This week, our In Focus section reviews the draft Medi-Cal Managed Care Plans (MCPs) request for proposals (RFP) released on June 1, 2021, by the California Department of Health Care Services (DHCS). California will procure MCPs for the Two-Plan Model, Geographic Managed Care (GMC), Regional Model, Imperial Model, and San Benito Model. This RFP excludes County Operated Health Systems (COHS) Plans and Local Initiative Plans. Of the total 13.5 million Medi-Cal beneficiaries, there are nearly 11.6 million in Medicaid managed care, of which approximately 3.5 million will be served under this RFP. A final RFP release date is still “to be determined” but expected in late 2021. Feedback on the draft RFP is due July 1, as well as voluntary non-binding letters of intent. A pre-proposal web conference will be held on June 10.
MCPs will provide medical, dental, mental health, substance use treatment services, and long-term care for Medicaid beneficiaries and incorporate the initiatives of California Advancing and Innovating Medi-Cal (CalAIM). View our In Focus covering CalAIM. Contracts will run for five years. DHCS may extend the contracts.
DHCS is looking for MCPs that can demonstrate their ability in:
- Quality
- Access to Care
- Continuum of Care
- Children Services
- Behavioral Health Services
- Coordinated/Integrated Care
- Reducing Health Disparities
- Increased Oversight of Delegated Entities
- Local Presence and Engagement
- Emergency Preparedness and Ensuring Essential Services
- Addressing Social Determinants of Health
- CalAIM
- Value-based Purchasing
- Administrative Efficiency
Awards
California will select plans by model and county as described in the table below.
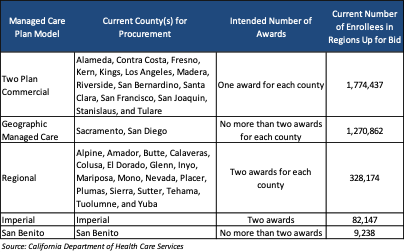
Contracts will be awarded to MCPs in each county with the highest total score(s). The evaluation criteria/scoring for proposals is still under development and will be available in the final RFP. For two-plan models, DHCS reserves the right not to award a commercial health plan contract to an MCP that will be contracted, subcontracted, affiliated, or otherwise entered into a partnership arrangement to serve as a Local Initiative in the same two-plan model, or has indicated an intent to do so.
Enrollment figures may shift as DHCS announced on May 7, 2021, a list of counties that submitted a full letter of intent to transition to a local Medi-Cal managed care plan model by January 2024. Counties intending to move to a single plan COHS model include Alameda (with Alameda Alliance for Health), Contra Costa (with Contra Costa Health Plan), and Imperial (with California Health and Wellness). The following counties intend to join with an existing COHS: Mariposa and San Benito (to join Central California Alliance for Health), and Butte, Colusa, Glenn, Nevada, Placer, Plumas, Sierra, Tehama, Sutter and Yuba (to join Partnership Health Plan). Alpine and El Dorado counties submitted their full letter of intent to join an existing two-plan model with Health Plan of San Joaquin. Counties that do not provide an executed county ordinance by October 1 to formalize their choice will be precluded from changing their model type for the current procurement that takes effect January 1, 2024.
Current Market
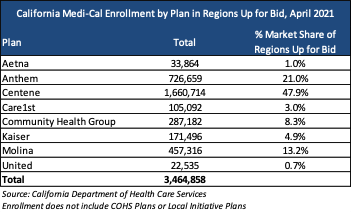
Below are the plans serving the regions that will be up for bid. Please note, this does NOT include plans and/or enrollment associated with COHS Plans or Local Initiative Plans. Other managed care organizations that are in the California Medi-Cal market are not reflected below. An additional 8 million enrollees are in managed care.
The draft RFP can be found here: https://www.dhcs.ca.gov/provgovpart/rfa_rfp/Pages/CSBmcodmcpHOME.aspx