HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Stays the Course with Proposed Payment Updates for Medicare Advantage and Part D Services in 2026

- Iowa to Seek Medicaid Work Requirements Demonstration

- Maryland Receives Approval for Section 1115 Demonstration Reentry Services Amendment

- Michigan Issues Competitive Grant Funding Opportunity for Statewide Crisis Intervention Services

- New York Governor to Prioritize Mental Health, Prescription Drug Costs

- Utah Receives Federal Approval for Section 1115 Medicaid Demonstration Amendment for HRSN, Expanded Dental

- CMS Issues CY 2026 Marketplace Benefit, Payment Parameters Final Rule

- CMS Awards Planning Grants to Address Care Continuity for Justice-involved Individuals

- United, Amedisys Request Judge Throw Out Antitrust Lawsuit, End Divestment Deal with VitalCaring Group

- More News Here

In Focus
CMS Stays the Course with Proposed Payment Updates for Medicare Advantage and Part D Services in 2026
Trump Administration will Issue Final Policies
This week, our In Focus section examines the Centers for Medicare & Medicaid Services (CMS) calendar year (CY) 2026 Advance Notice for the Medicare Advantage (MA) and Medicare Part D programs, published January 10, 2025. That same day, CMS also released draft CY 2026 Part D Redesign Program Instructions. This regulatory guidance includes CY 2026 payment updates as well as additional technical and methodological changes to MA and Part D for the coming plan year.
The release of the CY 2026 Advance Notice—along with the complementary CMS policy and technical proposed rule released in November 2024—represent the last major Medicare regulations of the Biden Administration, and these annual payment and policy updates will be finalized under the incoming Trump Administration. As a result, the proposed MA and Part D payment policies could be modified before finalization in April 2025.
Comments on the Advance Notice are due by February 10, 2025, leaving a tight timeline for MA plans and other stakeholders to provide formal feedback and written comments to CMS. Following are brief summaries of the major proposals in the Advance Notice and key considerations for stakeholders as they analyze the proposals.
Payment Impact on Medicare Advantage Organizations
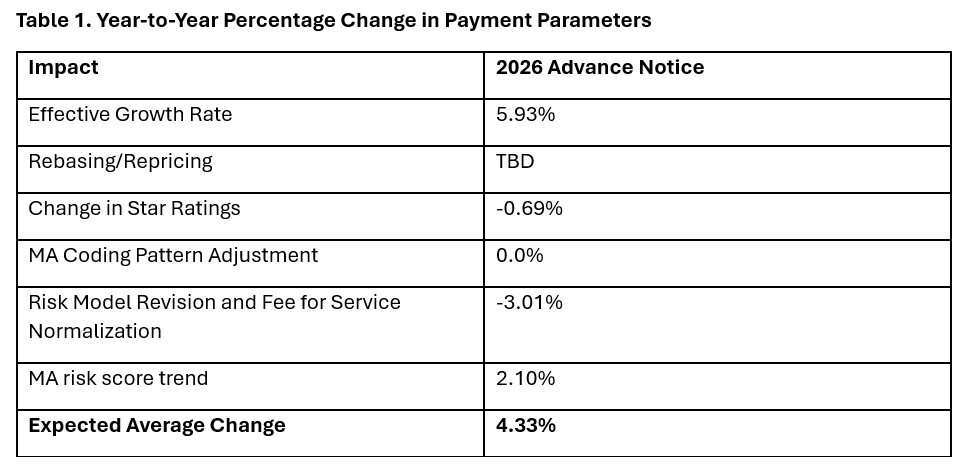
In the Advance Notice, CMS projects that federal payments to MA plans will increase by 4.33 percent from 2025 to 2026—which represents a $21 billion increase in expected payments to MA plans next year. CMS estimates that federal payments to MA plans in 2026 will total $590.9 billion.
The proposed increase in payments accounts for several factors, including growth rates in underlying costs, changes to MA Star Ratings, continued implementation of the new risk adjustment model, and MA risk score trends. The estimated growth rate considers demographic changes in MA enrollment, including projected increases in the number of enrollees.
The Advance Notice estimates represent the average increase in payments to MA plans and actual payments will vary from plan to plan. Below, Table 1 provides estimates of the impact of proposed policy changes on net MA plan payments.
