HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Arizona Releases Medicaid ALTCS-EPD Program RFP

- Colorado Hospitals Continue to Post Operating Losses

- Florida Projects $600 Million Medicaid Budget Deficit for Fiscal 2024

- Medicaid Eligibility Redeterminations News: Florida, Illinois, Massachusetts, Michigan, Nevada, Rhode Island, Wyoming

- Idaho Medicaid Managed Care Task Force Holds Second Hearing

- Illinois Governor Signs Law Increasing Oversight of Healthcare Mergers

- Indiana Parents, Advocates Call on Governor to Reconsider Funding Cut for Autism Therapy

- Massachusetts to Raise Income Eligibility Limits for ConnectorCare

- Nebraska to Lift $750 Cap on Medicaid Dental Benefits

- New Mexico to Award Previously Announced Medicaid Plan Contracts in Defeat for Governor

- New York City Cannot Switch Retirees to Aetna Medicare Advantage Plan, Judge Rules

- North Carolina Medicaid Behavioral Health Plans Sandhills Center, Eastpointe to Merge

- Vermont All-Payer ACO Model Lowers Medicare Spending, Hospitalizations, Analysis Finds

- CMS Launches Changes to Encourage Participation in Medicare ACO REACH

- 4.8 Million Medicaid Beneficiaries Are Disenrolled from Medicaid Following Redeterminations, Analysis Finds

- 5.6 Million Medicaid Enrollees Utilize Long-term Services, Supports in 2020, KFF Finds

