This week, our In Focus section reviews the Hawaii Quest Integration (QI) Medicaid managed care request for proposals (RFP) released on December 8, 2020, and the Minnesota Families and Children Medical Assistance (MA) and MinnesotaCare programs RFP released on January 4, 2021.
Hawaii QI RFP
The Hawaii Department of Human Services (DHS) intends to contract with up to five health plans to provide integrated medical, behavioral, and long-term services and supports (LTSS) to more than 378,000 Medicaid and Children’s Health Insurance Program (CHIP) members. DHS prefers that plans serve statewide, but plans may propose to serve one or more islands. Each island will need at least two plans. Contracts are estimated to be worth approximately $2.5 billion annually.
Hawaii previously awarded contracts to UnitedHealthcare, Centene/WellCare, AlohaCare (in partnership with Kaiser), and Hawaii Medical Service Association (HMSA) on January 22, 2020; however, those contracts were rescinded because of the COVID-19 pandemic. Contracts with incumbent plans AlohaCare, HMSA, Kaiser, Centene/WellCare, and UnitedHealthcare were extended. Read the write-up on the previous RFP.
The QUEST program, which stands for Quality care, Universal access, Efficient utilization, Stabilizing costs, and Transforming the way health care is provided to QUEST members, first began in 1994. In 2009, the aged, blind, and disabled (ABD) population was transitioned to a managed care program called QUEST Expanded Access (QExA) and in January 2015, integrated into the program now known as Quest Integration. Medicaid covered populations include children; former foster care children; pregnant women; parents/caretakers; individuals receiving transition medical assistance; ABD; non-citizens/refugees; and individuals with breast or cervical cancer.
Similar to the previous RFP, the new procurement will include the Hawaii `Ohana Nui Project Expansion (HOPE) Program, which focuses on health and wellness through four strategic areas:
- Investing in primary care, prevention, and health promotion
- Improving outcomes for individuals with special healthcare needs (SHCN)
- Reforming and aligning payment to providers
- Supporting community-driven initiatives to improve population health
Plans will also need to have a Dual-Eligible Special Needs Plan (D-SNP) for Medicare and Medicaid members in Hawaii no later than January 1, 2022, or provide DHS a quarterly report detailing progress made toward D-SNP approval in 2021 with the Centers for Medicare & Medicaid Services (CMS).
By no later than the end of the third contract year, DHS also intends to establish a specialized health pilot concept called the Hale Ola, an advanced health home for Expanded Health Care Needs (EHCN) members, which are members with complex, costly health care needs. Pilots will be established in at least three regions. Plans will be accountable for ensuring care is provided through the Hale Ola.
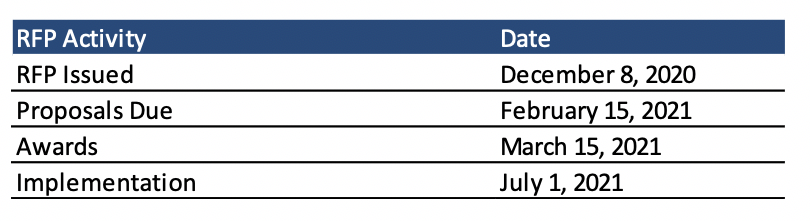
RFP Timeline
Proposals are due February 15, 2021, and awards will be made on March 15, 2021. Implementation is slated to begin July 1, 2021, with contracts running to December 31, 2026, with three additional optional years.