MA Risk Adjustment Changes
CMS intends to complete the three-year phase-in of the MA risk adjustment model that was first published in the CY 2024 Rate Announcement. Specifically, CMS proposes to calculate 100 percent of the risk scores using the new MA risk adjustment model, referred to as the 2024 hierarchical condition categories (CMS-HCC) framework. CMS maintains that the changes to the methodology for calculating risk have improved the predictive accuracy of the model while ensuring risk-adjusted payments to MA plans are accurate.
In addition, CMS has been working to calibrate the risk adjustment model based on MA encounter data, and CMS proposes to begin phasing in an encounter-based MA risk adjustment model as soon as CY 2027.
CMS also proposes to apply the statutory minimum MA coding pattern difference adjustment factor of 5.90 percent for CY 2026.
Technical Adjustment to Cost Calculations Related to Medical Education Costs
Similar to changes in the MA risk adjustment model, CMS plans to complete the three-year phase-in of technical adjustments to the per capita cost calculations related to indirect and direct medical education costs associated with services delivered to MA beneficiaries. This technical adjustment—finalized in the CY 2024 Rate Announcement—has reduced growth rates for MA plans because of the removal of MA-related medical education costs from the benchmarks.
MA Star Ratings
CMS reiterates its continued focus on moving toward a “Universal Foundation” of measures with the goal of creating metrics that center on clinical care, patient outcomes, and improved patient experiences and are aligned across CMS programs. In addition, CMS is soliciting initial feedback on both substantive measure specification updates as well as comments on new measure concepts. CMS also is seeking stakeholder feedback on modifications to the Health Equity Index, including adding social risk factors and geography (urban or rural) to the reward factor. Any specific changes to MA Star Ratings measures, including modifications to the Health Equity Index, would occur through the formal rulemaking process.
Medicare Part D Provisions
The CY 2026 Advance Notice and the CY 2026 Draft Part D Redesign Program Instructions include several payment and benefit updates as required in the Inflation Reduction Act (IRA) of 2022. The CY 2026 updates include:
- The CY 2026 annual out-of-pocket cost threshold for Part D covered drugs is $2,100, which is the original out-of-pocket cap of $2,000 adjusted for the annual percentage increase in average expenditures for Part D covered drugs
- Establishment of the selected drug subsidy program
- Changes to the liability of enrollees, plan sponsors, drug manufacturers, and CMS in the standard Part D benefit design, specifically to account for the start of the Medicare Drug Price Negotiation Program in 2026
- Guidance on the successor regulation exception to the IRA’s formulary inclusion requirement for selected drugs under the Medicare Drug Price Negotiation Program
Other previously implemented IRA reforms will continue in CY 2026, including no cost sharing for Medicare beneficiaries for Part D covered drugs in the catastrophic phase, which begins after the annual out-of-pocket threshold of $2,100 is reached; a $35 monthly cap on enrollee cost sharing for insulin; no cost sharing for adult vaccines recommended by the Centers for Disease Control and Prevention’s (CDC’s) Advisory Commission on Immunization Practices and covered under Part D; and the requirement for Part D plans to offer the Medicare Prescription Payment Plan to beneficiaries.
What to Expect
The CY 2026 Advance Notice includes important technical, programmatic changes and payment updates for MA and Part D plans, which will be finalized when CMS publishes the final CY 2026 Rate Announcement on or before April 7, 2025. MA plans and other stakeholders have a rigid timeframe to provide formal input and written comments to CMS before the February 10 deadline.
Like the policy and technical changes included in the MA proposed rule, the CMS Advance Notice payment updates will be finalized under the incoming Trump Administration. MA plans and other stakeholder can anticipate that the new leadership at the US Department of Health and Human Services and CMS will closely examine and take a fresh look at the proposed payment and policy changes. Though the current CMS leadership maintains that payment updates included in the Advance Notice are sufficient to support stability in MA premiums and benefits, proposed payment policies can be modified or delayed as the new leadership takes shape.
For example, officials in the Trump Administration could seek to delay the phase in of the risk adjustment changes as well as the technical adjustment regarding medical education costs, which CMS estimates would result in an additional $10.4 billion in payments to MA plans.
Connect With Us
Medicare experts at Health Management Associates, will continue to assess and analyze the policy and political landscape, which will determine the final policies included in the CY 2026 Rate Announcement. HMA experts have the depth of knowledge, experience, and subject matter expertise to assist organizations that engage in the rulemaking process and to support implementation of final policies, including policy development, tailored analysis, and modeling capabilities.
