This week, our In Focus sections reviews the Missouri HealthNet Pharmacy and Clinical Services Management Solution request for information (RFI) and the Kentucky Medicaid Managed Care Organization (MCO) Pharmacy Benefit Manager request for proposals (RFP).
Missouri RFI
On August 28, 2020, the Missouri Department of Social Services, HealthNet Division (MHD) released an RFI seeking information for a possible procurement of a Pharmacy and Clinical Services Management Solution for MO HealthNet, the state’s Medicaid program. HealthNet uses both managed care and fee-for-service (FFS) delivery models, with two-thirds of the population in managed care. However, pharmacy services are carved out entirely to FFS, so 85 percent of all Rx transactions will be FFS. The vendor will need to serve the needs of Medicaid enrolless in both FFS and managed care. HealthNet currently serves nearly 876,000 individuals, with over 313,000 claims processed daily, 99 percent of which are submitted electronically. Missouri HealthNet expenditures total $7.9 billion annually.
Missouri currently contracts with Conduent for the maintenance, operation, and development of the Clinical Management and System for Pharmacy Claims and Prior Authorization (CMSP) in addition to a clinical data mart for CMSP Ad Hoc Reporting. The current Missouri Medicaid Management Information Systems (MMIS) Fiscal Agent (FA) is Wipro Infocrossing, Inc., which is responsible for the development, operation, and maintenance of the primary MMIS, the Decision Support System (DSS), and reporting solutions such as Ad Hoc Reporting and Management and Administrative Reporting Subsystem (MARS). Both contracts expire on September 30, 2021.
The Pharmacy and Clinical Services Management Solution, part of the Medicaid Enterprise Systems (MES), will support the administration of the HealthNet program by helping manage the Missouri Medicaid Enterprise (MME) programs, provide services to program participants, and support the Medicaid healthcare service providers. Examples of services that this solution would provide include:
- Increased automation of Medicaid business processes
- Systems to reduce development time for functionality and business process modifications required to support Medicaid program changes
- Continuation of pharmacy and clinical services, including operation of call centers; development, operation, and support of the Pharmacy and Clinical Services Management System; hosting services; privacy and security management services; professional review services to support prior authorization of participant services; data entry; and project management services
- Support multiple payers and benefit packages designed for multiple individual eligibility groups
- Meeting the needs of the MME for the next decade with a modern, scalable, configurable, and customizable technical architecture
- A robust provider web portal, web services, and network connection options that allow Medicaid healthcare service providers to submit and manage pharmaceutical claims and service authorization requests and access necessary participant and provider information in an automated fashion
- Support for case management and coordination of care business functions within the MME
- Support for administration of the Home and Community-Based Services program including management of level of care assessments
Following the RFI, Missouri may choose the vendors to demonstrate their solutions. The proposed demonstrations are scheduled for November 2020.
The state is also working towards replacing the existing MMIS modules including the core claims processing system. Thus far, the state has committed to:
- Procuring an Enrollment Broker and Premium Collections solution and services. RFP responses are currently being evaluated
- Participating in a National Association of State Procurement Officers (NASPO) project to develop a master agreement for Third Party Liability (TPL) services
- Participating in a NASPO project to develop a master agreement for a core MMIS claims processing and financial solution; RFP responses are currently being evaluated.
- Procuring Health Information Network (HIN) services; RFP responses are currently being evaluated.
- Implementing a Program Integrity Solution to replace the existing Fraud and Abuse Detection System (FADS) and Surveillance and Utilization Review System (SURS) and to add a Program Integrity case management system
- Implementing a Business Intelligence Solution – Enterprise Data Warehouse (BIS-EDW) to replace the existing MMIS data warehouse and data analytics tools
- Evaluating options for purchase of a Provider Enrollment Solution
- Conducting extensive information gathering sessions to document business requirements related to key Medicaid business functions including claims processing, prior authorization, financial management and reporting, and drug rebate
Kentucky RFP
The Kentucky Cabinet for Health and Family Services (CHFS) Department for Medicaid Services (DMS) released its MCO Pharmacy Benefit Manager (PBM) RFP on August 14, 2020. Proposals are due October 6, 2020. DMS will award a single vendor to serve as the PBM for the entire Medicaid Managed Care Program. The award and contract date for a single, statewide MCO PBM will occur no later than December 31, 2020, with a planned operational, go-live date no later than July 1, 2021. The vendor will contract with each Medicaid MCO separately and receive pharmacy reimbursement directly from the MCOs. In return, the PBM will:
- Process claims and administer payments to Kentucky Medicaid pharmacy providers
- Apply the Kentucky Medicaid preferred drug list (PDL) and benefit design
- Adjudicate prior authorization (PA) requests using DMS-established criteria
- Adjudicate first level PA appeals
- Conduct Retrospective Drug Utilization Review (RetroDUR) activities
- Provide Kentucky Medicaid pharmacy Provider and Beneficiary customer service
- Perform pharmacy network auditing
- Prepare and submit reports to DMS and contracted MCOs
- Provide DMS and MCOs with real-time unredacted access to the contractor’s claims processing and online reporting systems
Magellan Rx Management currently holds the contract for FFS PBM, with options through December 31, 2021. It will continue to process FFS pharmacy claims, unrelated to this procurement.