- U.S. Appeals Panel Rules False Claims Lawsuit Against Walgreens Can Proceed

In Focus
Arizona Releases Medicaid ALTCS-EPD Program RFP
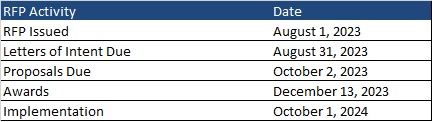
This week, our In Focus section reviews the Arizona Long Term Care System (ALTCS) Elderly and Physically Disabled (EPD) Program request for proposals (RFP), which the Arizona Health Care Cost Containment System (AHCCCS) released on August 1, 2023. The ALTCS-EPD program covers 26,000 individuals, representing approximately 38 percent of the ALTCS managed care population. The remaining ALTCS members are covered under a state-run model through the Department of Economic Security, Division of Developmental Disabilities (DES/DDD) health plans, which provide long-term care (LTC) to individuals with intellectual/developmental disabilities. Contracts for ALTCS-EPD are worth approximately $1.6 billion and will take effect October 1, 2024.
Background
ALTCS is one of the oldest Medicaid managed long-term services and supports (MLTSS) programs in the country, providing integrated physical health, behavioral health, and LTSS to individuals who are 65 years of age or older or who have a disability and require nursing facility level care. Beneficiaries may live in assisted living facilities or receive in-home services. The ALTCS-EPD program covers nearly all Arizonans who are dually eligible for Medicaid and Medicare statewide. Winning managed care organizations (MCOs) also will be required to implement companion Medicare Advantage Fully Integrated D-SNPs (FIDE SNPs) effective January 1, 2025.
Market
Members receive coverage through Banner-University Family Care, Mercy Care Plan, and UnitedHealthcare, depending on their geographic service area (GSA). MCOs will bid on all three GSAs and indicate their order of preference to be awarded. AHCCCS will not award the South GSA only or the North GSA only. At present, in the South region, Mercy Care Plan serves Pima County only. Under the new RFP, AHCCCS will not make an award specific to Pima County; rather the MCO will serve all seven counties within the South GSA.
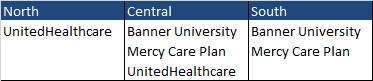
Together, the plans cover 25,973 individuals (see below).
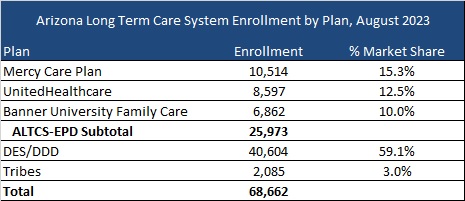
(United and Mercy administer DDD plans.)
Timeline
Intent to bid forms are due by August 31. Proposals are due October 2, and awards are expected to be announced December 13. As noted previously, implementation is scheduled to begin October 1, 2024.
HMA Roundup
Arizona
Arizona Expands Investigation Into Medicaid Provider Fraud. Native News Online reported on August 10, 2023, that Arizona has expanded an investigation into Medicaid provider fraud targeting Native Americans. More than 100 providers are now under investigation.
Colorado
Colorado Hospitals Continue to Post Operating Losses. The Colorado Sun reported on August 15, 2023, that approximately half of Colorado’s hospitals continue to lose money on patient care, according to the Colorado Hospital Association. First quarter financial 2023 filings suggest some larger hospitals with more resources returned to profitability. Read More
Delaware
Delaware Medicaid to Cover Doula Services By January 2024. Delaware Public Media reported on August 11, 2023, that Delaware Medicaid will cover doula services under a new law. Services must be covered by January 1, 2024. Read More
Florida
Florida Projects $600 Million Medicaid Budget Deficit for Fiscal 2024. Florida Politics reported on August 14, 2023, that the Florida Agency for Health Care Administration (AHCA) has projected a Medicaid budget deficit of nearly $600 million for the current fiscal year, ending June 30, 2024. The state’s share of the shortfall is about $227 million. AHCA further projects the program will require an additional $934 million in fiscal 2025. The deficit stems in part because the state assumed higher disenrollments following the resumption of Medicaid eligibility redeterminations. Read More
Florida May Be Non-compliant With Federal Requirements on Medicaid Eligibility Redeterminations, CMS Says. The Florida Phoenix reported on August 15, 2023, that Florida may be non-compliant with federal requirements concerning Medicaid eligibility redeterminations, including long call center wait times and abandoned calls, according to a letter from the Centers for Medicare & Medicaid Services (CMS). Healthcare policy groups in the state held a press call to raise concerns. Read More
Idaho
Idaho Medicaid Managed Care Task Force Holds Second Hearing. The Idaho Press reported on August 9, 2023, that Idaho legislators held a second round hearing on the potential transition to Medicaid managed care, with provider organizations voicing concerns and calling for a continuation of the existing value-based approach. The Medicaid Managed Task Force, co-chaired by Senator Julie VanOrden (R-Pingree) and Representative John Vander Woude (R-Nampa), will meet again on August 31. Read More
Illinois
