This week, our In Focus section reviews the Iowa Health Link request for proposals (RFP) for Medicaid managed care organizations (MCOs) to serve the state’s traditional Medicaid program, the Children’s Health Insurance Program (CHIP) known as Healthy and Well Kids in Iowa (Hawki), and the Iowa Health and Wellness Plan (IHAWP). The RFP was released by the Iowa Department of Human Services on February 17, 2022. Contracts are set to begin July 1, 2023, and are worth approximately $6.5 billion annually.
Iowa Health Link Background
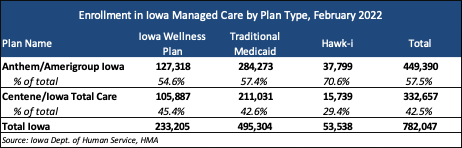
The Iowa Medicaid managed care program, called Health Link, began in April 2016. AmeriHealth Caritas, Anthem, and UnitedHealthcare were awarded the original contracts. All three experienced heavy financial loses, leading to AmeriHealth Caritas exiting the program in 2017 and UnitedHealthcare exiting in 2019. Centene/Iowa Total Care joined the program in 2019. As of February 2022, Anthem and Centene serve approximately 782,000 enrollees. Approximately 93 percent of all Iowa Medicaid members are enrolled in an MCO, with 7 percent remaining in fee-for-service (FFS).
In September 2021, Ohio-based CareSource confirmed its intent to bid on the RFP. Iowa is expected to procure between one and four contracts. The final number of awarded contracts under the procurement will be up to the discretion of the state.
RFP
MCOs will provide statewide integrated care, including physical health, behavioral health, long-term support services (LTSS), and pharmacy services. New contracts will run for four years with one possible two-year extension.
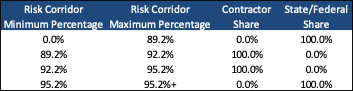
The MCOs will have a target medical loss ratio (MLR) of 88 percent. If the MLR is below, the MCO will need to refund the state. The risk sharing corridor is as follows:
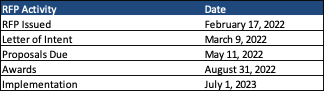
Timeline
Letters of intent are due by March 9, 2022, with proposals due by May 11. Awards are expected August 31. Implementation will begin July 1, 2023.