This week, our In Focus section provides a high-level overview and an analysis for how health plans should consider two related and significant policy statements from the Centers for Medicare & Medicaid Services (CMS) about opportunities to further integrate care for dually eligible individuals. Specifically, the CMS April 24, 2019, State Medicaid Director letter (SMDL) outlines new opportunities for states, largely working with health plans, to test models of integrated care, including opportunities to continue current financial alignment initiatives (FAIs).[i] CMS also issued final rules related to Medicare Advantage Dual Eligible Special Needs Plan (D-SNP) definitions and requirements for Medicare-Medicaid integration activities and unified grievances and appeals for calendar year 2021.[ii] Together, these guidance documents should present greater opportunities for health plans to partner with CMS and states to integrate care for dual eligible beneficiaries.[iii]
1247 Results found.

HMA Collaborates on Connecticut HEC Initiative
The Connecticut Office of Health Strategy and Department of Public Health recently announced that the State Innovation Model (SIM) Healthcare Innovation Steering Committee has approved the Health Enhancement Community (HEC) initiative proposed framework. This blueprint is designed to build or expand collaborations across the state to improve healthy weight and physical fitness, advance child well-being, and strengthen health equity. The HEC initiative will further residents’ health and well-being by addressing both clinical need and the social determinants that impact overall health.

Texas 2020-21 Biennium Budget Overview
This week, our In Focus section reviews the Texas 2020-21 biennium budget. The Texas Legislature adjourned its biennial legislative session on May 27, 2019, after adopting a $250.6 billion budget (all funds). The total budget is 6.3 percent higher than the 2018-19 budget with an increase of $14.8 billion.

It Takes a Village: How to Coordinate and Pay for a Community Response to Health Inequities
This week, our In Focus section reviews the Pathways HUB model, an approach designed to help coordinate outreach by specialized community health workers who are incentivized to engage high-need populations. An HMA webinar, held May 9, 2019, with Mark Redding, co-developer of the Pathways HUB model, and Heidi Arthur, HMA can be viewed here.

HMA Analysis of Modernizing Part D and Medicare Advantage to Lower Drug Prices and Reduce Out-of-Pocket Expenses Final Rule
On May 16, 2019, the Centers for Medicare & Medicaid Services (CMS) issued its final rule, Modernizing Part D and Medicare Advantage to Lower Drug Prices and Reduce Out-of-Pocket Expenses (Final Rule). The proposed rule, which was issued in November 2018, included a number of provisions intended to improve drug price transparency and expand use of utilization management tools to further Medicare Advantage and Part D cost-cutting efforts. However, in response to significant pushback from beneficiary advocates, physician groups, insurers, and pharmaceutical stakeholders, CMS elected not to implement key provisions. These include proposals to allow Part D plans to exclude protected class drugs from formularies as a result of price increases or if the drug is a new formulation of an existing single-source drug as well as proposed reforms to pharmacy price concessions that would require discounts be passed on to beneficiaries at the point of sale. Commenters in opposition to the pharmacy price concession proposal contend that these reforms would result in higher Part D premiums. While CMS has postponed addressing this provision in this Final Rule, the recently issued Department of Health and Human Services (HHS) Office of Inspector General (OIG) proposed rule, if finalized, may include fundamental changes to these pricing arrangements and other federal safe harbors to the anti-kickback statute.

Kentucky Releases Medicaid MCO RFP
This week, our In Focus section reviews the Kentucky Medicaid managed care organizations (MCOs) request for proposals (RFP), issued by the Kentucky Finance and Administration Cabinet on May 16, 2019. The Kentucky Cabinet for Health and Family Services (CHFS), Department for Medicaid Services (DMS) will select up to five Medicaid MCOs to manage health care services for more than 1.2 million people, starting July 2020. Contracts are estimated at more than $7 billion.