For details about the CY 2026 MA Advance Notice and its impact on MA and Part D plans, providers, and beneficiaries, contact our featured experts, Amy Bassano, Julie Faulhaber, and Greg Gierer.
HMA Roundup
Alaska
Alaska Awards MMIS Contract to Conduent. Conduent announced on January 15, 2025, that it was awarded a $92 million contract with Alaska to continue to operate and manage the state’s Medicaid Management Information System (MMIS) and modernize the system. Conduent has partnered with the state to deliver Medicaid Enterprise Systems technology solutions since 2007.
Florida
Florida Files New Lawsuit Over Premiums Provision in Federal 12-Month CHIP Eligibility Requirement. Bloomberg Law reported on January 8, 2025, that the Florida Agency for Health Care Administration (AHCA) has filed a lawsuit against the Centers for Medicare & Medicaid Services (CMS) and the U.S. Department of Health and Human Services over a provision included in federal regulations finalized in November 2024. The Medicaid and CHIP Eligibility rule requires states to continue coverage for children enrolled in the Children’s Health Insurance Program (CHIP) even when participants fail to pay premiums, which are required in the state’s CHIP program. AHCA claims the enrollment mandate exceeds CMS authority. Florida previously filed a lawsuit over the provision and has delayed implementation of the expansion of its CHIP program, called KidCare, due to the requirements in the final rule.
Hawaii
Hawaii Receives Federal Approval for Section 1115 QUEST Integration Demonstration Extension for HRSN, Reentry Services, Foster Youth. The Centers for Medicare & Medicaid Services announced on January 8, 2024, that it has approved Hawaii’s five-year extension to its Section 1115 Hawaii QUEST Integration demonstration, effective through December 31, 2029. New state authorities include health related social needs (HRSN) services related to nutrition; funding for HRSN infrastructure; a contingency management pilot for individuals with a stimulant use or opioid use disorder; non-medical transportation to and from HRSN and home and community-based services; coverage for former foster youth up to age 26; and coverage to certain incarcerated individuals, for up to 90 days prior to release in jails, prisons, and youth correctional facilities.
Iowa
Iowa to Seek Medicaid Work Requirements Demonstration. The Des Moines Register announced on January 14, 2025, that during the 2025 annual Condition of the State address, Iowa Governor Kim Reynolds said Iowa will pursue a Section 1115 demonstration for Medicaid work requirements for able-bodied adults. In addition, Reynolds proposed implementing higher Medicaid reimbursements for more complicated pregnancies and increased rates for nurse midwives. The Governor is also in favor of providing Medicaid coverage for doulas.
Kentucky
Kentucky Provider Tax Improving Hospital Margins. Kentucky Lantern reported on January 14, 2025, that the Hospital Rate Improvement Program (HRIP) has been improving hospital margins, according to the Kentucky Hospital Association. The association stated to the House Health Services Committee that without the program, state hospitals would be operating at a negative 6 percent margin. HRIP, which is a value-based program, provides an additional $2.2 billion in funding annually to Kentucky’s hospitals through a provider tax.
Maryland
Maryland Receives Approval for Section 1115 Demonstration Reentry Services Amendment. The Centers for Medicare & Medicaid Services (CMS) announced on January 13, 2025, that it has approved Maryland’s HealthChoice Section 1115 demonstration amendment to provide reentry services. The amendment authorizes the state to provide pre-release Medicaid coverage to eligible incarcerated individuals who are diagnosed with substance use disorder, serious mental illness, or both, up to 90 days before release from state-managed prisons and jails. The amendment also authorizes Maryland to expand the number of participant spaces in the Assistance in Community Integration Services pilot program. The HealthChoice demonstration is authorized through December 31, 2026.
Massachusetts
Massachusetts Governor Signs Law to Increase Private Equity Oversight. Modern Healthcare reported on January 8, 2024, that Massachusetts Governor Maura Healey signed legislation to require private equity investors, real estate investment trusts, and management service organizations to submit certain financial report and increased non-compliance fines. The law will also broaden the authority of the Massachusetts Health Policy Commission and allow the regulator to seek testimony from financial sponsors at its annual cost trends hearing. The law does not grant the state authority to completely block a private equity transaction.
