UnitedHealth Group Completes Acquisition of LHC Group. Modern Healthcare reported on February 22, 2023, that UnitedHealth Group completed its $5.4 billion acquisition of LHC Group, a home health and hospice provider. The deal was originally announced in March 2022. Read More
HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Announces Plans to Pursue New Medicare and Medicaid Drug Payment Models

- Arizona to Terminate Nearly 5,300 Medicaid Providers for Non-compliance

- Medicaid Expansion News: Arkansas, Mississippi, New Mexico, North Carolina

- Florida Representative Proposes Medicaid Managed Care Pilot Program for Individuals with Developmental Disabilities

- Medicaid Dental News: Florida, Iowa, Michigan, Nebraska, Virginia,

- Iowa Recommends Maximizing Access to HCBS for Individuals with LTSS Needs

- Massachusetts to Release One Care, Senior Care Options RFR in Late 2023

- Oklahoma to Phase In Medicaid Eligibility Redeterminations by Population

- West Virginia House Committee Recommends Bill to Create Medicaid Buy-in Program

- CMS Seeks Corrective Action Plans from Hospitals Falling Short on Price Transparency Requirements

- Amazon Completes Acquisition of One Medical

In Focus
CMS Announces Plans to Pursue New Medicare and Medicaid Drug Payment Models
This week our In Focus section reviews the Centers for Medicare and Medicaid Services’ (CMS) announcement that the agency will explore three new prescription drug payment models in the Medicare and Medicaid programs:
- Medicare High-Value Drug List Model
- Cell and Gene Therapy (CGT) Access Model
- Accelerating Clinical Evidence Model
The announcement – and accompanying report – responds to President Biden’s October 2022 Executive Order directing CMS’ Center for Medicare and Medicaid Innovation (the Innovation Center) to identify models that could lower cost sharing for commonly used drugs and include value-based payment for drugs.
Notably, the Innovation Center offered varying levels of specificity about the models, leaving unanswered many questions about the structures and timelines for the potential models. The Innovation Center will need to conduct more robust analysis to determine the design specifications for each model, stakeholder interest, and practical and political feasibility for each. In addition, each model will need to have its own application or rulemaking process to identify participants and other key model parameters. While this makes it difficult for the Innovation Center to specify timelines, it provides stakeholders some flexibility to analyze and develop recommendations for the potential models over the next several months.
HMA’s experts are also closely tracking CMS’ work on additional areas identified for the agency to research. For example, CMS could consider other regulatory pathways, partnerships, or campaigns to promote the following changes:
- Opportunities to encourage price transparency for prescription drugs
- Options to improve biosimilar adoption
- Medicare fee-for-service options to support CGT access and affordability
The drug payment models build on other federal and state-level efforts to address prescription drug costs and total cost of care initiatives. For example, CMS’ drug payment model announcement comes just a week after the agency released its implementation approach for the drug payment policies approved as part of the inflation Reduction Act of 2022 (IRA) (P.L. 117-169). CMS is balancing the extensive implementation needs for the IRA while also acknowledging the new law may not directly address other value-based considerations impacting cost and access for certain prescription medications.
Below are some of the highlights of the Innovation Center’s drug payment models.
Medicare High Value Drug List Model
The Medicare High Value Drug List model would provide standardized approach to cost sharing for specified Part D medications. CMS suggests a standardized list with consistent cost-sharing to allow providers to easily identify and prescribe appropriate medications. Part D Sponsors could offer a Medicare-defined standard set of approximately 150 high-value generic drugs with a maximum co-payment of $2 for a month’s supply. Under this model, generic drugs included in the standardized list would not be subject to step therapy, prior authorization, quantity limits, or pharmacy network restrictions.
According to the report, CMS could explore leveraging existing systems, which would allow for a streamlined implementation. CMS also plans to seek input from beneficiaries, Part D Sponsors, manufacturers, and providers, but the agency did not provide a more specific timeline for announcing the Model specifications and start date.