Illinois May Be Non-compliant With Federal Requirements on Medicaid Eligibility Redeterminations, CMS Says. Health News Illinois reported on August 16, 2023, that Illinois is experiencing long wait times and high call abandonment rates at call centers handling Medicaid eligibility redeterminations. The Centers for Medicare & Medicaid Services (CMS) said in a letter to the state that individuals may be impeded from renewing Medicaid and Children’s Health Insurance Plan coverage. Read More
Governor Signs Law Increasing Oversight of Healthcare Mergers. Health News Illinois reported on August 14, 2023, that Illinois Governor JB Pritzker signed a law aimed at increasing oversight of healthcare mergers, including providing the state with advance notice of merger and acquisition plans. The law is effective January 2024. Read More
Illinois to Implement Recommended Changes to Children’s Behavioral Health. Health News Illinois reported on August 14, 2023, Illinois Governor JB Pritzker signed legislation to implement recommendations aimed at improving behavioral healthcare for children. The recommendations, which were released in February 2023 by the Illinois Children’s Behavioral Health Transformation Initiative, include establishment of a centralized intake portal to provide families guidance and referrals to state and community-based programs, creation of a navigator assistance program, and statutory language to pave the way for annual mental health screenings to all K-12 students. Read More
Illinois to Seek $601 Million in Missed Federal Medicaid Matching Funds. Health News Illinois reported on August 14, 2023, that Illinois is looking to recoup $601 million in federal Medicaid matching funds the state failed to claim for the period covering the end of 2020 through June 2022. The state blamed a computer error for the missed claims, which were for services provided to individuals with developmental disabilities. Read More
Indiana
Indiana Parents, Advocates Call on Governor to Reconsider Funding Cut for Autism Therapy. Fox59 reported on August 11, 2023, that advocacy group Indiana ACT for Families, comprised of nearly 60 parents and advocates, signed a letter addressed to Indiana Governor Eric Holcomb calling for a halt to potential funding cuts of up to 50 percent for Applied Behavior Analysis Therapy (ABA) for autism. Indiana Medicaid provided 6,200 children with ABA services in 2022. Read More
Massachusetts
Massachusetts to Raise Income Eligibility Limits for ConnectorCare. WBUR reported on August 15, 2023, that the Massachusetts Health Connector, the state’s Exchange, announced plans to raise income eligibility limits from 300 percent of the federal poverty level to 500 percent as part of a two-year pilot aimed at increasing Exchange plan enrollment. The pilot, which is effective on January 1, is expected to reach an additional 50,000 people. The changes were approved by the Connector board on an emergency basis; public hearings will be held over the next few months. Read More
Massachusetts Disenrolls 33,989 Medicaid Beneficiaries During June Redeterminations. The Massachusetts Executive Office of Health and Human Services reported on August 9, 2023, the disenrollment of 33,989 Medicaid beneficiaries during June redeterminations, including 9,081 due to procedural reasons. Coverage was renewed for 57,176 beneficiaries.
Michigan
Michigan Disenrolls 22,911 Medicaid Beneficiaries Following June, July Redeterminations. Michigan Radio reported on August 15, 2023, that Michigan disenrolled 22,911 Medicaid beneficiaries following June and July redeterminations. The state renewed coverage for 224,757 beneficiaries. Read More
Minnesota
Minnesota Governor Launches Task Force on Future of UMN Health System. The Minnesota Daily reported on August 10, 2023, that Governor Tim Walz signed an executive order to launch a state task force on the future of the University of Minnesota (UMN) Health Care System. A summary of recommendations is due by January 15, 2024. Read More
Nebraska
Nebraska to Lift $750 Cap on Medicaid Dental Benefits. Nebraska Public Media reported on August 10, 2023, that Nebraska will lift a $750 annual cap on Medicaid dental benefits in January 2024 among other changes in hopes of improving access to dental care and compensation for dentists. In 2022, 378 dentists in Nebraska served at least one Medicaid beneficiary, down from nearly 600 dentists in 2017. Read More
Nevada
Nevada Launches Eligibility Redeterminations Data Dashboard. FOX5 reported on August 9, 2023, that the Nevada Department of Health and Human Services has launched a redeterminations data dashboard with monthly snapshots of enrollment changes, application processing, renewal outcomes, and call wait times. Read More
New Jersey
New Jersey to Provide $1.5 Million in Grants to Help Enroll Eligible Children in Medicaid. Insider NJ reported on August 10, 2023, that the New Jersey Department of Human Services will provide $1.5 million in grants through the state’s Cover All Kids Initiative to enroll eligible, uninsured children in Medicaid. Up to six grants of $250,000 each are expected to be announced in the fall. Applicants must submit a statement of intent to apply by August 11, 2023, and proposals must be submitted by September 1, 2023. Read More
New Mexico
