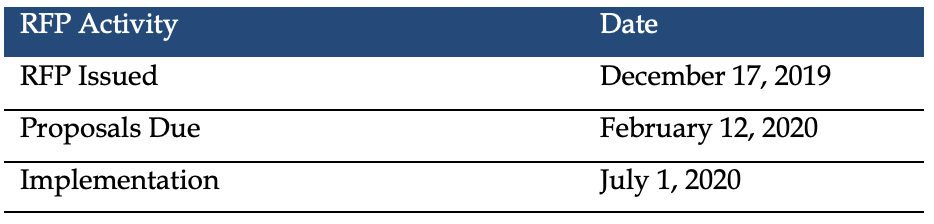
This week, our In Focus section reviews the West Virginia Mountain Health Trust request for proposals (RFP) released by the West Virginia Department of Administration (DOA) for the Department for Health and Human Resources (DHHR) on December 17, 2019. Mountain Health Trust (MHT) is the statewide physical and behavioral Medicaid managed care program. West Virginia will award contracts, worth over $1.5 billion, to three managed care organizations (MCOs), with implementation beginning July 1, 2020.
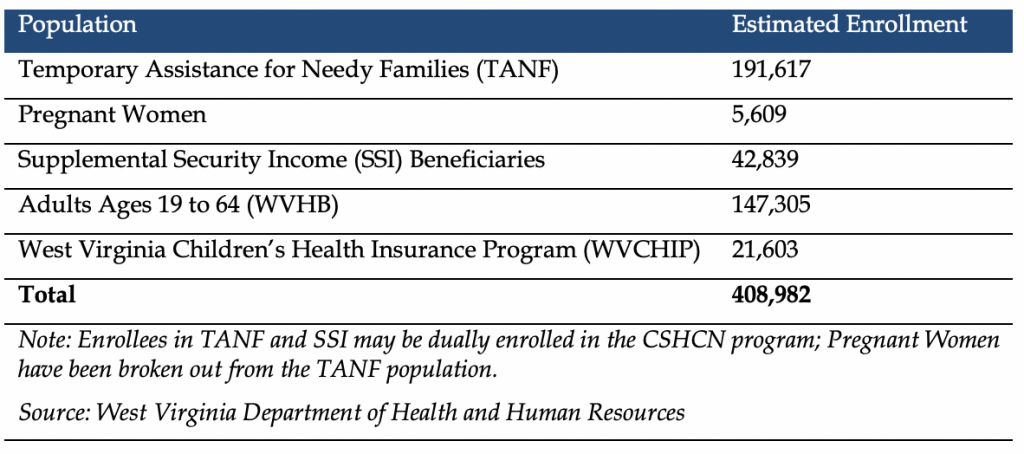
Mountain Health Trust serves most Medicaid eligibility groups, including TANF, pregnant women, Children with Special Health Care Needs (CSHCN), and SSI; the West Virginia Health Bridge Medicaid expansion population; and beginning July 1, 2020, the West Virginia Children’s Health Insurance Program (WVCHIP). WVCHIP is currently fee-for-service and will add approximately $45 million to the contracts. MHT is projected to have 408,982 total enrollees for the fiscal 2021 contract term.
Fiscal 2021 Managed Care Estimated Member Enrollment
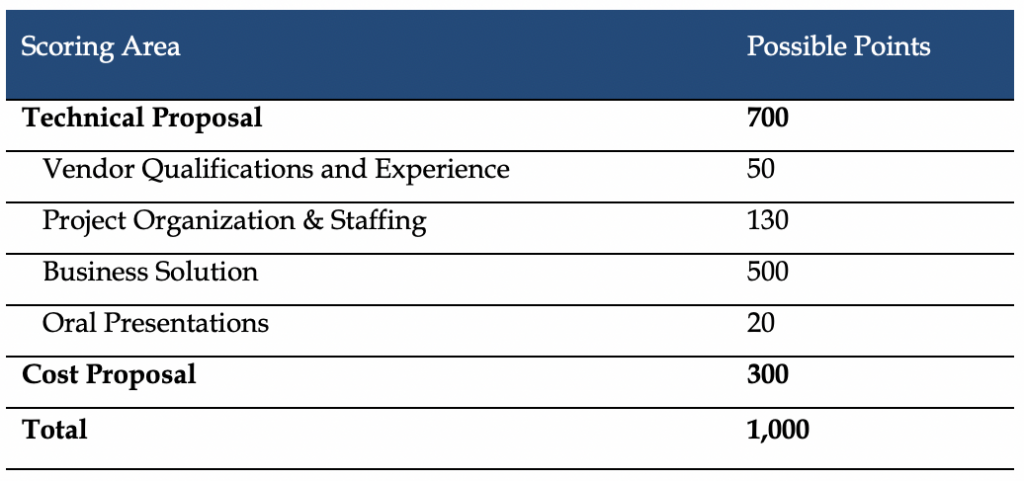
Evaluation
Proposals will be evaluated out of a total 1,000 points – 700 for the technical proposal and 300 for the cost proposal. The three plans with the highest number of points will be awarded contracts. Plans will need to score a minimum of 70 percent or 490 points in the technical proposal to move on and have the cost proposal evaluated. To determine the cost score, the state will divide the lowest cost of all proposals by the cost of the proposal being evaluated. This percentage will then be multiplied by the total 300 points.
Timeline
Proposals are due February 12, 2020. The contracts are for one year beginning July 1, 2020, with three optional, one-year renewals. A date to award the three winning plans is still to be determined.
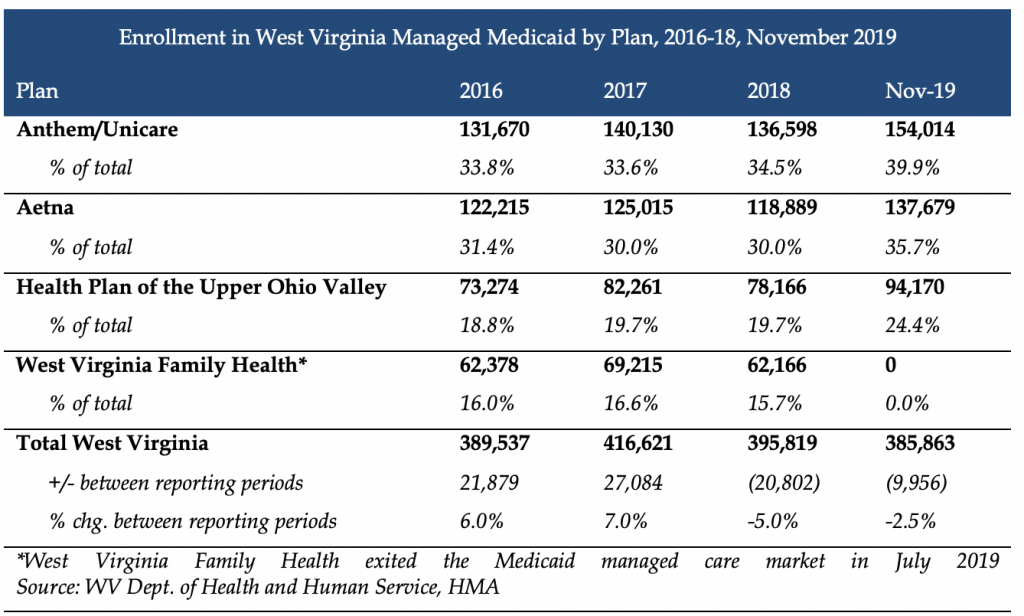
Current Market
Incumbent health plans are Anthem, Aetna, and the Health Plan of the Upper Ohio Valley, serving nearly 386,000 individuals.