Medicaid Plan Profit Margin Dips to 0.5 Percent in 2018, Continuing Multi-Year Decline, HMAIS Analysis Shows
This week, our In Focus summarizes the findings of an HMA Information Services analysis of Medicaid managed care plan profitabilty, based on data from annual statutory filings made with the National Association of Insurance Commissioners (NAIC). For information on how to subscribe to HMA Information Resources, contact Carl Mercurio.
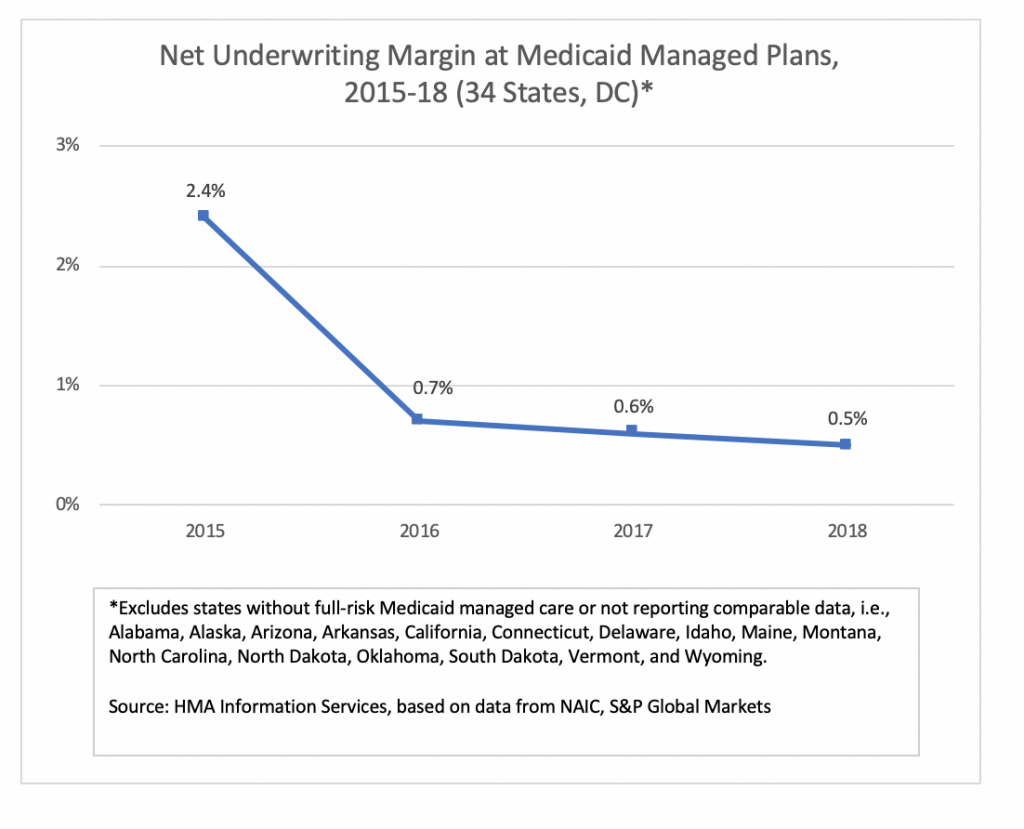
Underwriting Margin
An analysis by HMA Information Services, a division of Health Management Associates, shows that Medicaid managed care plans in 34 states and Washington, DC, posted a net underwriting margin of 0.5 percent in 2018, down 10 basis points from 0.6 percent in 2017. For-profit plans posted higher underwriting margins than not-for-profit plans.
Overall, margins have fallen consistently since hitting a four-year high of 2.4 percent in 2015. The data include financial information for about 210 Medicaid managed care plans, with total membership of 37 million in 2018 and revenues of about $188 billion. Net underwriting profit in 2018 was about $911 million, compared to more than $990 million in 2017.
States in which the aggregate Medicaid managed care margin was below the national average in 2018 (based on plans reporting NAIC statutory filings) included Florida, Hawaii, Louisiana, Massachusetts, Mississippi, New Jersey, New Mexico, Rhode Island, Texas, and Virginia.
Not included in the tally are most Medicaid plans in California and Arizona, which don’t report financial information through NAIC. In addition, some of the largest plans in New York don’t report financial information through NAIC.
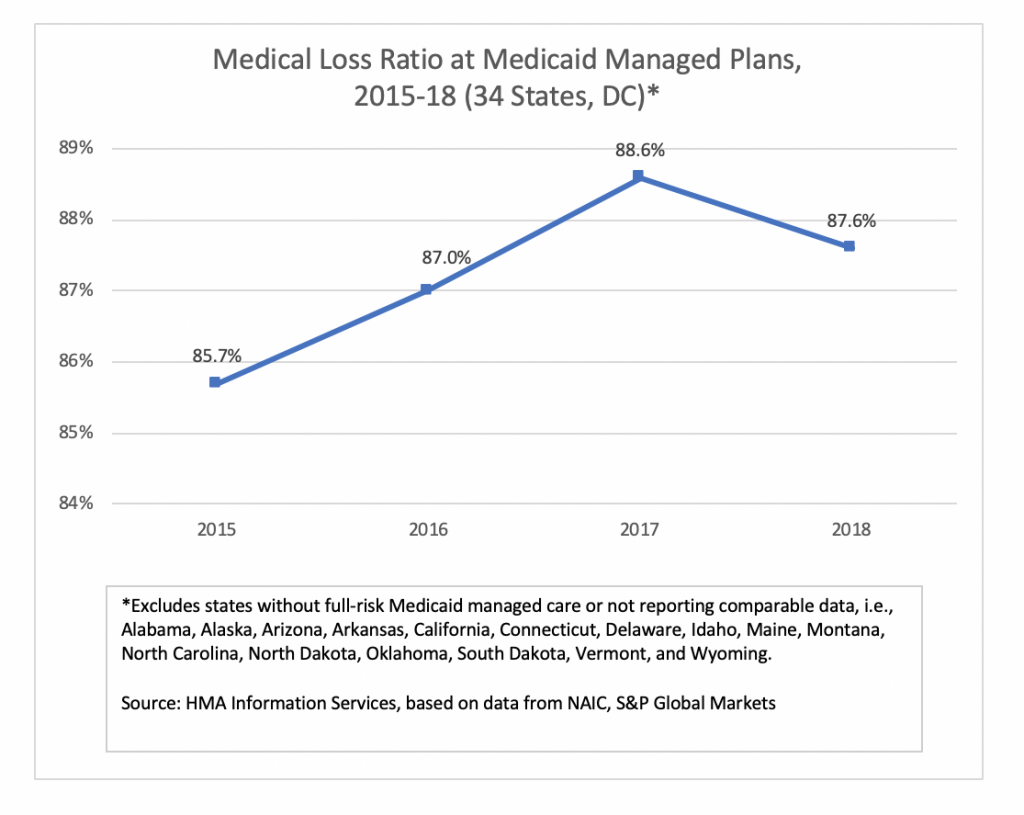
Medical Loss Ratio
Medical loss ratio (MLR) among Medicaid managed care plans in 34 states and Washington, DC, was 87.6 percent in 2018, down about 100 basis points from 2017. The MLRs calculated by HMAIS are blended and may include traditional Medicaid, expansion, and aged, blind and disabled populations, depending on the state. The improvement in average MLR was offset by an increase in administrative costs, resulting in the drop in underwriting margin.