Kentucky’s Medicaid and CHIP programs serve a total of 1.4 million beneficiaries, with 120,000 Aged, Blind or Disabled (ABD) and Long Term Care (LTC) members in FFS. The remaining 1.3 million members are served by Aetna, Anthem, Centene/WellCare, Humana, and Passport. New contracts were awarded in May 2020 to Aetna, Centene/WellCare, Humana, Molina, and UnitedHealthcare, which will be effective January 1, 2021, prior to the go-live date of the single MCO PBM. MCO pharmacy services are currently provided by the health plans and DMS.
In 2019, a total of 55.6 million Rx claims were paid by the five MCOs, with nearly 4,700 pharmacies enrolled with DMS.
Evaluation
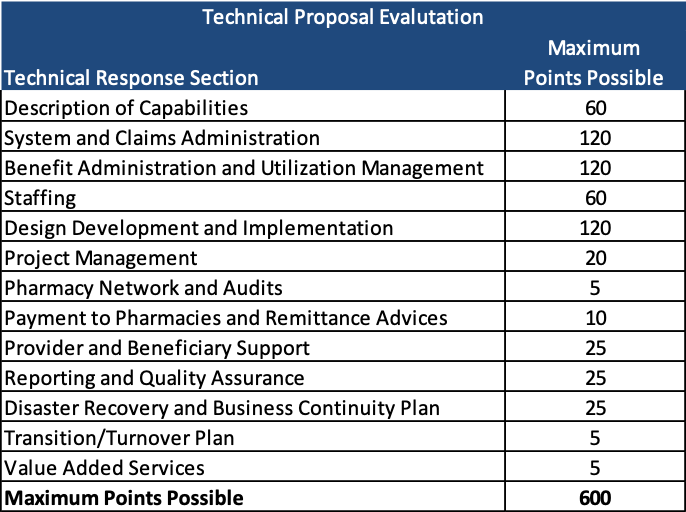
The proposals will be scored on a maximum total of 1,000 points.
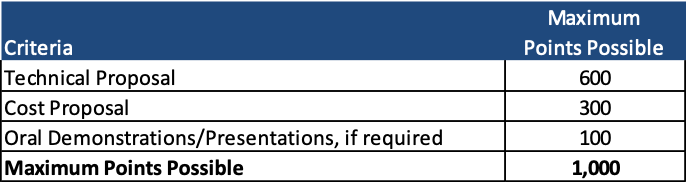
Any proposals that scoreless than 360 points on the technical evaluation will not be considered.
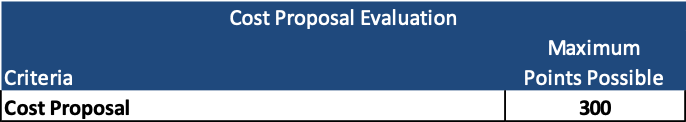
The bidder with the lowest total cost will receive 300 points for the cost proposal.
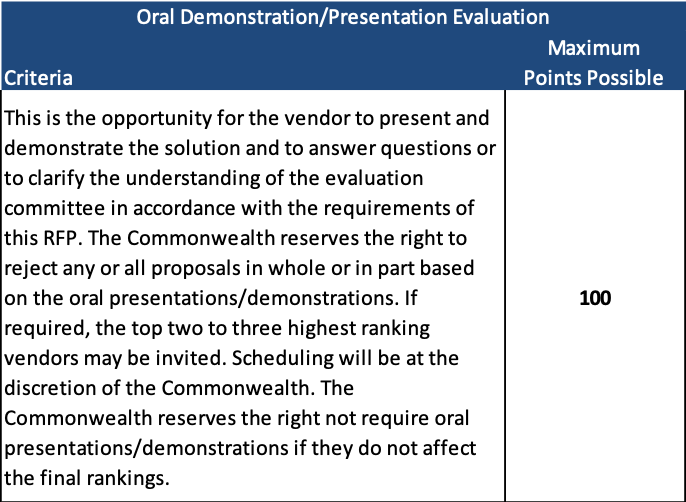
Oral demonstrations/presentations, if required by the state, are worth 100 points.