Michigan
Michigan Issues Competitive Grant Funding Opportunity for Statewide Crisis Intervention Services. The Michigan Department of Health and Human Services (MDHHS) issued on January 15, 2024, a competitive Grant Funding Opportunity (GFO) worth a total of $1.8 million for crisis response initiatives that would establish or expand community-based mobile crisis intervention services statewide. MDHHS anticipates issuing up to seven awards to any applicable local public entity, including federally recognized tribal governments and local health departments. Awardees may receive up to $225,000 during the initial grant period from April 1, 2025, to September 30, 2025. A continuation of awards will be available for October 1, 2025, to September 30, 2027, with up to $775,000 per applicant. Grant applications must be submitted by February 11. The grants are part of an effort to expand behavioral health services in the state.
Minnesota
Minnesota to Release Section 1115 Medicaid Reentry Demonstration, Seeks Evaluation Plan Design Contractor. The Minnesota Department of Human Services released on January 10, 2025, a request for proposals (RFP) seeking a vendor to design a monitoring protocol and conduct evaluations for a new Section 1115 Medicaid Reentry Demonstration. The state directed the Minnesota Department of Human Services to submit an application to the Centers for Medicare & Medicaid Services (CMS) to implement a medical assistance demonstration project to provide health care and coordination services that connect to community-based services for individuals confined in state, local, or Tribal correctional facilities prior to community reentry. The selected contractor will need to provide an examination of pre-release carceral and community providers, provide insight and design planning for data collection and analysis, conduct the corresponding independent evaluation, and develop the mid-point assessment and interim and summative evaluation reports as required by CMS. Proposals are due February 20, with awards anticipated on April 2. The contract is expected to run from May 1, 2025 through April 30, 2030, with an optional contract extension up to a total of five years.
New Mexico
New Mexico to Increase Medicaid Rates for HCBS for Individuals with IDD. KRQE reported on January 9, 2025, that New Mexico received federal approval to increase Medicaid rates for services provided to individuals with intellectual and developmental disabilities (IDD), beginning in mid-January. The rate increases will apply to home and community based services (HCBS) programs including the Developmental Disabilities Waiver; Mi Via Waiver; and the Medically Fragile Waiver. Rate increases for the Developmental Disabilities and Medically Fragile Waivers will be retroactive to July 1, 2024, and the Mi Via Waiver increases will be retroactive to October 1, 2024.
New York
New York Governor to Prioritize Mental Health, Prescription Drug Costs. Crain’s New York reported on January 14, 2025, that New York Governor Kathy Hochul has proposed the state does more to address mental illness and prescription drug costs, as outlined in the 2025 State of the State Address. Hochul’s proposals include passing laws to allow for more involuntary commitments for severe mental illness, as well as expanding support for the state’s healthcare safety net by aiding financially struggling medical facilities and hospitals with funding through an expanded version of the Safety-net Transformation Program. Additionally, the governor aims to participate in the U.S. Food and Drug Administration’s program allowing states to import lower-cost drugs from Canada, introduce legislation requiring greater transparency from pharmacy benefit managers, direct the state Department of Health to evaluate access to prescription weight-loss drugs among Medicaid enrollees with cardiovascular health problems, and distribute $25 million from the Reproductive Freedom and Equity Grant Fund. New York is also implementing two workforce programs under a Section 1115 demonstration to expand the health, behavioral, and social care workforce.
New York Judge Authorizes State to Continue Implementation of Single Statewide Fiscal Intermediary for CDPAP. Bloomberg Law reported on January 14, 2025, that New York is able to move forward with its implementation of the single statewide fiscal intermediary (FI) for the $9 billion Consumer Directed Personal Assistance Program (CDPAP) after a judge ruled in favor of the state in a lawsuit that sought to block the move. The New York Department of Health will transition to a single FI April 1, 2025.
New York Judge Temporarily Blocks Fiscal Intermediary from Relaying CDPAP Consumer Data. Spectrum News reported on January 8, 2025, that a New York state Supreme Court judge has issued a temporary order to block one fiscal intermediary from sending patient data records for people in the Consumer Directed Personal Assistance Program (CDPAP) to a third party. This comes after the state Department of Health ordered nearly 700 fiscal intermediaries to send consumer data related to CDPAP by January 15, 2025, as the agency informs program users about the change to a single statewide fiscal intermediary. The temporary block only affects one fiscal intermediary and the Health Department is on track to transition to the single fiscal intermediary on April 1, according to Governor Kathy Hochul’s office.
