Medicaid is funded, including a look at whether managed care drives cost savings and improves quality. The next hearing is July 25. Read More
Idaho Disenrolls 87,000 Following Medicaid Redeterminations. The Idaho Capital Sun reported on July 10, 2023, that Idaho has disenrolled more than 87,000 Medicaid beneficiaries since redeterminations began in April. More than half lost coverage for procedural reasons. Read More
Maryland
Maryland Disenrolls 28,694 Medicaid Beneficiaries Following June Redeterminations. The Maryland Department of Health announced on July 11, 2023, the disenrollment of 28,694 Medicaid beneficiaries following June redeterminations. Approximately 17,000 lost coverage due to procedural reasons, 98,630 were renewed, and another 11,894 are pending review. Read More
Michigan
Michigan Disenrolls 12,000 Medicaid Beneficiaries During June Redeterminations. The Michigan Department of Health and Human Services announced on July 6, 2023, the disenrollment of approximately 12,000 Medicaid beneficiaries during June redeterminations, which is the first month the state has disenrolled anyone. The state renewed coverage for more than 103,500.
Mississippi
Mississippi Disenrolls Nearly 29,500 Medicaid Beneficiaries During June Redeterminations. The Associated Press reported on July 11, 2023, that Mississippi disenrolled nearly 29,500 Medicaid beneficiaries during June redeterminations. The state renewed coverage for almost 33,000 beneficiaries. Read More
Missouri
Missouri Extends Postpartum Medicaid Coverage. The Missouri Independent reported on July 7, 2023, that Missouri Governor Mike Parson signed legislation to extend postpartum Medicaid coverage from 60 days to 12 months. The extension will cover an estimated 4,000 individuals. Read More
Nevada
Nevada to Receive $285 Million in Opioid Settlement. The Associated Press reported on July 5, 2023, that Nevada reached a $285 million settlement with Walgreens for its role in the opioid epidemic. Walgreens, which will pay the money over 15 years, is the final defendant named in a lawsuit filed by the state in 2019. About $98.1 million will go to funding opioid recovery programs through the state Department of Health and Human Services. Read More
New Jersey
New Jersey Will Allocate $5 Million to Improve Housing for Individuals with Disabilities, Acute Medical Needs. Al Dia News reported on July 10, 2023, that the New Jersey Department of Health will allocate $5 million to purchase, develop, and renovate group homes for individuals with intellectual and developmental disabilities and acute behavioral and medical needs. The funding is available through the Money Follows the Person program. Group homes meeting specific criteria will each receive $90,000. Read More
New Jersey Initiates Medicaid Eligibility Redeterminations for 333,000 Beneficiaries in May. New Jersey Spotlight News reported on July 5, 2023, that New Jersey initiated Medicaid eligibility redeterminations for 333,000 beneficiaries in May. Of these, about 48,000 were renewed, while the rest are pending. The state has previously projected more than 280,000 beneficiaries could be disenrolled as a result of redeterminations. Read More
New York
New York Releases Third-Party Liability Match, Recovery Services RFP. The New York State Office of the Medicaid Inspector General (OMIG) released on July 10, 2023, a request for proposals (RFP) for Medicaid third-party liability match and recovery vendors. Proposals are due August 14. The contract is anticipated to begin in January 2024, and last for three years with two one-year extension options.