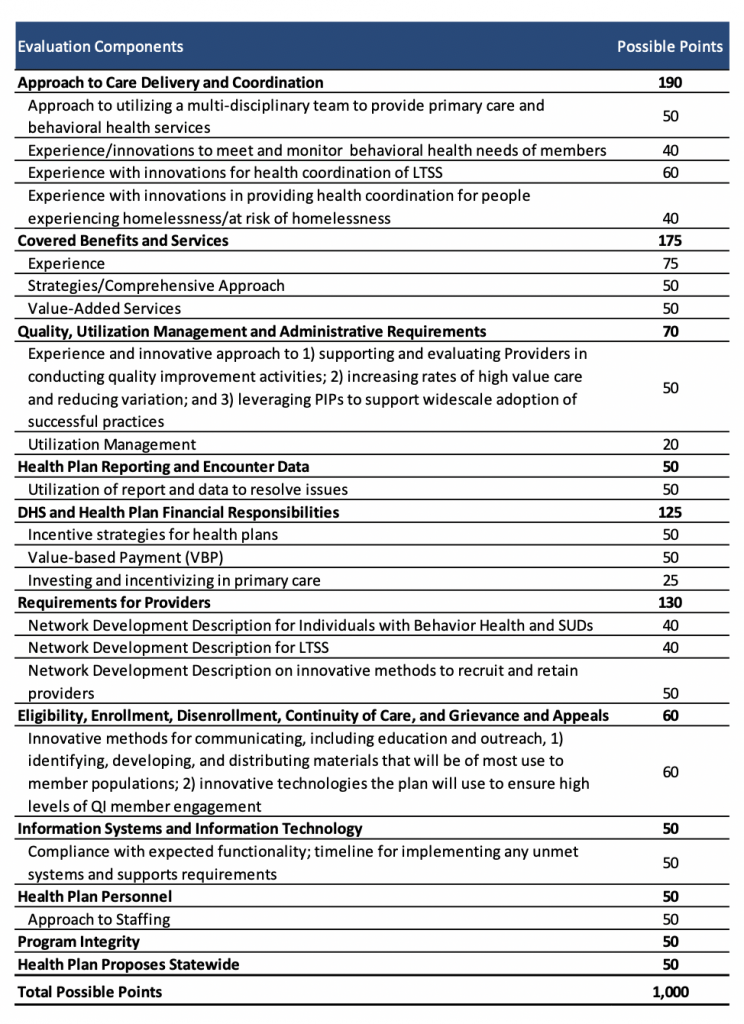
Evaluation
Health plans’ technical proposals will be scored out of a possible 1,000 points. DHS will then score plan proposals using rating methodology (ranging from 0 poor to 5 excellent) on how the proposal addresses the criteria and understanding of the subject matter. At a minimum, plans must receive a rating score of three and a minimum score of 750.
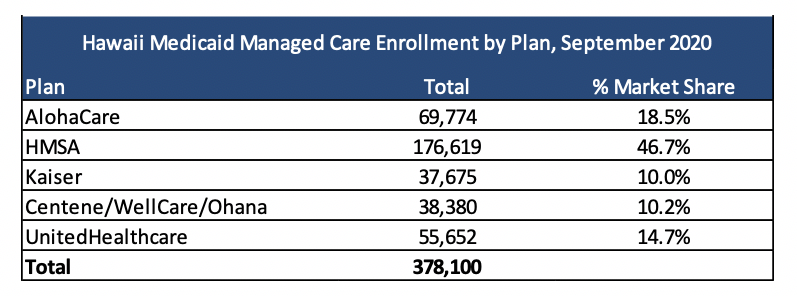
Current Market
As of September 2020, AlohaCare, HMSA, Kaiser, Centene, and United served 378,100 Quest Integration lives.
Minnesota MA and MinnesotaCare RFP
In September 2019, the Minnesota Department of Human Services (DHS) cancelled a procurement for MA, the state’s Medicaid managed care program, and MinnesotaCare, the Basic Health Program (BHP) across 80 greater Minnesota counties and renewed current contracts. The MA program provides Medicaid services for low income individuals, while MinnesotaCare provides health care services to individuals at 138 percent to 200 percent of the federal poverty level, funded by a provider tax, BHP funding, and enrollee premiums/cost sharing. The state explained that a court decision on the procurement “made it impossible to complete contracts in time to avoid disruption for enrollees and to meet timelines required by law.” For a write-up on the previous RFP, please click here.