New York to Crack Down on NEMT Medicaid Fraud. Crain’s New York Business reported on January 8, 2025, that New York is cracking down on potential Medicaid fraud in non-emergency medical transport (NEMT) after an investigation claimed that 54 transportation companies falsely billed Medicaid. All of the companies were issued cease-and-desist orders and 15 of them were ordered to repay stolen funds. New York Attorney General Leticia James cited lack of NEMT oversight for the increasing fraud.
Oregon
Oregon Extends Medicaid Coverage for Young Adults with Special Health Care Needs. The Oregon Health Authority (OHA) announced on January 8, 2025, that it has expanded Oregon Health Plan (OHP) benefits, vision and dental benefits, and the new health-related social need housing and climate benefits to certain individuals ages 19 and 20 through a new eligibility category called Young Adults with Special Health Care Needs (YSHCN). To qualify for YSHCN benefits, an individual must be 19 or 20, have a qualifying health need, and have an individual or family income up to 205 percent of the federal poverty level. OHA estimates that 4,000 people will newly qualify for OHP coverage and 15,000 current OHP members will qualify for enhanced benefits through the new eligibility category.
Oregon Medicaid Enrollees Face Dental, SUD Provider Shortages. The Oregon Health Authority announced on January 14, 2025, that more than half of Oregon dentists do not accept Medicaid, with approximately 12 percent of Oregonian dentists providing nearly all of the Medicaid treatment while 30 percent of the population is on Medicaid, according to a report by Oregon State University. The report found that in the Medicaid Management Information System, there are about 83,000 enrolled Medicaid providers, and of those 25,076 are mental health providers and 2,341 are substance use disorder (SUD) providers. Wages for most direct care workers are lower than for other entry-level jobs, but employers’ ability to raise their pay is limited by low Medicaid reimbursement levels.
South Dakota
South Dakota Governor Proposes Budget Cuts to State Social Services, Human Services Departments. South Dakota Searchlight reported on January 13, 2025, that South Dakota Governor Kristi Noem has proposed budget cuts to both the state Department of Human Services and the Department of Social Services for utilization adjustments, totaling $42 million during the current fiscal year and $38 million for the upcoming fiscal year. Noem aims to right-size the budgets to match utilization of programs in both departments, citing their budget reversions, totaling $77 million over 2023 and 2024. The governor also proposed a combined $25 million reduction for current fiscal year Medicaid enrollments, citing slower-than-expected enrollment after the state expanded Medicaid eligibility.
Utah
Utah Receives Federal Approval for Section 1115 Medicaid Demonstration Amendment for HRSN, Expanded Dental. The Centers for Medicare & Medicaid Services (CMS) announced on January 8, 2024, that it has approved Utah’s amendment to its section 1115 Utah Medicaid Reform demonstration. The amendment will allow the state to provide health-related social needs (HRSN) services and infrastructure support; non-medical transportation to and from HRSN services; expanded eligibility for adult dental services; and fertility preservation services for individuals up to age 50 that have been diagnosed with cancer.
National
CMS Issues CY 2026 Marketplace Benefit, Payment Parameters Final Rule. The Centers for Medicare & Medicaid Services (CMS) issued on January 13, 2025, a final 2026 Payment Notice which sets standards for the Health Insurance Marketplaces, including for issuers and brokers, and safeguards consumers from unauthorized changes to their health care coverage, effective January 15, 2025. The final rule also includes 2026 user fee rates for issuers, changes to calculations for the Basic Health Program, and annual public reporting of summary-level information from the Affordable Care Act (ACA) Quality Improvement Strategy which will begin January 1, 2026. A second Final Rule published withdraws a notice of proposed rulemaking regarding coverage of certain preventive services under the ACA.
CMS Awards Planning Grants to Address Care Continuity for Justice-involved Individuals. The Centers for Medicare & Medicaid Services (CMS) announced on January 13, 2025, that 12 states and territories were awarded funding in the first round of planning grants that will allow state Medicaid and Children’s Health Insurance Program (CHIP) agencies to address operational barriers and care continuity for Medicaid and CHIP-eligible people who are inmates at a public institution, including jails, prisons, and youth detention facilities. Awardees, which will receive up to $5 million over a four-year period, include Alaska, District of Columbia, Kentucky, Maine, Massachusetts, Nevada, New Mexico, North Dakota, Puerto Rico, South Dakota, Utah, and Virginia. Applications for the second round of funding closes on March 17, 2025.
HHS Releases AI Strategic Plan. Fierce Healthcare reported on January 14, 2025, that the U.S. Department of Health and Human Services (HHS) has released an artificial intelligence (AI) strategic plan outlining the agency’s goals for adopting responsible AI use to improve overall health. The plan will focus on AI use in medical research and discovery, medical product development, healthcare delivery, human services delivery, public health, cybersecurity and critical infrastructure protection, and internal operations. Healthcare delivery goals include accelerating AI innovation and adoption, promoting trustworthy and ethical AI use, promoting external validation for quality assurance, and using AI to empower the healthcare workforce. The strategic plan also outlines potential risks of AI use in each category.
U.S. Supreme Court to Rule on ACA Preventive Care Coverage Dispute. Health Payer Specialist reported on January 13, 2024, that the U.S. Supreme Court is expected to rule on a dispute over preventative care coverage under the Affordable Care Act. The Biden administration appealed to the Supreme Court following a U.S. Fifth Circuit ruling which sided with a group of conservative businesses who rejected providing full insurance coverage for HIV medications on religious grounds. The U.S. Supreme Court is expected issue a final ruling in June.
PBMs Generate Billions of Dollars by Marking Up Specialty Drug Prices, FTC Report Finds. The Hill reported on January 14, 2025, that the three largest pharmacy benefit managers (PBMs), CVS Caremark Rx, Cigna’s Express Scripts, and United’s Optum Rx, earned $7.3 billion in revenue between 2017 and 2022 through vertical integration and marking up the prices of specialty prescription drugs by as much as 1,000 percent, according to a secondary interim report released by the Federal Trade Commission (FTC). The report found that 41 percent of these specialty drugs dispensed at pharmacies affiliated with one of the top three PBMs were marked up between 100 and 1,000 percent, and 22 percent were marked up by more than 1,000 percent. The price markups were found to be in excess of the National Average Drug Acquisition Cost. FTC’s analyses did not include Medicaid, instead focusing on commercial and Medicare Part D prescriptions, due to the regulatory framework for pharmacy reimbursement policies differing for Medicaid plans and varying by state.
CMS Proposes 4.33 Percent Medicare Advantage Pay Raise Beginning CY 2026. The Centers for Medicare & Medicaid Services (CMS) released on January 10, 2025, the Calendar Year (CY) 2026 Advance Notice for Medicare Advantage (MA) and Medicare Part D plans to update payment policies. The advance notice complements CMS’ November 2024 proposed rule for CY 2026 MA and Part D plans, and would increase MA payments by 4.33 percent on average, a $21 billion jump from 2025 to 2026. The proposed increase factors in growth rates of underlying costs, changes to MA star ratings, ongoing implementation of the new risk-adjustment model, and risk score trends. The notice also proposes technical updates to MA and Part D to ensure accurate payments to plans and proposes to complete the three-year implementation of the risk-adjustment model. Additionally, CMS concurrently released the draft CY 2026 Part D Redesign Program Instructions. CMS is accepting public comments on the notice through February 10, 2025.
House Budget Committee Discusses Potential Medicaid, ACA Budget Cuts. Politico reported on January 10, 2025, that Republican Congress members have begun discussing potential options to offset the federal budget, including potential cuts to Medicare, Medicaid, and the Affordable Care Act (ACA). A list originating from the House Budget Committee outlined $5.7 trillion in potential savings over 10 years, including repeals of certain health rules made under the Biden administration totaling $420 billion in savings, and $2.3 trillion in Medicaid cuts, which could come from equalizing Medicaid payments for able-bodied adults, lowering the minimum Federal Medical Assistance Percentage, and implementing Medicaid work requirements. Other savings options include “reimagining” the ACA to save up to $151 billion by ending insurance subsidies and limiting coverage eligibility based on citizenship status, and finding $479 billion in savings in the Medicare program.