Cell and Gene Therapy (CGT) Access
The Cell and Gene Therapy (CGT) Access model would be a voluntary opportunity for states and manufacturers. The model builds on existing state Medicaid initiatives to develop outcomes-based agreements (OBAs) with certain manufacturers of high-cost and breakthrough medications. CMS suggests the multistate test could inform a more permanent framework for evaluating, financing, and delivering CGTs on a broader scale. This model may also help address complexities with the federal drug rebate requirements in states that wish to pursue value-based contracting arrangements. Under this model a state Medicaid agency could choose to adopt the CMS structure for multi-state OBAs with participating manufacturers. CMS would be responsible for implementing, monitoring, reconciling, and evaluating financial and clinical outcomes. Initially the model would focus on CGTs for illnesses like sickle cell disease and cancer. This approach could remove some of the barriers that have slowed state uptake of OBAs.
CMS plans to begin model development in 2023, announce the model sometime in 2024-25, and test it as early as 2026.
Accelerating Clinical Evidence Model
The Innovation Center is considering mandatory participation for Medicare Part B providers in the Accelerating Clinical Evidence Model. Under this potential model, the agency would adjust Medicare Part B payment amounts for Accelerated Approval Program (AAP) drugs to determine if adjustments incentivize manufacturers to timely complete trials, which in turn may facilitate earlier availability of clinical evidence.
The Innovation Center identified some challenging aspects for this model and stated the agency will need to consult with the U.S. Food and Drug Administration (FDA) in 2023 to consider approaches for this model. Statements from agency officials about the model also indicate the need for consultation with the Medicare Payment Advisory Commission (MedPAC) and other stakeholders, including through an Advance Notice of Proposed Rulemaking.
If the Innovation Center determines this model is feasible, the agency will provide more details about a targeted launch. The Innovation Center has previously attempted to implement mandatory Part B drug payment models but never implemented them due to legal challenges and stakeholder opposition.
HMA and HMA companies will continue to analyze these potential models and initiatives developing in parallel with the Innovation Center’s work. We have the depth and breadth of expertise to assist with tailored analysis, to model policy impacts of the potential models, and to support the drafting of feedback to CMS as it considers these options.
If you have questions about the Innovation Center’s proposed models and how it will affect manufacturers, Medicare providers, Medicaid programs and patients, contact Amy Bassano ([email protected]), Kevin Kirby ([email protected]) or Andrea Maresca ([email protected]).
HMA Roundup
Alaska
Alaska Governor Proposes $9 Million to Address Medicaid Application Backlog in Fiscal 2024 Budget. KTOO reported on February 17, 2023, that Alaska Governor Mike Dunleavy is proposing $9 million in his fiscal 2024 budget to address the Medicaid and SNAP application processing backlog. The money will be used to hire contract workers to address the backlog and prepare for the upcoming Medicaid redetermination process. Read More
Arizona
Arizona to Terminate Nearly 5,300 Medicaid Providers for Non-compliance. The Arizona Health Care Cost Containment System (AHCCCS) announced on February 17, 2023, that it will terminate 5,288 Medicaid providers for non-compliance if they do not complete their revalidation process. AHCCCS informed providers in November 2022 that they had to complete the revalidation process within 90 days to remain in compliance. Read More
Arkansas
Arkansas Governor Directs DHS to Implement Medicaid Work Requirement for ARHOME. Arkansas Governor Sarah Huckabee Sanders announced on February 15, 2023, that she directed the Arkansas Department of Human Services (DHS) to implement a Medicaid work requirement for the Medicaid expansion program, Arkansas Health and Opportunity for Me (ARHOME), which covers more than 300,000 adults. The state will submit an amendment request for its ARHOME Section 1115 waiver to the Centers for Medicare & Medicaid Services for approval. DHS plans on publishing a draft amendment by April 23, with a proposed effective date of January 1, 2024. Read More
Florida