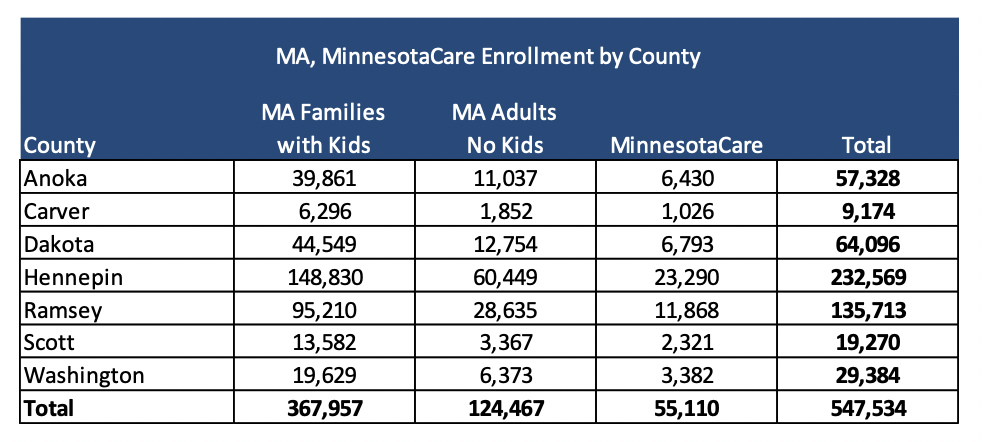
The new RFP, released this year, will only be for seven counties: Anoka, Carver, Dakota, Hennepin, Ramsey, Scott, and Washington, which are all metro areas. Medicaid managed care organizations must respond for all counties. The state will award contracts, worth over $3 billion annually, to at least two MCOs in each county for MA and MinnesotaCare.
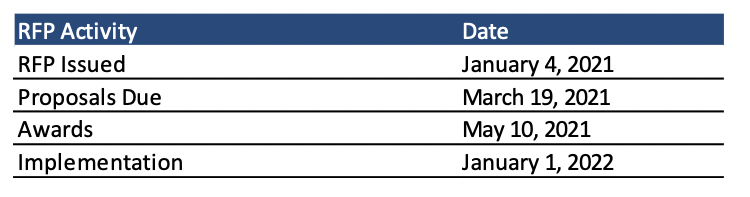
RFP Timeline
Contracts will run for one year beginning January 1, 2022, with five option years. Proposals for the RFP are due March 19, 2021, with awards expected to be announced on May 10, 2021.
Evaluation
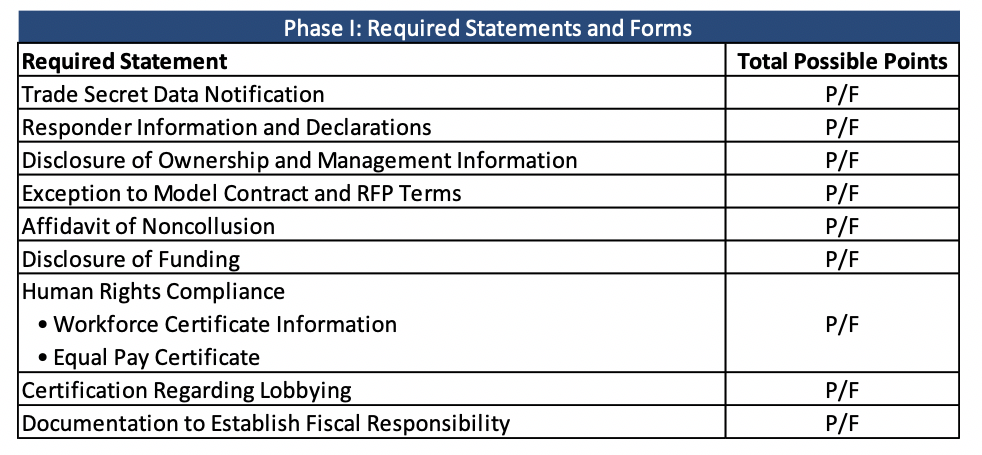
The RFP evaluation will consist of three phases:
- Phase I Required Statements Review
- Phase II Evaluation of Proposal Requirements and Readiness Review
- Phase III Selection of the Successful Responders
In Phase I, required statements will be scored on a pass/fail basis.