New Mexico to Award Previously Announced Medicaid Plan Contracts in Defeat for Governor. The Santa Fe New Mexican reported on August 10, 2023, that New Mexico will release notices of intent to award contracts to four previously selected Medicaid managed care plans: Blue Cross and Blue Shield of New Mexico; UnitedHealthcare of New Mexico; Molina Healthcare of New Mexico, Inc.; and Presbyterian Health Plan. Contract implementation is set for July 1, 2024. The state ethics commission reached an agreement with Governor Michelle Lujan Grisham to reverse her unilateral decision to cancel the request for proposals and block the awards. Read More
New York
New York City Cannot Switch Retirees to Aetna Medicare Advantage Plan, Judge Rules. Beckers Payer Issues reported on August 14, 2023, that a New York Supreme Court judge permanently blocked New York City from switching 250,000 retired individuals and their dependents from traditional Medicare to an Aetna Medicare Advantage Plan. The contract was worth $15 billion over five years. The city plans to appeal the judge’s decision. Read More
Fidelis Care to Expand Medicaid Advantage Plus Plan to Three More New York Counties. Fidelis Care announced on August 9, 2023, that it will expand its Wellcare Fidelis Dual Plus Medicaid Advantage Plus plan into Westchester, Nassau, and Suffolk counties. Fidelis Care now offers Wellcare Fidelis Dual Plus in 52 New York counties. Read More
North Carolina
North Carolina Medicaid Behavioral Health Plans Sandhills Center, Eastpointe to Merge. North Carolina Health News reported on August 14, 2023, that Sandhills Center and Eastpointe, two of the six North Carolina Local Management Entity-Managed Care Organizations covering behavioral health, have announced plans to merge. The new entity would serve more than 100,000 people in 21 counties. Read More
Rhode Island
Rhode Island Announces Availability of $100,000 in Additional Grants for Medicaid Eligibility Redeterminations Outreach. Rhode Island announced on August 9, 2023, the availability of a second round of grants totaling $100,000 for community organizations to assist in Medicaid eligibility redeterminations outreach. Organizations may apply to the state Executive Office of Health and Human Services for up to $4,950 each. Read More
Texas
Texas Seeks Repayment of More Than $17 Million in Medicaid Funds from Planned Parenthood. The Associated Press reported on August 15, 2023, that Texas is looking to recoup more than $17 million plus fines from Planned Parenthood, alleging in a lawsuit that the organization improperly received Medicaid payments before being removed from the program in 2021. A hearing in the false claims case was set for today. Read More
Vermont
Vermont All-Payer ACO Model Lowers Medicare Spending, Hospitalizations, Analysis Finds. AJMC reported on August 11, 2023, that the Vermont all-payer accountable care organization (ACO) model reduced Medicare spending and hospitalizations from 2018 to 2021, while improving patient care, according to an analysis from NORC at the University of Chicago. The voluntary model promotes risk-sharing and population-based payments for hospitals. Read More
Wyoming
Wyoming Disenrolls 10,100 Enrollees for Procedural Reasons. Wyoming News Now reported on August 15, 2023, that Wyoming disenrolled 10,100 Medicaid beneficiaries for procedural reasons since eligibility redeterminations began in April. Read More
National
4.8 Million Medicaid Beneficiaries Are Disenrolled from Medicaid Following Redeterminations, Analysis Finds. Kaiser Family Foundation released an analysis on August 15, 2023, showing that nearly 4.8 million Medicaid beneficiaries have lost coverage across 42 states and the District of Columbia since the reinstatement of eligibility redeterminations. Of enrollees who applied for Medicaid coverage renewals, 38 percent were disenrolled and 62 percent maintained coverage. Overall, 75 percent of those disenrolled lost coverage due to procedural reasons. Read More
CMS Launches Changes to Encourage Participation in Medicare ACO REACH. Modern Healthcare reported on August 14, 2023, that the Centers for Medicare & Medicaid Services (CMS) will raise financial reserve requirements and reduce enrollment minimums as part of an effort to encourage provider participation in the Medicare Accountable Care Organization Realizing Equity, Accountability and Community Health (ACO REACH) program. Under the program, which launched this year, providers form ACOs to manage care for traditional Medicare members, receive capitated payments, and take shared or full risk. Read More
5.6 Million Medicaid Enrollees Utilize Long-term Services, Supports in 2020, KFF Finds. KFF reported on August 14, 2023, that 5.6 million people utilized Medicaid long-term services and supports (LTSS) in 2020. About 4 million (72 percent) utilized home and community based care, 1.4 million (24 percent) utilized institutional care, and 200,000 (4 percent) used both. Individuals utilizing LTSS comprised 6 percent of Medicaid enrollment but 37 percent of federal and state Medicaid spending. Read More