Florida Senate Committee Passes Bill to Allow Medicaid Enrollees with SMI to Bypass Step Therapy Requirements. Florida Politics reported on February 20, 2023, that the Florida Senate Health Policy Committee passed a bill that would allow Medicaid beneficiaries with serious mental illness (SMI) to bypass step therapy requirements. Step therapy refers to regulations that require beneficiaries first be prescribed less expensive drugs before more expensive options are tried. Read More
Florida Senator Files Medicaid Dental Services Legislation. The Florida Senate announced on February 20, 2023, that Senator Rosalind Osgood (D-Broward) filed a bill to expand adult dental benefits in the Medicaid state plan to cover a full array of preventive and restorative oral health services. Currently, Florida Medicaid covers only emergency dental services to alleviate pain and infection and dentures. Medicaid managed dental plans provide the full array of adult dental benefits as value-added services that are funded out of their profit margin. This bill would make those benefits standard for all adults on Medicaid and fund them through appropriation rather than through the plans’ margins. Read More
Florida Representative Proposes Medicaid Managed Care Pilot Program for Individuals with Developmental Disabilities. Health News Florida reported on February 20, 2023, that Florida Representative Wyman Duggan (R-Jacksonville) introduced legislation that would create a Medicaid managed care pilot program covering individuals with developmental disabilities. The state would select a single Medicaid managed care plan for the program, which would aim to cover individuals currently on the waiting list for the state’s home and community-based services program. Read More
Florida to Use Opioid Lawsuit Settlements to Increase Access to Treatment, Recovery Services. Health News Florida reported on February 19, 2023, that Florida Governor Ron DeSantis announced that the $205 million coming to the state from legal settlements with opioid manufacturers and distributors will be used to expand opioid treatment and recovery services statewide. Read More
Illinois
Illinois Governor Proposes Increasing HFS Funding by $709 Million for Fiscal 2024. The State Journal-Register reported on February 20, 2023, that Illinois Governor JB Pritzker is proposing an increase in funding for the Department of Healthcare and Family Services (HFS), which includes Medicaid, by $709 million to $37.2 billion in his fiscal 2024 budget. The prosed budget includes $8 million to help keep individuals enrolled in Medicaid or find other coverage following redeterminations. Read More
Iowa
Iowa to Release Medicaid Dental RFP April 24. The Iowa Department of Health and Human Services (DHHS) announced on February 13, 2023, plans to release a request for proposals (RFP) for Medicaid dental care services for the Iowa Dental Wellness Plan and Hawki programs around April 24. Proposals will be due in summer 2023, with awards expected in fall 2023. Implementation is scheduled for summer 2024. DHHS has not announced how many pre-paid ambulatory health plans will be selected. Currently, dental managed care contracts are not competitively procured. Read More
Iowa Recommends Maximizing Access to HCBS for Individuals with LTSS Needs. The Iowa Department of Health and Human Services released on January 31, 2023, an evaluation report on the state’s community-based services system (CBS), which recommends maximizing access to Medicaid home and community-based services (HCBS) and other supports for individuals with long-term service and support (LTSS) needs. The reports also recommends aligning CBS to the needs of individuals and implementing streamlined screening and improved processes. The report was conducted by Mathematica and the Harkin Institute.
Iowa Senate Considers Bill to Require Asset Test for Medicaid Coverage. The Iowa Capital Dispatch reported on February 15, 2023, that the Iowa Senate is considering a bill that would require an asset test for individuals applying for Medicaid coverage. The asset limit would match the federal asset test guidelines and would apply to both savings and property. A Senate subcommittee recommended moving the bill forward to the Health and Human Services committee. Read More
Maryland
Maryland Lawmakers Express Support for Mental Health Legislation. The Associated Press reported on February 17, 2023, that a bipartisan group of Maryland legislators expressed support for a package of mental health legislation, including a bill that would set aside $12 million to fund the state’s crisis prevention hotline currently being considered by the House. Other legislative items in the package include a bill to reimburse services provided through the collaborative care primary care model and a bill to expand access to intensive behavioral health services for children. Read More