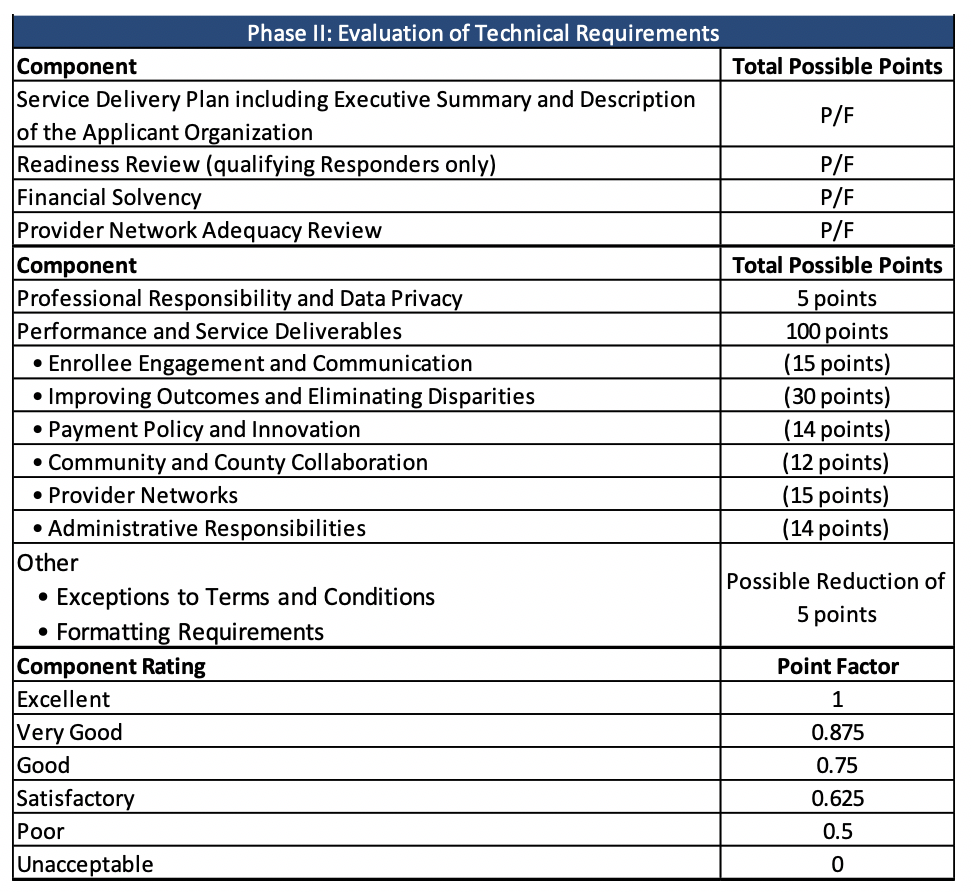
In Phase II, technical requirements will be evaluated on both a pass/fail basis and point factors. The evaluation team will then rate the performance and service deliverables on a scale.
Current Market
Seven plans, Blue Plus/BCBS of Minnesota, Health Partners, Itasca, Metropolitan/Hennepin Health, PrimeWest Health, South Country Health Alliance, and UCare Minnesota serve approximately 971,000 MA Children and Families and MinnesotaCare members across the state, as of December 2020. Medica has Medicaid lives in the Minnesota Senior Care Plus (MSC+)/Minnesota Senior Health Options (MSHO) programs in the state but not in the two programs relevant to this RFP.
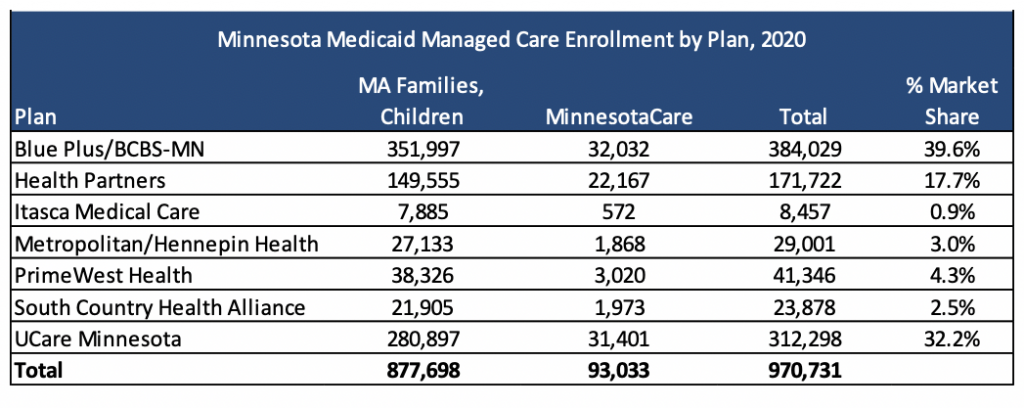
Currently, in the seven counties eligible for this RFP, there are nearly 550,000 MA and MinnesotaCare lives: