This week our In Focus section summarizes the United States Government Accountability Office (GAO) Medicaid report, State Views on Program Administration Challenges, released earlier this year. GAO conducted interviews with Medicaid officials from 50 states and the District of Columbia to identify challenges related to federal Medicaid policies.
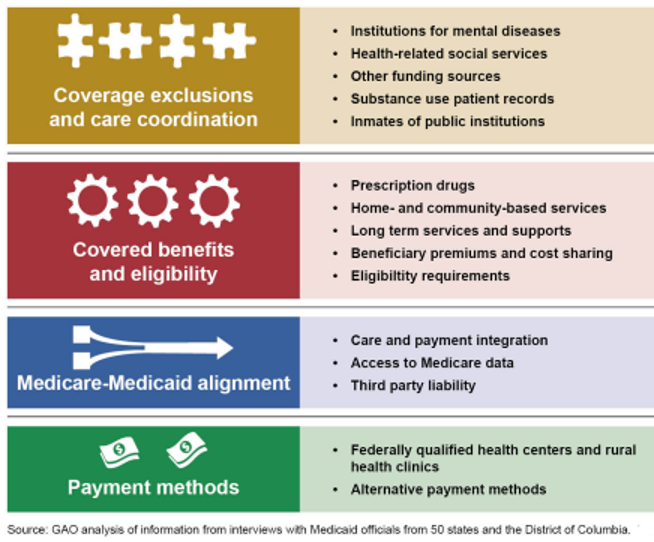
The areas posing the most challenges were coverage exclusions and care coordination; covered benefits and eligibility; Medicare-Medicaid alignment; and payment methods. HMA acknowledges that since the report was published on April 30, 2020, it does not reflect current COVID-19 policies.
Figure 1: Key Medicaid Program Areas Identified by State Medicaid Officials as Posing Challenges for Effective Program Administration
Coverage Exclusions and Care Coordination
Nearly all states found that federal policies related to coverage exclusions and care coordination are one of the most challenging barriers to providing a full continuum of care to beneficiaries with complex health care needs. Medicaid officials identified policies that exclude coverage for institutions for mental disease (IMDs); policies that exclude coverage for health-related social services, particularly housing; and policies that limit sharing medical records for patients with substance-use disorder (SUD).
Although states are able to apply for Medicaid waivers, for example a section 1115 waiver to cover services such as SUD treatment in IMDs, officials noted the administrative burden and concerns over limits on days of coverage. Specifically, officials cited the length and burden of the review process, level of guidance available, lack of permanency, and duration of approval period as challenges to the waiver review processes.
Other policies that officials found challenging include the inability to use Medicaid funds for other federal assistance programs (e.g. Supplemental Nutrition Assistance Program (SNAP)) or to provide Medicaid coverage for inmates, particularly high-risk inmates in short-term incarceration who may need SUD treatment.
Covered Benefits and Eligibility
While states noted the importance of access to prescription drugs, coverage requirements posed fiscal challenges. Under federal policy, states must cover all outpatient prescription drugs approved by the Food and Drug Administration (FDA) that are offered by manufacturers participating in the Medicaid Drug Rebate Program. However, newer drugs are often higher cost and certain higher cost drugs may not yet have an established clinical benefit or have an available lower cost alternative. States also cited other challenges, including not being able to impose premiums and cost sharing requirements that exceed five percent of a family’s monthly or quarterly household income and not being able to impose enrollment caps for home and community-bases services (HCBS) under state plan authority.
Medicare and Medicaid Alignment
In regard to Medicaid and Medicare alignment, officials stated that program differences limit integration efforts. States are unable to mandatorily enroll Medicaid beneficiaries in Medicare managed care plans and payment integration is complicated due to differences in covered services. Instead, officials said the Centers for Medicare & Medicaid Services (CMS) should create a new single program to serve dual-eligible beneficiaries and continue initiatives in this area. Officials also suggested that CMS provide further guidance on how Medicare data can be used and allow Medicaid managed care plans to access Medicare data. Additionally, since Medicare must pay for covered services for dual eligibiles before Medicaid, officials cited the burden of identifying Medicare contacts to address issues that arise and potential delays in beneficiaries’ access to services.
Payment Methods
Finally states identified challenges with payment methods, including a federal law that generally requires states to pay federally qualified health centers (FQHC) and rural health clinics (RHC) on the basis of a prospective payment system, where each facility is paid a rate based on its historical costs. Officials also cited delayed guidance or lack of clarity over how they can use alternative payment methods for certain services, such as long-term services and supports (LTSS) and prescription drugs.
CMS Actions to Address Policy Challenges
CMS is working to mitigate challenges for states. In the last few years, CMS has released guidance describing opportunities for states to improve integration across Medicare and Medicaid programs; describing opportunities to cover Medicaid services for residents of IMDs through section 1115 waivers; and provided technical assistance to states regarding housing services that can be covered under waivers and demonstrations. CMS has also streamlined the waiver process, reducing processing times, approving longer extensions, and clarifying guidance. Additionally, the agency is developing an updated reporting system that includes efforts to modernize state expenditure reporting on the form CMS-64.