This week, our In Focus section reviews a new model – Geographic Direct Contracting – introduced by the Centers for Medicare & Medicaid Services (CMS) Innovation Center. The model will test whether a geographic-based approach to care delivery and value-based care can improve health and reduce costs for Medicare beneficiaries enrolled in the traditional fee-for-service program across an entire region. This model represents one of the most transformational models released by the Innovation Center. During the 6-year Geographic Direct Contracting model performance period the traditional Medicare program will be replaced by the Direct Contracting program in the 10 selected regions.
Applications are due by April 2, 2021. CMS expects to announce participants by June 30, 2021, with the first performance year planned to begin January 1, 2022. However, it is possible the Biden Administration may opt to modify aspects of the Geographic Direct Contracting demonstration, potentially delaying any of these dates and modifying model characteristics. Interested participants will need to closely monitor CMS updates for potential revisions.
The Geographic Direct Contracting model joins similar models that were introduced earlier: standard, new entrant, high-needs, and Medicaid managed care organization-based (MCO) Direct Contracting. (The request for applications for the next performance year for these models is expected soon.) The new model will build on and continue testing potential reforms to the Medicare program encompassed by accountable care organizations (ACOs), the Medicare Shared Savings Program (MSSP), Medicare Advantage (MA), Medicaid managed care, and private sector risk-sharing arrangements.
Geographic Direct Contracting has the potential to transform how the traditional Medicare program interacts with providers and delivers care to beneficiaries. However, there will be substantial financial risk—and reward—for participants based on a new, complex payment methodology, so organizations interested in this new model should carefully consider the potential impact of participating in Geographic Direct Contracting versus other options.
Geo DCE Regions
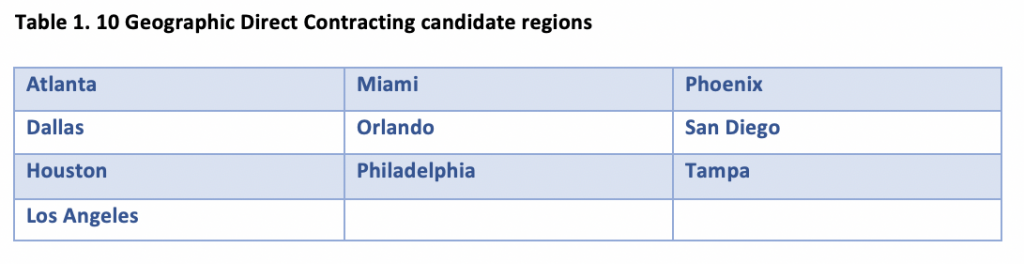
As CMS has currently outlined, Geographic Direct Contracting Entities (Geo DCEs) will take responsibility for the total cost of care for Medicare Fee for Service (FFS) beneficiaries in a specific region. Regions will be delineated by the central and outlying counties that comprise ten candidate cities, each of which contains between approximately 150,000 to 700,00 beneficiaries (Table 1). CMS expects the number of Geo DCEs per region to be between three and seven depending on the number of organizations that apply and the number of Medicare FFS beneficiaries in a region. This means that unlike the MA program where all qualified applicants are approved, the selection of DCEs will depend on their proposed approaches for implementing the model and their financial bids as CMS may select fewer participants than the number of organizations that apply.
Requirements for Participation
CMS anticipates interest from organizations that have significant experience taking risk in value-based care models, including sophisticated ACOs, health systems, health care provider groups, and health plans. CMS also anticipates some applications might include innovative partnerships between health plans and health care providers.
CMS’s specific requirements are that the Geo DCE must:
- be a legal entity identified by a federal taxpayer identification number (TIN) formed under applicable state, federal, or tribal law, and authorized to conduct business in each state in which it operates,
- have an identifiable governing body with the ultimate authority to execute the functions of the Geo DCE and to make final decisions on behalf of the Geo DCE,
- enter into an Organized Health Care Arrangement (OHCA), as the term is defined under the HIPAA Privacy Rule, with CMS, which includes detailed requirements, such as the Geo DCE must be a Covered Entity and use of protected health information (PHI),
- assume responsibility for receiving shared savings and paying shared losses to CMS,
- be capable of administering payments to “Geo Preferred Providers” and other providers, and
- maintain a 10 percent financial guarantee to repay any shared losses.
