An HMA-authored issue brief examines beneficiary access to, and plan adoption of, newly expanded Medicare Advantage (MA) supplemental benefit flexibilities and raises questions regarding the expected impacts of new supplemental benefit offerings on beneficiary satisfaction, outcomes, and total cost of care.
1247 Results found.

Webinar Replay: Tracking State Responses to COVID-19 for Home Health and Home Care Providers: Survey Results and Provider Perspectives
This webinar was held on June 9, 2020.
With most federal COVID-19 funding going to hospitals and nursing homes, states are implementing various Medicaid authorities, legislation, and policies of their own to improve access to long-term services and supports, including home and community-based services. HMA home care experts have tracked these state efforts and presented the results during this informational session. They were joined by home health and home care industry leaders, who offered important perspectives on state actions as well as thoughts on additional steps that will be necessary over the long term.
Learning Objectives:
- Understand state COVID-19 legislation, executive orders, and policy guidance and how it affects home health and home care providers.
- Gain perspective from home health and home care providers on how state COVID-19 efforts are playing out.
- Understand the immediate and long-term challenges and opportunities home health and home care providers are likely to face as they respond to COVID-19.
Speakers
Karen Brodsky, Principal, HMA
Pat Kelleher, Executive Director, Home Care Alliance of Massachusetts
Linda Mintz, Co-Chair, CareFinders Total Care
Susan Tucker, Principal, HMA

HMA Conference on Trends in Publicly Sponsored Healthcare
HMA Conference 2020
What’s Next for Medicaid, Medicare, and Publicly Sponsored Healthcare:
How Payers, Providers, and States Are Navigating a Future of Opportunity and Uncertainty
Pre-Conference Workshop: October 25
Conference: October 26-27
Location: Fairmont Chicago, Millennium Park

Medicare FY 2021 Hospital Inpatient Proposed Rule, Federal Flexibilities for COVID-19
This week, our In Focus section reviews recent announcements and actions by Congress and the Centers for Medicare & Medicaid Services (CMS) that have significant financial and operational implications for the hospital industry. This brief begins with the most recent of these actions by providing a summary of the key provisions of the CMS Fiscal Year (FY) 2021 Medicare Hospital Inpatient Prospective Payment System (IPPS) and Long-Term Acute Care Hospital (LTCH) Proposed Rule (CMS-1735-P), which includes Medicare payment updates and policy changes for the upcoming FY, with a comment deadline of July 10, 2020. Although somewhat limited in scope compared to previous proposals, this year’s proposed rule includes several disruptive proposals that the hospital industry should carefully consider.

HMA Updates Forecast of COVID-19 Impact on Medicaid, Marketplace, Uninsured
Health Management Associates’ (HMA) updated analysis projects the potential impact of the COVID-19 pandemic on health insurance coverage and cost by state through 2022. The analysis provides deeper insights into how health insurance coverage is estimated to take years to more closely resemble pre-COVID-19 coverage levels.

Medicaid Managed Care Spending in 2019
This week, our In Focus section reviews Medicaid managed care spending data collected in the annual CMS-64 Medicaid expenditure report. After submitting a Freedom of Information Act request to the Centers for Medicare & Medicaid Services (CMS), we have received a draft version of the CMS-64 report that is based on preliminary estimates of Medicaid spending by state for federal fiscal year (FFY) 2019. We expect the final version of the report will be completed by the end of 2020 and posted to the CMS website at that time. Based on the preliminary estimates, Medicaid expenditures on medical services across all 50 states and six territories in FFY 2019 exceeded $594 billion, with over half of all spending now flowing through Medicaid managed care programs. In addition, total Medicaid spending on administrative services was $29.5 billion, bringing total program expenditures to $623.5 billion.