CMS Seeks Public Comment on Technical Specifications of Certain LTSS Quality Measures. The Centers for Medicare & Medicaid Services (CMS) announced on August 15, 2023, that it is seeking public comments on technical specifications for long-term services and supports (LTSS) assessment and care planning measures and for LTSS rebalancing and utilization measures. The comment period closes on August 28, 2023. Read More
Prices Have Tripled for Top 25 Medicare Part D Drugs, Report Finds. Axios reported on August 11, 2023, that prices have tripled for the top 25 Medicare Part D drugs since first hitting the market, according to a report from AARP. Top drugs are defined as those that accounted for the most Medicare Part D spending in 2021. Read More
House Bill Would Allow States to Hire Outside Contractors to Help with Medicaid Eligibility Redeterminations. Becker’s Payer Issues reported on August 11, 2023, that U.S. Representatives Earl Carter (R-GA) and Neal Dunn (R-FL) introduced legislation that would allow state agencies to hire outside contractors to help with Medicaid eligibility redeterminations. The Medicaid Staffing Flexibility and Protection Act, which was introduced in the House Energy and Commerce committee, targets coverage losses for procedural reasons. Read More
Medicaid FFS Coverage of Substance Use Disorder Treatment Improves, Study Finds. JAMA Network published on August 11, 2023, a study showing that coverage of substance use disorder treatment for Medicaid fee-for-service (FFS) beneficiaries improved from 2014 to 2021. Meanwhile, prior authorization restrictions declined. Read More
Federal Regulators Push States to Improve Medicaid Redeterminations Compliance. Becker’s Payer Issues reported on August 11, 2023, that the U.S. Department of Health and Human Services has indicated that 36 states are failing to meet at least one of three key regulatory requirements for Medicaid eligibility redeterminations, and five (Alaska, Florida, New Mexico, Montana, and Rhode Island) were deficient in all three categories. Categories include call center wait times, rates of procedural terminations, and application approval wait times. Read More
Over Half a Million Children Lose Medicaid Coverage Since April Redeterminations. Bloomberg Law reported on August 11, 2023, that since redeterminations resumed in April more than half a million children have lost Medicaid coverage, according to data compiled by the Georgetown Center for Children and Families. Florida, Ohio, and Washington were among the states showing heavy losses. Results may be understated because several major states have not yet released their redetermination numbers on children. Read More
CMS Releases Toolkit Aimed at Improving Quality, Access to Postpartum Care in Medicaid, CHIP. The Centers for Medicare & Medicaid Services released on August 10, 2023, a toolkit aimed at enhancing equity, quality, and access to postpartum care in Medicaid and the Children’s Health Insurance Program (CHIP). The toolkit includes strategies for states in partnering with managed care plans and better utilizing existing authorities. Read More
Medicare Advantage Plans to Receive $12.8 Billion in Quality Bonus Payments in 2023, Analysis Finds. KFF released on August 9, 2023, an analysis showing that Medicare Advantage plans will receive a minimum of $12.8 billion dollars in quality bonus payments from the federal government in 2023, up nearly 30 percent from the prior year. About 85 percent of Medicare Advantage recipients are in plans receiving bonus payments, which reflect quality ratings from 2022. Read More
Medicare Advantage Enrollment is Highly Concentrated, KFF Finds. KFF reported on August 9, 2023, that Medicare Advantage enrollment is highly concentrated, with United Healthcare and Humana alone serving about 47 percent of all 2023 enrollees. Read More
Industry News
U.S. Appeals Panel Rules False Claims Lawsuit Against Walgreens Can Proceed. Reuters reported on August 15, 2023, that a federal appeals panel ruled that a Medicaid false claims lawsuit against Walgreens can proceed, overturning a lower court ruling. The case involves allegations that a Walgreens clinical pharmacy manager in Tennessee falsified patient records to obtain approval from Virginia Medicaid for hepatitis C drugs between January 2015 and June 2016. Read More
Enrollment at Top 5 Medicaid Managed Care Organizations Falls 576,000 in 2Q23. Axios reported on August 14, 2023, that Medicaid enrollment fell 576,400 or 1.3 percent in the second quarter of 2023 at the nation’s top five Medicaid managed care organizations, according to a report from the Georgetown University Center for Children and Families. The five organizations included in the tally were Centene, CVS Health, Elevance Health, Molina Healthcare, and UnitedHealth Group. Read More
UnitedHealth Acquisition of Amedisys to Be Delayed as Justice Seeks Additional Information. Fierce Healthcare reported on August 11, 2023, that UnitedHealth Group’s proposed $3.3 billion acquisition of Amedisys will be delayed following a request from the U.S. Department of Justice for additional information about the transaction. Amedisys revealed the request in a securities filing. Read More
RFP Calendar