North Carolina
North Carolina Further Delays Implementation of Behavioral Health IDD Tailored Plans. The Associated Press reported on July 11, 2023, that the North Carolina Department of Health and Human Services is again delaying implementation of Behavioral Health and Intellectual/Developmental Disabilities (IDD) Tailored Plans. The state did not give a new start date. Implementation was originally scheduled for July 2022, and then delayed three times, most recently to October 2023. The state blamed the delays on network adequacy concerns and technical challenges among regional behavioral health organizations. Read More
Ohio
Ohio Releases RFP for Medicaid Enterprise System Alternate Payment Model Logic, Reporting Tool. The Ohio Department of Medicaid released on June 16, 2023, a request for proposals (RFP) for the state’s Medicaid Enterprise System’s Alternate Payment Model Logic and Reporting Tool. Responses are due July 28. Awards will be announced in September, and the work is scheduled to begin in October. Read More
Ohio to Again Seek Federal Approval to Implement Medicaid Work Requirements in 2025. Cleveland.com reported on July 6, 2023, that Ohio will again seek federal approval to implement Medicaid work requirements in 2025. Under the plan, able-bodied Medicaid enrollees 55 years or younger would have to work or engage in community activities for at least 20 hours per week to access benefits. A prior work requirement was blocked by the Biden Administration in 2021. Read More
Governor Signs State Budget, Vetoes Medicaid Coverage of Doulas. News 5 Cleveland reported on July 5, 2023, that Ohio Governor Mike DeWine vetoed a proposal to use Medicaid funding to cover doulas for pregnant women prior to signing the state’s $191 billion budget. Medicaid currently pays for 51 percent of births in the state. Read More
Oregon
Oregon Implements Full Medicaid Coverage for Eligible Noncitizen Children, Adults. The Oregon Health Authority announced on July 6, 2023, that full Medicaid coverage is available to eligible children and adults regardless of immigration status, effective July 1. Approximately 40,000 individuals ages 26 to 54 who receive coverage of emergency services through the state’s Citizenship Waived Medical program will be enrolled in Medicaid, and all other eligible individuals are able to enroll. Read More
Pennsylvania
Pennsylvania Medicaid to Cover Care Delivered on Streets to Homeless. Pennwatch reported on July 5, 2023, that Pennsylvania will use Medicaid funds to pay for care delivered on the street by certain Medicaid professionals to individuals who are homeless. The practice, known as “street medicine,” will provide services such as primary care, vaccines, wound care, preventive services, counseling, medication for the treatment of opioid use disorder, and diagnostic services. Read More
Tennessee
Tennessee Disenrolls 31,000 Medicaid Beneficiaries Following April Redeterminations. The Chattanooga Times Free Press reported on July 10, 2023, that Tennessee has disenrolled more than 31,000 Medicaid beneficiaries following April redeterminations. More than 23,700 enrollees lost coverage due to procedural reasons. Nearly 43,700 were renewed, and another 5,300 are pending. Read More
Wisconsin
Wisconsin Governor Enacts Budget with $385 Million to Increase Medicaid Reimbursement Rates. Wisconsin Health News reported on July 5, 2023, that Wisconsin Governor Tony Evers signed a fiscal 2025 budget that includes $236 million to increase Medicaid reimbursement rates for hospitals and $149 million to increase rates for primary care, emergency physicians, and chiropractic services. Read More
Wyoming
Wyoming Disenrolls 450 Medicaid, CHIP Enrollees Following Redeterminations. WyoFile reported on July 6, 2023, that Wyoming has disenrolled more than 450 Medicaid or Kid Care CHIP enrollees following April eligibility redeterminations. The state health department has predicted redeterminations will result in coverage losses for between 10,000 and 15,000 beneficiaries over the next nine months. Read More
National
HHS Seeks to Reinstate Obama-era Rule Banning Discrimination Based on Sexual Orientation. Modern Healthcare reported on July 11, 2023, that the Department of Health and Human Services (HHS) has proposed a rule that would define and ban discrimination on the basis of sexual orientation or gender identity in any of its programs, services, or funding opportunities. The rule would reinstate an Obama-era policy that was overturned during the Trump administration. Read More
Buprenorphine Distribution Increases 24 Percent from 2019 to 2022, KFF Finds. Kaiser Family Foundation (KFF) reported on July 11, 2023, that distribution of buprenorphine to treat opioid use disorder grew 24 percent from 2019 to 2022. Growing utilization of telehealth and federal legislation removing barriers to accessing buprenorphine drove the increase. Read More
ACA Risk Adjustment Pool to Redistribute $15.2 Billion to Individual Plans. Health Payer Specialist reported on July 10, 2023, that the federally operated Affordable Care Act risk adjustment program will redistribute $15.17 billion to individual plans in 2022. Another $3.3 billion with be redistributed among small group and other plans. The Centers for Medicare & Medicaid Services reported a slight increase in the number of plans participating. Read More