Massachusetts
Massachusetts to Release One Care, Senior Care Options RFR in Late 2023. The Massachusetts Executive Office of Health and Human Services announced on February 21, 2023, its intent to release a request for responses (RFR) later this year for One Care and Senior Care Options (SCO), including some significant program changes. One Care, which serves dual eligible individuals ages 21 to 64, will shift from a Medicare-Medicaid Plan to a Medicare Fully Integrated Dual Eligible Special Needs Plan (FIDE SNPs) with a companion Medicaid managed care plan. SCO, which serves dual eligibles or Medicaid-only beneficiaries ages 65 and older, already consists of Medicare FIDE SNPs with companion Medicaid managed care plans. One Care incumbents are Commonwealth Care Alliance, Tufts Health Unify, and UnitedHealthcare Connected. SCO incumbents are Boston Medical Center HealthNet Plan Senior Care Options, Commonwealth Care Alliance, NaviCare, Molina/Senior Whole Health, Tufts Health Plan Senior Care Options, and UnitedHealthcare. The state is expected to include a preference for organizations that will operate both One Care and SCO plans. The contracts are expected to be effective on January 1, 2026. Read More
Michigan
Michigan Proposes New Service Delivery Model for Medicaid FFS Dental Program. State of Reform reported on February 17, 2023, that Michigan is proposing changes to its Medicaid fee-for-service (FFS) dental program, including implementing a new service delivery model for adult beneficiaries where Medicaid beneficiaries ages 21 and over will receive dental benefits through their Medicaid Health Plan or Integrated Care Organization. The state is also proposing changes to the dental benefits, provider verification process, and prior authorization requirements. If the new policy receives federal approval, it will go into effect on April 1. Read More
Mississippi
Mississippi House Passes Bill to Provide $80 Million to Hospitals Struggling Financially. The Meridian Star reported on February 19, 2023, that the Mississippi House passed a bill to provide $80 million to hospitals that are struggling financially. The state Senate has also recently passed similar legislation. The two versions will need to be reconciled. Read More
Mississippi House Republicans Reject Medicaid Expansion Budget Amendment. Mississippi Today reported on February 15, 2023, that the Mississippi House Republican majority rejected a Medicaid expansion budget bill amendment proposed by House Minority Leader Representative Robert Johnson (D-Natchez). The amendment would have prevented the budget appropriation for the Division of Medicaid from going into effect until Medicaid was expanded. Read More
Nebraska
Nebraska Senate Committee Considers Bill to Increase Medicaid Dental Reimbursement Rate. The Nebraska legislature announced on February 17, 2023, that the Senate Health and Human Services Committee is considering a 25 percent increase in the state’s Medicaid reimbursement rate for dental services. The committee heard testimony in support of the bill. Read More
New Mexico
New Mexico House Considers Medicaid Expansion Legislation. The Albuquerque Journal reported on February 21, 2023, that the New Mexico House Health & Human Services Committee is considering legislation to offer low-cost Medicaid coverage to individuals with household incomes from 133 percent to 400 percent of poverty in 2026. The bill would also appropriate funds to study the impacts of expanding Medicaid eligibility. Read More
New York
New York Has Yet to Recover $50 Million in Medicaid Overpayments Identified in December 2020 Audit. The New York State Comptroller published on February 13, 2023, an audit that found that the Office of the Medicaid Inspector General had yet to materially recover $50 million in Medicaid overpayments for services provided to dual eligibles enrolled in Medicare-covered hospice. The audit was a follow-up to a December 2020 audit that identified the overpayments. Of the initial audit’s nine recommendations, three were implemented, five were partially implemented, and one had not been implemented. Read More
North Carolina
North Carolina House Passes Medicaid Expansion Bill. The Associated Press reported on February 16, 2023, that the North Carolina House passed a Medicaid expansion bill, which now moved to the Senate. The bill instructs the state to attempt to win federal approval of work requirements.
