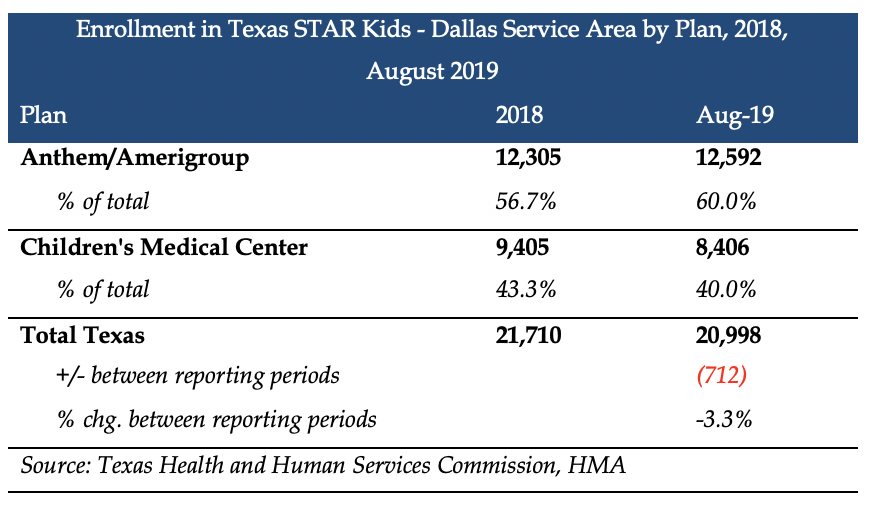
This week, our In Focus section reviews the Texas STAR Kids Medicaid Managed Care in the Dallas Service Area (SA) request for proposals (RFP) released by the Texas Health and Human Services Commission (HHSC) on December 13, 2019. The RFP comes after Children’s Medical Center, which covers approximately 9,000 members under the program, said it would be leaving the market. The contracts for the SA are worth approximately $500 million. Anthem/Amerigroup will remain in the Dallas SA and continue to provide services. STAR Kids provides Medicaid coverage to individuals with disabilities under age 21.
Evaluation
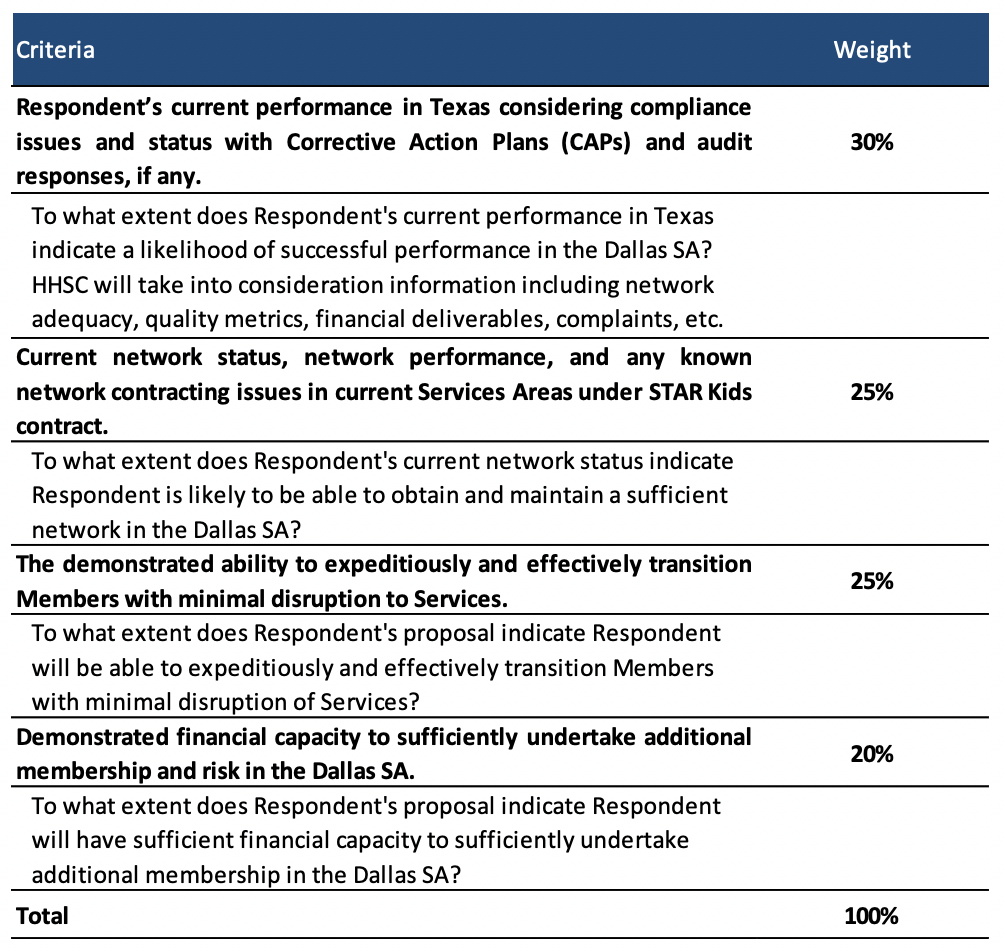
In order to qualify, MCOs will need to have a current STAR Kids contract in any SA. Eligible plans include Aetna, Blue Cross Blue Shield of Texas, Centene/Superior, Community First, Cook Children’s Health Plan, Driscoll, Texas Children’s Health Plan, and United. Proposals will be scored based on the following criteria found in the table below.
Timeline
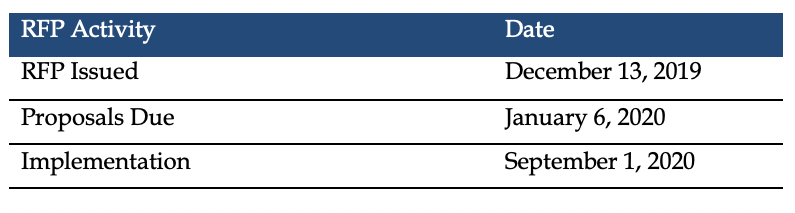
Implementation begins September 1, 2020, with contracts running through August 31, 2022. HHSC can extend the contracts for up to two additional years. The original implementation date was scheduled for March 1, 2020.
Enrollment
In August 2019, there were approximately 21,000 STAR Kids members in the Dallas SA. Statewide, STAR Kids has 158,000 members.
Texas STAR Kids – Dallas Service Area RFP Link