Webinar Replay: Supporting the Behavioral Health Workforce During the COVID-19 Response: Strategies for Providers to Sustain and Strengthen the Behavioral Health System
This webinar was held on May 18, 2020.
Even as behavioral health providers work tirelessly to respond to COVID-19, the most forward-looking organizations also recognize that the pandemic has laid bare the need to develop a wide variety of short- and long-term solutions to ongoing and emergent needs. The most pressing of these needs concern strategies to support and strengthen the behavioral health system workforce.
During this webinar, HMA experts showed how leading behavioral health providers are using new regulatory flexibilities, emerging staffing models, and new delivery formats to develop and implement organizational changes and innovations that sustain workforce excellence.
Learning Objectives:
- Hear how behavioral health providers around the country are supporting their workforce and continuing to meet ongoing and emergent behavioral health needs.
- Learn how collaborative efforts among states and providers can lead to meaningful changes in rules, roles, tools, and approaches to delivering behavioral healthcare.
- Obtain cross-cutting strategies for management and leadership during a crisis.
- Find out how to ensure organizational structures are in place to help staff adjust to change, foster resilience, and provide bereavement support when appropriate.
- Understand the available resources and emerging practices for workforce support, including training, technology, and strategies for enhancing the ability of the behavioral health workforce to meet the needs of special populations.
HMA Speakers
Barry Jacobs, PsyD, Principal, Philadelphia, Pennsylvania
Gina Lasky, PsyD, Principal, Denver, Colorado
Shannon Mong, PsyD, Principal, San Francisco, California
Lori Raney, MD, Principal, Denver, Colorado
Meggan Schilkie, MBA, Managing Principal, New York
Tim Sheehan, MSW, Principal, Chicago, Illinois

HMA report examines COVID-19 toll on Pennsylvania hospitals
A report completed by HMA colleagues estimated the potential financial impact on hospitals and health systems of the current COVID-19 pandemic in the Commonwealth of Pennsylvania.
The analysis, completed in mid-April, concluded that Pennsylvania hospitals and health systems are likely to experience losses in excess of $7 billion for the final 10 months of 2020 after accounting for federal disaster relief payments, based on emergency relief legislation that had been passed at the time. HMA Principal Tom Marks and Senior Consultant Mary Goddeeris completed the report, Analysis of the Financial Impact of COVID-19 on Pennsylvania Hospitals, on behalf of the Hospital and Healthsystem Association of Pennsylvania (HAP). HMA conducted interviews and collected data from finance officials at a sample of health systems and projected the findings across the population of Pennsylvania hospitals and health systems. The interviews and analysis were completed in mid-April, well before the full effect of the pandemic could be measured. Financial leaders consistently reported enormous declines in patient service from mid-March to mid-April due to the cancellation and deferral of non-emergency services. While there are varying assumptions about the return of pre-pandemic patient service volumes, all leaders projected a bleak forecast for the second quarter and continued negative impact of service disruption for the rest of 2020.
Learn more about HMA’s multi-faceted COVID-19 response.

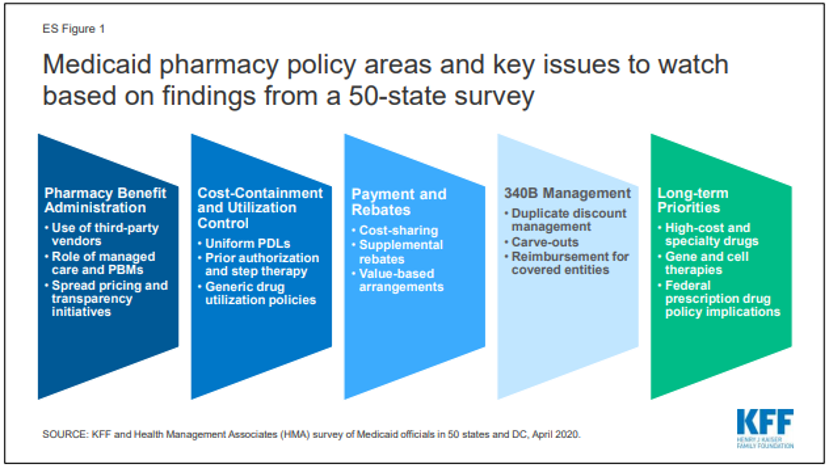
HMA experts publish 50-state Medicaid pharmacy study with Kaiser Family Foundation
In conjunction with the Kaiser Family Foundation (KFF), a team of HMA experts have published survey results and analysis examining administration of the Medicaid pharmacy benefit. HMA contributing colleagues were Kathleen Gifford, Anne Winter and Linda Wiant. Rachel Dolan, Marina Tian, and Rachel Garfield from KFF also contributed.
The report, How State Medicaid Programs are Managing Prescription Drug Costs: Results from a State Medicaid Pharmacy Survey for State Fiscal Years 2019 and 2020, summarized the survey conducted in all 50 states and the District of Columbia.
The survey outlines Medicaid pharmacy policy areas and key issues to watch based on feedback from the states in several categories including pharmacy benefit administration, cost-containment and utilization controls, payment and rebates, 340B management and long-term priorities.