HMA News & Events
Upcoming HMA Webinar:
Medicaid 1115 Justice Waivers and Special Populations: Meeting the Needs of Justice-Involved Youth. Youth in detention often have complex medical, behavioral health, developmental, social, and legal needs and have been exposed to adverse childhood experiences. Part 5 of this series on 1115 Medicaid Justice Demonstration Waivers: Bridging Healthcare, will delve into differences of care and services for youth so that a whole-person approach can be applied to their successful reentry to the community. Thursday, August 17, 2 pm ET.
Medicare Policy Changes Impacting Behavioral Health Services Workforce and Population Health. With recent rule changes proposed by the Centers for Medicare and Medicaid Services (CMS) addressing expanding access to behavioral health services, this webinar will focus on how those changes will impact the already strained workforce, and corresponding impacts on population health. HMA Experts will dive deeper into approaches to handle workforce shortages while expanding access. Tuesday, September 12, 12pm ET
Wakely, an HMA company, White Paper:
2022 Supplemental Claims Impact: Risk score capture and accuracy through supplemental claims continues to be an industry hot topic. Supplemental files allow issuers to ensure accurate coding for risk scoring, thus impacting risk adjustment transfers in the ACA market. In addition, supplemental files also help issuers mitigate risk adjustment data validation (RADV) audit risk for both “under-coding” and “over-coding” by correcting data within their claims system.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Down 1.2%, May-23 Data
- Louisiana Medicaid Managed Care Enrollment is Down 1%, Jun-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 2.2%, Jul-23 Data
- New Jersey Medicaid Managed Care Enrollment is Up 3.3%, May-23 Data
- New Jersey Medicaid Managed Care Enrollment is Up 2.4%, Apr-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 0.3%, Jun-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 1.9%, May-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 2.1%, Apr-23 Data
- Tennessee Medicaid Managed Care Enrollment is Up 1.6%, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Arizona Long Term Care System RFP and Q&A, Aug-23
- California Medicare Advantage D-SNP Model Contracts, 2021-24
- New York Medicare Advantage D-SNP Model Contracts, 2022-24
Medicaid Program Reports, Data, and Updates:
- Idaho PHE Medicaid Unwinding Monthly Report to CMS, Jul-23
- Indiana PHE Medicaid Redeterminations Monthly Report to CMS, Jul-23
- Kansas PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Maine PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Massachusetts PHE Medicaid Redeterminations Monthly Reports to CMS, Jun-23
- Michigan PHE Medicaid Redeterminations Monthly Reports to CMS, Jul-23
- Missouri HealthNet Managed Care Rates, SFY 2023
- Ohio PHE Medicaid Redeterminations Monthly Report to CMS, Jul-23
- Texas HHSC Medicaid Rate Setting Reports, FY 2024
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