Beneficiary Attribution
Each Geo DCE will be attributed a minimum of 30,000 beneficiaries. Eligible beneficiaries must be enrolled in both Medicare Part A and Part B, have Medicare as a primary payer, and not be enrolled in a MA plan, cost plan, PACE organization, or other Medicare managed care plan. Beneficiaries may be attributed to Geo DCEs in multiple ways, including voluntary sign-up, claims-based assignment based on the plurality of primary care services received from the Geo DCE’s Geo Preferred Providers, and concurrent enrollment in an MCO operated by a DCE or its affiliates for full-benefit dually-eligible beneficiaries. Beneficiaries will have the right to voluntarily choose to align to a different DCE. All eligible beneficiaries residing in the ten regions will be attributed to a Geo DCE. Any beneficiaries not attributed through another method will be randomly attributed by CMS to a Geo DCE.
Geo DCEs’ Responsibilities and Payment
Medicare beneficiaries will maintain their rights to see any willing Medicare participating provider. However, DCEs will be permitted to provide incentives and care management support to encourage beneficiaries to seek care by DCE’s preferred providers. CMS has also stated that DCE’s will be able to apply utilization management tools, commonly applied in the MA program.
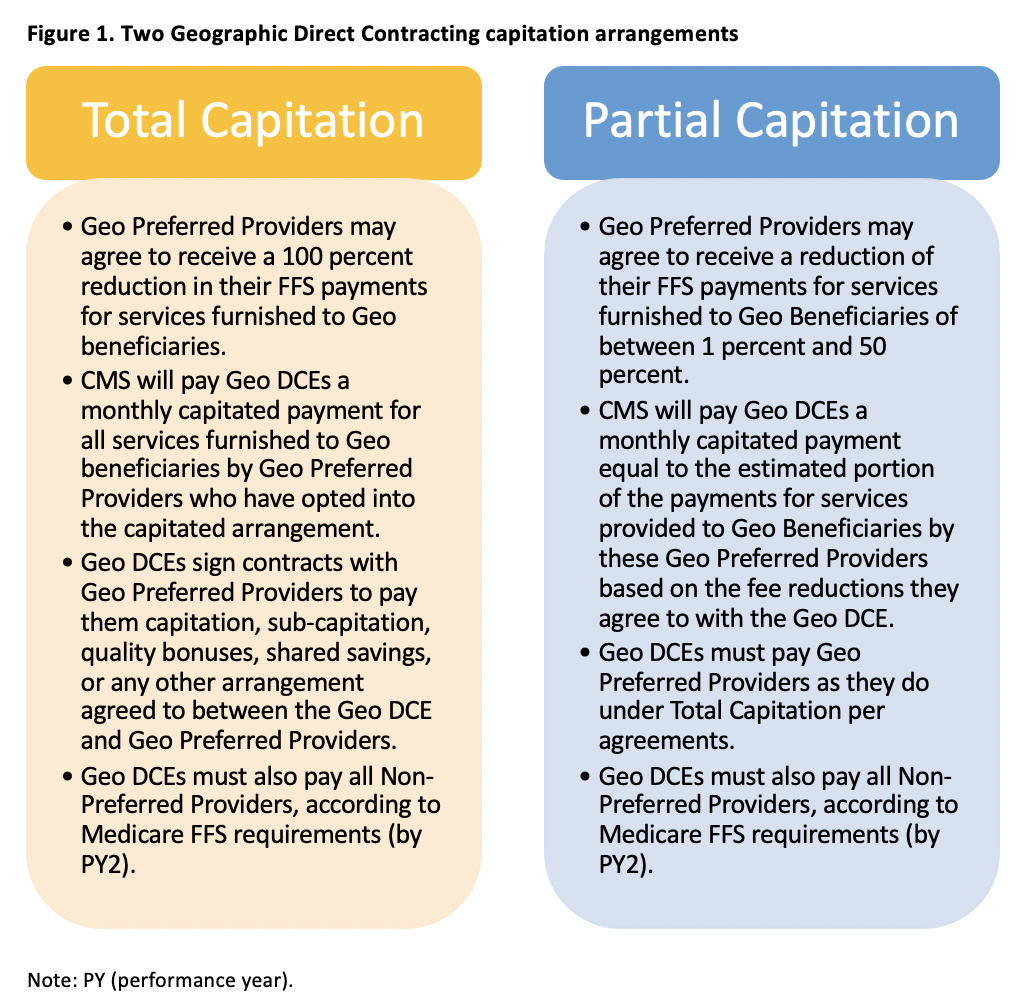
Geo DCEs’ responsibility for beneficiaries’ total cost of care will be facilitated through the use of capitated payments. Geo DCEs will choose between Total Capitation or Partial Capitation (Figure 1). This choice is driven by and affects contracts with Geo Preferred Providers and other providers and the arrangements between the Geo DCEs and CMS.