Medicaid and Exchange Enrollment Update – January 2019
This week, our In Focus section reviews updated information issued by the Department of Health & Human Services (HHS) Centers for Medicare & Medicaid Services (CMS) on Medicaid expansion enrollment from the “January 2019 Medicaid and CHIP Applications, Eligibility Determination, and Enrollment Report,” published on April 25, 2019. Additionally, we review 2019 Exchange enrollment data from the “Health Insurance Exchanges 2019 Open Enrollment Period: Final State-Level Public Use File,” published by CMS on March 25, 2019. Combined, these reports present a picture of Medicaid and Exchange enrollment in 2019, representing 72.4 million Medicaid and CHIP enrollees and 11.4 million Exchange enrollees.

HMA MACPAC report, care coordination in integrated care programs serving dually eligible beneficiaries
A team of HMA colleagues including Sarah Barth, Sharon Silow-Carroll, Esther Reagan, Mary Russell and Taylor Simmons completed a study for the Medicaid and Children’s Health Insurance Program (CHIP) Payment and Access Commission (MACPAC) to examine care coordination requirements for several Medicare-Medicaid integrated care models.
The study’s final report, Care Coordination in Integrated Care Programs Serving Dually Eligible Beneficiaries – Health Plan Standards, Challenges and Evolving Approaches, is posted to the MACPAC website.

HMA Summary of Fiscal Year 2020 Medicare Proposed Rules for Medicare Part A Providers
This week, our In Focus section reviews the Centers for Medicare & Medicaid Services (CMS)-issued Fiscal Year (FY) 2020 Medicare Part A proposed rules. Between April 17 and April 23, 2019, the CMS issued the proposed rules for general acute care hospitals paid under the Inpatient Prospective Payment System (IPPS), the skilled nursing facility (SNF) prospective payment system (PPS), the Inpatient Rehabilitation Facility (IRF) PPS, the Long-Term Care Hospital (LTCH) PPS, the Hospice PPS, and the Inpatient Psychiatric Facility (IPF) PPS. These proposed regulations include annual payment rate changes and other proposed policy changes. Comment deadlines for these rules vary.

Engagement with community-based organizations key to achieving health equity & wellness for Medicaid populations
A new issue brief from AcademyHealth, in partnership with Health Management Associates (HMA) and the Disability Policy Consortium (DPC), showcases the vital role that community-based organizations (CBOs) can play in advancing health equity and wellness for individuals and communities in Medicaid payment and care delivery system reform.
The brief provides five key lessons from CBOs in New York City and reactions to those lessons from CBOs in Massachusetts. Together, these perspectives provide a compelling case to elevate the role of CBOs in reform.
The authors, including HMA’s Ellen Breslin and Heidi Arthur, call for the development of a National Blueprint for Advancing Health Equity Through Community-Based Organizations to facilitate greater cross-sector collaboration between CBOs and HCOs.
Read the full brief here or on the AcademyHealth website.

HMA Conference to Feature Insights from 40+ Speakers, Including Health Plan CEOs, State Medicaid Directors, Providers
Pre-Conference Workshop: September 8, 2019
Conference: September 9-10, 2019
Location: Chicago Marriott Downtown Magnificent Mile
Health Management Associates is proud to announce its fourth annual conference on trends in publicly sponsored health care: The Next Wave of Medicaid Growth and Opportunity: How Payers, Providers, and States Are Positioning Themselves for Success.
The HMA conference has emerged as a premier informational and networking event, attracting more than 450 executives and policy experts. Speakers this year include state Medicaid directors and leaders from Medicaid managed care, hospitals, clinics, community-based organizations, and other providers.