Top Part D Drugs Have Nearly Doubled in Price Since Entering the Market. CNBC reported on January 9, 2025, that 25 Medicare Part D brand-name drugs with the highest spending in 2022 have nearly doubled in price since they entered the market, according to an AARP Public Policy Institute report. These drugs, which are not currently subject to Medicare price negotiation, have been on the market for an average of 11 years. These lifetime price increases often exceeded the corresponding rate of inflation.
MACPAC Releases Brief on Effects of Mental Health in Postpartum Medicaid Beneficiaries. The Medicaid and CHIP Payment and Access Commission (MACPAC) released in January 2025, an issue brief exploring differences in reported health status, access to care, service utilization, and overall health between postpartum Medicaid beneficiaries with and without mental health conditions, using data from the Postpartum Assessment of Health Survey. The brief also includes a comparison of individuals with mental health conditions by payer type.
Industry News
United, Amedisys Request Judge Throw Out Antitrust Lawsuit, End Divestment Deal with VitalCaring Group. Modern Healthcare reported on January 9, 2025, that UnitedHealth Group and Amedisys have filed a motion asking a judge to dismiss the federal antitrust lawsuit filed in November by the U.S. Department of Justice over United’s $3 billion acquisition of the home health company, or require the agency to better define why the acquisition would suppress competition. The motion alleges the Justice Department failed to define which specific geographic regions would be negatively impacted in its lawsuit. Additionally, United terminated a divestment deal with VitalCaring Group, which was set to purchase some United home health locations to avoid additional antitrust concerns over the acquisition. Both parties have been released from the purchasing agreement.
Blue Shield of California Restructures, Names Lois Quam Chief Executive. Health Payer Specialist reported on January 8, 2025, that Blue Shield of California has created a new nonprofit parent called Ascendiun. Ascendiun will also cover two new entities: Altais and Stellarus. Altais will operate as a clinical services business, and Stellarus, a healthcare solutions division that aims to scale and sell Blue Shield’s pharmacy and technology offerings to other insurers. Blue Shield of California’s chief executive, Paul Markovich, will head Ascendiun and will be interim president of Stellarus. Lois Quam was named chief executive of Blue Shield of California.
Alignment Sues CMS Over 2025 Medicare Advantage Star Ratings. Health Payer Specialist reported on January 15, 2025, that Alignment Healthcare has filed a lawsuit against the U.S. Department of Health and Human Services and the Centers for Medicare & Medicaid Services (CMS) over the plan’s 2025 Medicare Advantage Star Ratings. The lawsuit alleges that CMS uses faulty data science in the score calculation and challenges the lawfulness of the agency’s choice to subcontract with independent outside reviewers to determine plan performance. Alignment is seeking a score recalculation, as well as compensation for financial damages.
MMM Healthcare Faces Lawsuit Over Shifting MA Physician Payments to FFS. Health Payer Specialist reported on January 15, 2024, that a group of primary care physicians filed a lawsuit against Puerto Rico-based MMM Healthcare, a subsidiary of Elevance Health, alleging that subcontractors informed them without due process in 2023 that their Medicare Advantage (MA) payments would be shifting to a traditional fee-for-service model. The suit, filed in federal district court in San Juan, claims the shift took place without the proper notice and appeals process required under MA rules and by their contracts. The group of doctors is seeking $200 million in damages.
