On May 10, 2024, the Centers for Medicare & Medicaid Services (CMS) published the Medicaid and Children’s Health Insurance Program (CHIP) Managed Care Access, Finance, and Quality Final Rule (CMS-2439-F).
CMS created a fact sheet which concisely reviews the final rule’s key provisions, as well as an applicability dates chart, which serves as a reference guide to the various applicability dates for different provisions in the final rule. The final rule creates new flexibilities and requirements aimed at enhancing accountability for improving access and quality in Medicaid and CHIP by principally addressing these topic areas:
- ILOSs are defined as substitute services or settings for a service or setting covered under the state plan and can be leveraged by Managed Care Organizations (MCOs) to address unmet health-related social needs (HRSNs).
- They must be offered to all members and must be voluntary as well as documented in MCO contracts.
- ILOSs cannot exceed 5% of total capitation.
- If ILOS costs exceed 1.5% of total capitation, states must provide additional documentation to CMS to demonstrate medical appropriateness and cost-effectiveness.
- When an ILOS is terminated, states must develop a transition plan to arrange for state plan services and settings to be provided in a timely manner.
- States must make available online a “one-stop-shop” where members can learn about and compare MCOs based on quality and other variables.
- Mandatory quality measures are established.
- The methodology for calculating the quality ratings displayed on each state’s MAC QRS is also established.
- Although guidelines exist, states can submit their own version of a MAC QRS to CMS for approval.
- Provider incentive payments must be tied to clearly defined, objectively measurable, and well-documented clinical or quality improvement standards to be classified as incurred claims (in alignment with private market MLR regulations).
- Prohibits the inclusion of indirect administrative costs that are not directly related to improving quality as QIAs as incurred claims in the numerator (in alignment with private market MLR regulations).
- Imposes additional expense allocation methodology requirements (in alignment with private market MLR regulations).
- Requires SDPs to be included as both incurred claims (for payments made by MCOs to providers) and premium revenue (for payments made by states to MCOs).
- Sets maximum appointment wait time standards of no more than 15 business days for routine primary care (adult and pediatric) and obstetric/gynecological services and 10 business days for mental health and substance use disorder services (adult and pediatric).
- Enforces these standards using secret shopper surveys and requires states to contract for the secret shopper surveys.
- Requires states to post the appointment wait time standards as well secret shopper survey results.
- A remedy plan must be implemented for any MCO that fails to meet these required standards for access.
- States must also conduct an annual enrollee experience survey for each MCO.
- Codifies ACR payment ceiling, which applies to hospitals, practitioner services at academic medical, and nursing facility services.
- Requires “hold harmless” attestation.
- Allows for SDPs at 100% of Medicare without prior written approval.
- Removes network provider requirement to receive payment.
- Prohibits use of interim payments based on prior period data even if ultimately reconciled.
- Prohibits use of separate payment term where SDPs are paid separate from capitation rates.
- Explicitly states that SDPs must result in “stated goals and objectives.”
- Requires states to submit detailed, provider level SDP data to the Transformed Medicaid Statistical Information System.
Implications for States
The final rule creates opportunities for states to leverage new flexibilities to further policy goals but also creates new administrative burdens. MCOs and providers will look to states to comprehensively understand final rule’s requirements and be prepared to manage the steps necessary to achieve compliance over a multiyear implementation process.
Implications for MCOs
As states move to comply with the final rule, MCOs will be immediately downstream from the steps taken by states to do so and MCOs need to prepare accordingly. Proactive actions by MCOs to not only engage with states early but also to prepare financially and operationally for the different provisions of the final rule over time will put them in the best position possible.
Implications for Providers
The most significant implications for providers in the final rule are related to SDPs, where a new level of accountability will be required. All topics covered by the final rule, however, have provider implications.
Looking ahead
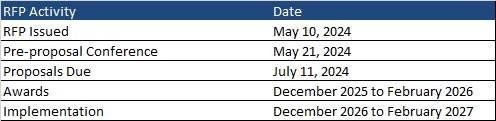
The provisions of the final rule range in their effective dates from as early as the final rule’s effective date, July 9, 2024, to as late as the first rating period on or after four years after July 9, 2024.
Because of these variable effective dates, states, MCOs, and providers will need to comply with the final rule immediately in some cases, while having significant lead time to do so in other areas. Sub regulatory guidance is also forthcoming and must be monitored for and digested.
HMA stands ready to support states, MCOs, and providers in analyzing and responding to the strategic, financial, and operational impacts of the final rule’s provisions in specific markets and organizational contexts.
If you have questions or want to connect with our expert team members, e-mail [email protected].