CMS Proposes $9 Billion Payment for 340B Hospitals to Offset Unlawful Payment Cuts. Fierce Healthcare reported on July 9, 2023, that the Centers for Medicare & Medicaid Services (CMS) is proposing a one-time payment of $9 billion to 340B hospitals to offset unlawful payment cuts in 2022. The U.S. Department of Health and Human Services cut prescription drug payments by nearly 30 percent in 2018, and the Supreme Court ruled the cuts were unlawful in 2022. Read More
Biden Administration Proposes Limiting Short-term Health Plan Durations to 3 Months. CNN reported on July 7, 2023, that the Biden administration has proposed a rule limiting short-term health insurance plans to three months with a one month optional extension, reversing a Trump-era rule allowing short-term plan durations of up to three years including renewals. Plans would also be required to provide a clear explanation of benefits. Read More
Medicare Advantage Quality Bonus Program is Ineffective, Urban Institute Study Finds. Modern Healthcare reported on July 6, 2023, that the Medicare Advantage (MA) quality bonus program is ineffective and often overpays MA plans, according to a study from the Urban Institute. The study found that more than half of MA plans received five percent bonuses for high quality ratings without resulting in better care than traditional Medicare. The study recommends reforms, including targeting outlier performance and providing bonuses to only the best plans. Read More
‘Look Alike’ D-SNP Enrollment Increased by 200,000 from 2013 to 2020, Study Finds. Becker’s Payer Issues reported on July 6, 2023, that enrollment in “look alike” dual-eligible special needs plans (D-SNPs) increased from 20,900 in 2013 to 220,860 in 2020, according to a recent Health Affairs study. The look alike D-SNPs are Medicare Advantage plans marketed towards dual eligibles that are not subject to federal regulations requiring integrated Medicaid services. The study also found look alike plans were more likely to enroll beneficiaries who are older, Hispanic, and from disadvantaged communities compared to regulated plans. Read More
Home Health Association Files Lawsuit Over Medicare Payment Reductions. Modern Healthcare reported on July 6, 2023, that the National Association for Home Care and Hospice filed a lawsuit against the Biden administration over a 3.9 percent reduction in Medicare home health payment rates in 2023 as well as a proposed 5.7 percent cut for 2024. The proposed rates would reduce overall payments to home health providers by $375 million in 2024. Read More
Industry News
AmeriHealth Caritas CEO Paul Tufano to Step Down. AmeriHealth Caritas announced on July 11, 2023, that Paul Tufano, chief executive of the company since 2014, will step down, effective September 1. Thomas Hutton, executive vice president and counsel for AmeriHealth Caritas’s parent company, Independence Health Group, will serve as interim CEO while the company searches for a replacement. Read More
PurposeCare is Acquiring 3 Home-based Care Agencies in Indiana, Ohio. Home Health Care News reported on July 11, 2023, that PurposeCare is acquiring Indiana-based Scott’s Home Healthcare and Attentive Personal Care, as well as Ohio-based Choice Nursing Care & Home Health. All three are home care agencies. PurposeCare serves more than 3,000 mostly dual eligible clients per month. Read More
Baylor Scott & White Health to Acquire Interest in 41 NextCare Urgent Care Centers. Connect CRE reported on July 7, 2023, that Baylor Scott & White Health will acquire a stake in 41 NextCare urgent care clinics throughout Texas. The organizations will integrate systems and branding over the next few months. Baylor Scott & White Health currently owns 51 hospitals in the state. Read More
Dungarvin Acquires 3 IDD Providers in Minnesota, Wisconsin. Behavioral Health Business reported on July 6, 2023, that Dungarvin acquired Bridges MN, Bridges WI, and Rumi, which are all providers of care to individuals with intellectual and developmental disabilities (IDD) at 103 locations in Minnesota and Wisconsin. The transaction is effective September 1. Dungarvin currently operates in 15 states and provides IDD and behavioral health services to 6,000 individuals. Read More
RFP Calendar
HMA News & Events
Upcoming HMA Conference:
HMA Conference to Feature Session on Understanding, Meeting Health-Related Social Needs Requirements. The sixth annual HMA conference in Chicago, October 30-31, will feature a session on understanding and meeting new requirements concerning health-related social needs like housing and food insecurity. Speakers confirmed to date include Richard Ayoub, chief executive, Project Angel Food; Bryan Buckley, director for health equity initiatives, National Committee for Quality Assurance; and Paul Leon, chief executive, National Healthcare & Housing Advisors. To view the entire agenda and to register, visit here.