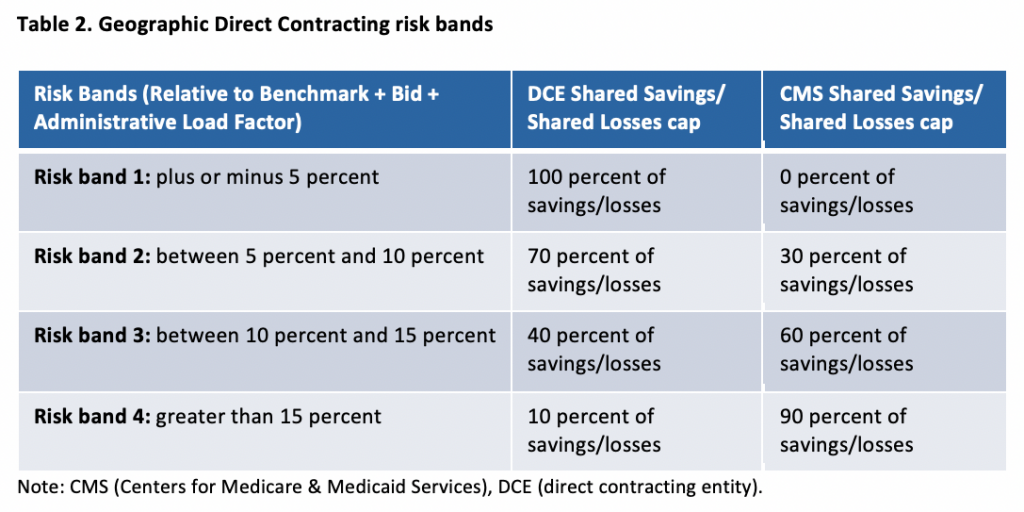
A Geo DCE’s ultimate shared savings and losses will be based on its proposed “savings discount” bid and its performance against a region’s Performance Year Benchmark and will be subject to risk corridors, risk adjustment, and quality adjustments. As part of their application, applicant Geo DCEs will bid on how much savings they expect to achieve in each of the performance years relative to typical FFS spending. This savings discount will be subtracted from Geo DCE payments and will contribute to calculation of the total cost of Geo DCE care that will be compared to the Performance Year Benchmarks, which will be set using a Geographic Rate Book, similar to the MA Rate Book. Geo DCEs’ shared savings and shared losses will be subject to the risk corridors shown in Table 2.
Conclusion
The decision to apply for the Geographic Direct Contracting demonstration and elections for each of the model characteristics can have a substantial impact on potential shared savings and losses and has the potential to shape the future of Medicare FFS program. HMA staff have extensive experience in assessing the implications of these decisions for the Geographic Direct Contracting model and other Innovation Center opportunities. If your organization is interested in assessing its Geographic Direct Contracting opportunities, contact Jennifer Podulka to learn how our expert team can assist with a data-based consultation.