North Carolina House Approves Medicaid Expansion Bill with Work Requirement Amendment. The Winston-Salem Journal reported on February 16, 2023, that the North Carolina House approved a Medicaid expansion bill with a work requirement amendment. It now faces a third House vote because it contains financial considerations. Read More
Oklahoma
Oklahoma to Phase In Medicaid Eligibility Redeterminations by Population. Bloomberg Law reported on February 22, 2022, that the Oklahoma Medicaid Authority announced a plan to phase in Medicaid eligibility redeterminations by population, with mothers, children, and patients with chronic health conditions redetermined last to delay potential disenrollment. The risk-based approach will redetermine individuals who rarely use Medicaid services early in the unwinding schedule while delaying the cancellation of coverage for vulnerable populations. Read More
Ohio
Ohio Senator to Introduce Bill to Provide Statewide Medicaid Coverage of Doula Services. The Sandusky Register reported on February 21, 2023, that Ohio Senator Paula Hicks-Hudson (D-Toledo) plans on introducing a bill to provide statewide Medicaid coverage of doula services. Currently, Ohio Equity Institute grants cover doula services for about 1,600 Medicaid-eligible pregnant women in Butler, Cuyahoga, Hamilton, Lorain, Lucas, Montgomery, and Summit counties. Read More
Texas
Texas Enrollment Broker Did Not Follow Procedures Re-enrolling CHIP Members, Audit Finds. The Texas Office of the Inspector General released on February 14, 2023, an audit of the state’s Medicaid and Children’s Health Insurance Program (CHIP) enrollment broker Maximus, which found that Maximus did not follow procedure for re-enrolling CHIP members who reenter the program after one year of leaving. Auditors found that all previous CHIP clients were re-enrolled in their previous MCO regardless of their last coverage period. The audit did find, however, that most requirements related to communicating and processing enrollment information were met. Maximus agreed with most of the audits findings and is in the process of developing or implementing changes. Read More
Utah
Utah Senate Passes Bill Extending Medicaid Coverage to Doula Services. State of Reform reported on February 17, 2023, that the Utah Senate passed a bill to extend Medicaid coverage of doula services during the pregnancy, childbirth, and postpartum periods. The bill now heads to the House. If passed, the Department of Health and Human Services will need to submit a state plan amendment. The state legislature is also considering legislation to expand Medicaid postpartum coverage to 12 months and increase the income eligibility threshold to 200 percent of federal poverty. Read More
Virginia
Virginia Medicaid Beneficiaries Struggle to Find Dental Providers. WSET reported on February 20, 2023, that Virginia Medicaid beneficiaries face a shortage of dental providers. Only 30 percent of dentists served Medicaid patients, according to a state report from November 2021. Meanwhile, the number of beneficiaries eligible for comprehensive dental coverage grew to over 2 million, as of August 2022, after adults become eligible in addition to children and pregnant women. Read More
West Virginia
West Virginia House Committee Recommends Bill to Create Medicaid Buy-in Program. The Weirton Daily Times reported on February 17, 2023, that the West Virginia House Health and Human Resources committee recommended a bill that would create a Medicaid buy-in program for low-income West Virginians who do not qualify for Medicaid coverage. If passed, the new option would be available January 1, 2024. The bill now goes to the House Judiciary Committee. Read More
National
CMS Seeks Corrective Action Plans from Hospitals Falling Short on Price Transparency Requirements. Fierce Healthcare reported on February 21, 2023, that the Centers for Medicare & Medicaid Services (CMS) has notified nearly 500 hospitals of failure to comply with federal price transparency requirements as of January 2023, with 230 of the notifications including requests for corrective action plans. CMS also announced plans to standardize hospital price reporting requirements and streamline enforcement efforts. Read More
Medicare Advantage Enrollment Surpasses 31 Million in February 2023. Fierce Healthcare reported on February 21, 2023, that Medicare Advantage enrollment neared 31.2 million in February 2023, an increase of over 2 million enrollees from a year earlier, according to data from the Centers for Medicare & Medicaid Services. Another 22.5 million individuals enrolled in Part D only plans. Read More
U.S. Senator Introduces Bill to Remove Ban on Physician-Owned Hospitals. U.S. Senator James Lankford (R-OK) reintroduced on February 21, 2023, Senate Bill 470, which removes the ban on creating and expanding new physician-owned hospitals (POHs) and allows POHs to participate in Medicare and Medicaid. Read More
U.S. Senators Reintroduce Legislation to Improve Coordination Between HHS, Urban Indian Organizations. U.S. Senator Tina Smith (D-MN) reintroduced on February 21, 2023, legislation with Senator Markwayne Mullin (R-OK) that would require the Department of Health and Human Services (HHS) to coordinate with urban Indian organizations on health care for American Indians and Alaska Natives living in urban areas. Read More
60 Percent of Medicaid Beneficiaries Are Not Aware of Upcoming Medicaid Redeterminations, Survey Finds. Fierce Healthcare reported on February 17, 2023, that more than 60 percent of Medicaid beneficiaries are not aware of the upcoming Medicaid redeterminations, beginning on April 1, according to a study from the Robert Wood Johnson Foundation and the Urban Institute. The survey also showed that awareness was approximately the same, regardless of the area surveyed. The survey was based on responses from Medicaid beneficiaries in December 2022. Read More
Opioid Prescriptions for Medicaid Enrollees Decreased from 2016 to 2019, Study Finds. The Kaiser Family Foundation (KFF) reported on February 17, 2023, that the percentage of Medicaid enrollees prescribed opioids declined from 11.3 percent in 2016 to 7.2 percent in 2019, while the percentage of enrollees receiving drugs to treat opioid use disorder or overdose doubled during that time period. The KFF analysis found that White Medicaid enrollees were more likely to receive opioid use disorder treatment than Black and Hispanic enrollees. Read More
U.S. Senate Committee Holds Hearing on Health Care Worker Shortage. Kaiser Health News reported on February 17, 2023, that the U.S. Senate Health, Education, Labor, and Pensions committee held a hearing on the health care worker shortage. Data shared at the hearing suggest that the shortage could rise to 450,000 nurses and 120,000 doctors in the coming years. The committee is hoping to produce bipartisan legislation. Read More
U.S. Senator Introduces Bill to Allow States to Disqualify Abortion Providers from Medicaid. The Daily Citizen reported on February 17, 2023, that U.S. Senator James Lankford (R-OK) introduced legislation that would allow states to revoke Medicaid “qualified provider” status from any provider or organization that provides abortion services, including Planned Parenthood. U.S. Congressman Michael Cloud (R-TX) plans to introduce a similar bill in the House. Read More
U.S. Senators Work on PBM Reform. Fierce Healthcare reported on February 16, 2023, that the U.S. Senate Commerce Committee held a hearing on pharmacy benefit managers (PBMs) as part of an ongoing reform and transparency effort. Other topics under discussion included the consolidation of the PBM market and PBMs steering patients to their own pharmacies. Read More
U.S. Lawmakers Voice Support for Proposed Medicare Advantage Rule. Becker’s Payer Issues reported on February 16, 2023, that a group of 70 federal lawmakers submitted a statement of support for the Centers for Medicare & Medicaid Services (CMS) proposed rule to improve prior authorization in the Medicare Advantage (MA) program. The rule would also require MA plans to cover services from any provider that accepts Medicare payments and prompt CMS to develop more accurate risk scoring models for the MA program. In the letter, lawmakers also called on CMS to implement further reforms to MA. Read More
Industry News
Amazon Completes Acquisition of One Medical. Modern Healthcare reported on February 22, 2023, that Amazon completed its $3.9 billion acquisition of One Medical, a primary care provider, following a decision by federal regulators not to block the deal. The deal was announced in July 2022. Read More
Health Connect America Acquires First Home Care, North Star Counseling of Central Florida. Health Connect America announced on February 22, 2023, its acquisitions of First Home Care and North Star Counseling of Central Florida. Health Connect America, which provides behavioral health services, will now reach more than 21,000 children and their families in seven southeast states. Read More
HAP Announces Joint Venture with CareSource. Health Alliance Plan (HAP) announced on February 21, 2023, a joint venture with Ohio-based CareSource in hopes of covering more Medicaid members across Michigan. HAP currently has 43,000 Medicaid members. The partnership will also offer Exchange coverage. Read More
Privia Health, Community Medical Group Launch Privia Quality Network of Connecticut. Privia Health announced on February 17, 2023, its partnership with Community Medical Group to launch Privia Quality Network of Connecticut (PQN CT), which will be the largest clinically integrated network (CIN) in the state. The CIN is made up of 1,100 multi-specialty providers in over 450 locations. PQN CT will serve approximately 29,000 Medicare beneficiaries, with over 10,000 participating in the Medicare Shared Savings Program for 2023. Read More
BCBS-LA Establishes $3 Billion Foundation to Address Health Equity. Becker’s Payer Issues reported on February 16, 2023, that Blue Cross Blue Shield of Louisiana is establishing a $3 billion foundation to address health equity and to disperse funds to some members. The funding comes from its acquisition by Elevance Health. Read More
CommonSpirit Health Acquires Steward Health Care’s Utah Care Sites. Nonprofit, Catholic health system CommonSpirit Health announced on February 15, 2023, that it will acquire Steward Health Care’s Utah care sites, which include five hospitals, more than 35 medical group clinics, and a network of providers. Centura Health, which CommonSpirit jointly sponsors with AdventHealth, will manage the assets. The transaction is expected to close later this year. Read More
HouseWorks Acquires Amedisys’ Personal Care Division. HouseWorks announced on February 15, 2023, its acquisition of the personal care division at Amedisys, a provider of home health, hospice, and high-acuity care. HouseWorks provides personal care services in Massachusetts, New Hampshire, Pennsylvania, and Maine. The acquisition is expected to close in the second quarter of 2023. Read More
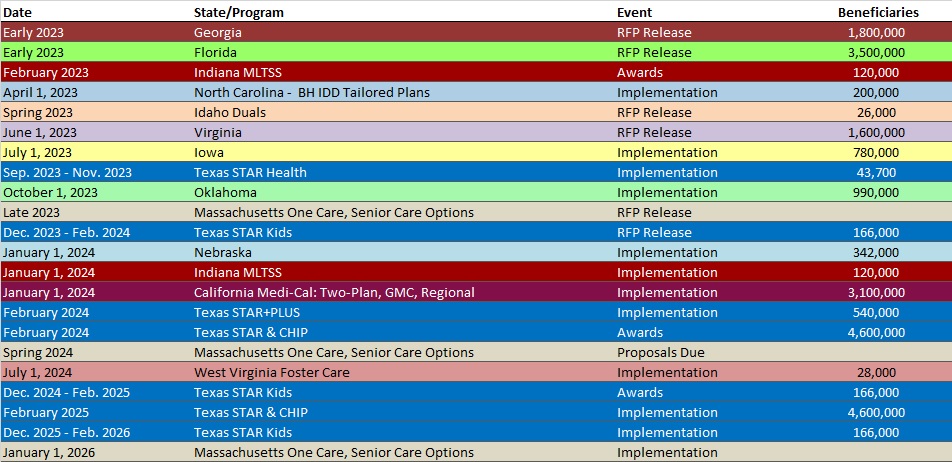
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Up 6.5%, Nov-22 Data
- Colorado RAE Enrollment is Up 7.1%, Nov-22 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 5.6%, Oct-22 Data
- Georgia Medicaid Managed Care Enrollment is Up 1%, Feb-23 Data
- Iowa Medicaid Managed Care Enrollment is Up 6.1%, 2022 Data
- Kansas Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- New York Medicaid Managed Care Enrollment is Up 4.6%, 2022 Data
- Ohio Medicaid Managed Care Enrollment is Up 0.5%, Nov-22 Data
- Oklahoma Medicaid Enrollment is Up 13.6%, 2022 Data
- Oklahoma SNP Membership at 40,469, Mar-22 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 6.5%, 2022 Data
- South Dakota Medicaid Enrollment is Up 9.4%, FY 2022 Data
- Tennessee Medicaid Managed Care Enrollment is Up 5.8%, 2022 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Pharmacy Administrative Services RFP, Feb-23
- Idaho MMIS Systems Integrator RFI, Feb-23
- Minnesota Homelessness Assistance Grants RFP, Feb-23
Medicaid Program Reports, Data, and Updates:
- Arizona Medicaid Annual Reports, 2014-22
- Iowa HHS Recommendations for Strengthening Iowa’s Community-Based Services System Report, Jan-23
- Iowa Medical Assistance Advisory Council Meeting Materials, 2016-22
- Nebraska DHHS Division of Behavioral Health Annual Reports, FY 2013-22
- Nevada Biennial Report on the Condition, Operation, and Functioning of Medicaid, 2022
- Nevada Medicaid Managed Care Actuarial Rate Certifications, CY 2016-22
- Nevada Medicaid Managed Care Quality Strategy Reports, 2014-2024
- New Mexico External Quality Review Reports, 2016-20
- Oklahoma Health Care Authority Annual Reports, 2014-22
- Texas HHS Presentations to Legislative Committees, Feb-23
- Texas Medicaid Managed Care Advisory Committee Annual Reports, 2020-22
- Texas Nursing Facility Workforce Challenges Report, Nov-22
- West Virginia Medicaid Mountain Health Trust Annual Reports, SFY 2011-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