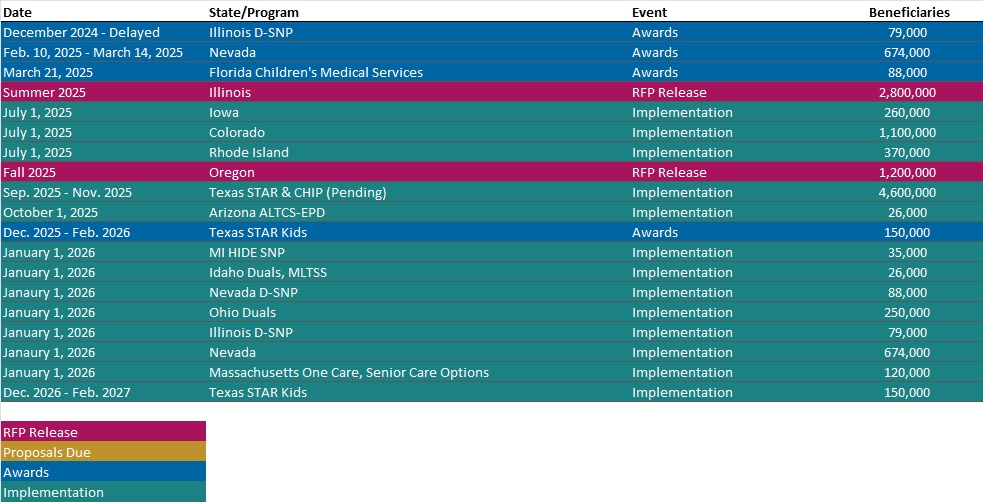
RFP Calendar
HMA News & Events
HMA Webinars
Improving Maternal Health Outcomes: Navigating CMS Guidance for Better Care. Tuesday, January 28, 2025, 12PM ET. Maternal health is at a critical turning point, and healthcare professionals are seeking innovative solutions to improve outcomes, reduce disparities, and ensure equitable access to care. This webinar highlights the latest CMS policies and guidance designed to address maternal mortality, expand access to high-quality care, and advance health equity for diverse populations. This session is ideal for hospital and critical access administrators, healthcare professionals, and policymakers dedicated to advancing maternal health and achieving better outcomes. Register Here
HMA Reports
Los Angeles County State of Children’s Health Report: Policy Briefs. Informed by research and exploration of the on some of the most complex challenges facing children in a post-pandemic world, experts from L.A. Care Health Plan, the nation’s largest publicly operated plan, and Children’s Hospital Los Angeles (CHLA), one of the nation’s leading pediatric hospitals, unveiled their first-ever Los Angeles County State of Children’s Health report. The report, made up of four policy briefs, identified core issues impacting kids and teens and key recommendations to proactively address them. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
- Updated Medicaid Managed Care Enrollment for 300 Plans in 41 States, Plus Ownership, Updated 3Q24
- Updated Section 1115 Medicaid Demonstration Inventory
- Updated HMA Federal Health Policy Snapshot
- Updated Massachusetts State Overview
Medicaid Data
Medicaid Enrollment and Financials:
- Arizona Medicaid Managed Care Enrollment is Down 4.4%, Nov-24 Data
- Iowa Medicaid Managed Care Enrollment is Down 3%, Aug-24 Data
- Kentucky Medicaid Managed Care Enrollment is Down 7.9%, 2024 Data
- New Mexico Medicaid Managed Care Enrollment is Up 0.6%, Aug-24 Data
- New York Medicaid Managed Care Enrollment is Down 5.5%, Apr-24 Data
- New York CHIP Managed Care Enrollment is Up 13.7%, Apr-24 Data
- Ohio Medicaid Managed Care Enrollment is Down 6.6%, Oct-24 Data
- South Carolina Medicaid Managed Care Enrollment is Down 13.3%, Jul-24 Data
- South Carolina Dual Demo Enrollment is Down 16.8%, Jul-24 Data
- South Dakota SNP Membership at 4,844, Nov-24 Data
- Texas Medicaid Managed Care Enrollment is Down 9.2%, Aug-24 Data
- Texas Dual Demo Enrollment is 20,745, Aug-24 Data
- Washington Medicaid Managed Care Enrollment is Down 4.5%, Oct-24 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Minnesota Section 1115 Reentry Demonstration Evaluation Plan Contractor RFP, Jan-25
- Virginia Cardinal Care Medicaid Managed Care Contracts, FY 2024-25
Medicaid Program Reports, Data, and Updates:
- Colorado Health Care Policy & Financing Performance Plans, FY 2020-25
- Colorado Medicaid HEDIS Reports, 2013-24
- Colorado Health Plan CAHPS Reports, 2017-24
- Florida Medicare Advantage D-SNP Contracts, 2025
- Hawaii Quest Integration 1115 Waiver Documents, 2018-25
- Louisiana Medicaid Annual Reports, 2011-23
- Maryland HealthChoices 1115 Medicaid Waiver Documents, 2016-25
- Missouri CHIP and SMHB Annual Reports, 2016-23
- Texas Medicaid Managed Care Provider Network Adequacy Reports, Dec-24
- Texas HHS Quality Measures and Value-Based Payments Annual Reports, 2018-24
- Texas HHS Medicaid & CHIP Reference Guides, 2018-24
- Texas HHS Interoperability Report, Dec-24
- Texas HHS Permanency Planning and Family-based Alternatives Reports, 2020-25
- Utah Medicaid Reform 1115 Demonstration Waiver Documents, 2016-25
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