Upcoming HMA Webinar:
Medicaid 1115 Justice Waiver Opportunities: Medication Assisted Treatment for Substance Use Disorder in Carceral Settings. Part 4 of HMA’s webinar series, 1115 Medicaid Justice Demonstration Waivers: Bridging Healthcare, will focus on access to medication assisted treatment (MAT) for opioid use disorder during and after transition from a carceral setting into the community, to ensure continuity of care for those leaving incarceration to reduce overdose and recidivism. Thursday, July 13, 2 pm ET. Register Here
Wakely, an HMA Company, White Paper:
Implications of the 2023 CAA on Medicare Physician Fee Schedule. The Consolidated Appropriations Act, 2023 (the 2023 CAA) was passed and signed into law December 29, 2022. This paper includes a summary of important provisions that impact physicians in 2023 and beyond, together with Wakely’s analysis of the CY 2023 rate changes using national Medicare Fee-for-Service (FFS) data and the Wakely Medicare Repricing Analysis Tool (WMRAT). Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Colorado RAE Enrollment is Up 0.7%, Jan-23 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 1%, Mar-23 Data
- Illinois Medicaid Managed Care Enrollment is Up 1.8%, May-23 Data
- Illinois Dual Demo Enrollment is Down 3.3%, May-23 Data
- Iowa Medicaid Managed Care Enrollment is Up 2.1%, May-23 Data
- Massachusetts Medicaid Managed Care Enrollment is Up 6.7%, 2021 Data
- New Hampshire Medicaid Managed Care Enrollment is Up 5.3%, 2022 Data
- North Dakota Medicaid Expansion Enrollment is Up 6.2%, May-23 Data
- Ohio Medicaid Managed Care Enrollment is Up 7%, Mar-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 0.8%, May-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Florida Statewide Medicaid Managed Care (SMMC) Program ITN and Q&A, 2023
- New York Medicaid Third-Party Liability Match and Recovery Services RFP, Jul-23
- North Carolina Comprehensive Independent Assessment Entity Services RFP, Responses, and Evaluation, 2022
Medicaid Program Reports, Data, and Updates:
- Arizona Medicaid Eligibility Renewals Dashboard, Jul-23
- Arkansas PHE Medicaid Redeterminations Monthly Reports to CMS, Jun-23
- District of Columbia Medicaid Renewal Community Meeting Presentations, Jun-23
- Michigan PHE Medicaid Redeterminations Monthly Reports to CMS, Jun-23
- Mississippi PHE Medicaid Redeterminations Monthly Reports to CMS, Jun-23
- Nevada PHE Medicaid Redeterminations Monthly Reports to CMS, May-23
- New Jersey Medicaid, MLTSS Quality Technical Reports, CY 2020-22
- New Jersey PHE Medicaid Redeterminations Monthly Report, May-23
- North Carolina Medicaid Annual Reports, SFY 2015-22
- Pennsylvania PHE Medicaid Redeterminations Monthly Reports to CMS, May-23
- Tennessee Medicaid Redeterminations Renewals Report, Apr-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
