HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: How States Are Shaping Medicaid Managed Care and Marketplace Participation

- Connecticut Medicaid Program Forecasts $210 Million Deficit in Fiscal 2025

- Illinois Releases D-SNP RFP

- Illinois to Release Medicaid Managed Care RFP Summer 2025

- Iowa Awards Health Link Medicaid Managed Care Contract to Centene

- New York Individual Marketplace Insurance Premiums to Rise in 2025

- New Mexico Private Marketplace Sees Less Than 5 Percent of Disenrolled Medicaid Beneficiaries Enrolling in Private Insurance

- Pennsylvania Releases CHIP RFA

- Tennessee Submits Section 1115 Waiver Amendment to Expand Coverage for Working Individuals with Disabilities

- CMS Issues State Guidance on Medicaid, CHIP Eligibility Renewal Timeliness Requirements

- Elevance to Enter Maryland, Florida, Texas Marketplaces in 2025

- The Ensign Group Acquires Skilled Nursing Facilities in Colorado, Kansas

- More News Here

In Focus
How States Are Shaping Medicaid Managed Care and Marketplace Participation
This week, our In Focus section reviews state policies designed to increase insurer participation in Medicaid managed care and Marketplace programs. As states seek to address healthcare costs, affordability, and consumer experiences, they are exploring a range of initiatives—from the rise of prescription drug affordability boards to cost containment commissions, cost growth benchmarks, transparency, and examination of mergers and acquisitions.
A notable trend is the use of state policy and purchasing power to encourage or mandate that Medicaid managed care organizations (MCOs) offer Marketplace plans. Dual-market participation can help smooth coverage transitions, ensure continuity of care, and expand consumer choice. The remainder of this article addresses original research and analysis of this trend by Health Management Associates, Inc. (HMA), experts Zach Sherman, Aimee Lashbrook, and Hannah Turner.
Current Landscape
In 2024, enrollment in the Marketplace program has surged to more than 21 million, approximately a 30 percent increase from 2023. This growth was largely attributed to the temporary enhanced subsidies that allowed more people to access affordable coverage. Over the past several regulatory cycles, federal policymakers also have taken steps to further align the Marketplace framework with Medicaid on key issues, such as essential community provider access, eligibility and enrollment processes, and plan design standards. In response, states are innovating to meet federal requirements while pursuing their own healthcare goals related to coverage, affordability, access, and healthcare outcomes.
Value Proposition
A compelling value proposition for Medicaid MCOs to participate in the Marketplace (and vice versa) includes the ability to market to and retain people moving from one program to another as life circumstances change. Dual-market participation also supports diversification and growth strategies. In fact, enrollment in the Marketplace has nearly doubled since 2020. For Medicaid MCOs in particular, expanding product offerings to include Marketplace plans presents a unique opportunity to leverage existing provider networks and reimbursement arrangements to deliver more competitive rates.
Consumers benefit when the same organization participates in both markets. Families with parents and children who obtain coverage under different programs have an opportunity to work with a single organization and choose providers from the same or overlapping networks. Income fluctuations may result in disenrollment from one program (e.g., Medicaid) and eligibility for a new program (e.g., Marketplace subsidies). Continuity of care policies can smooth these transitions in areas such as prior authorization, care management, and provider network.
State Strategies to Increase Dual-Market Participation
The Affordable Care Act expanded access to affordable health insurance coverage for as many as 45 million individuals by giving states the option to expand Medicaid and provide federal subsidies to people who purchase Marketplace plans. States are now using various strategies to encourage or require insurer participation in both programs to ease transitions for individuals and families “churning” from one program to another, increase competition and choice of Marketplace plans, and reduce the risk of coverage gaps. For example:
- Nevada is requiring any bidder that plans to respond to its upcoming Medicaid MCO procurement to separately submit a “good faith” response to the Battle Born State Plans (BBSP) RFP. This state-contracted, public option will be available on the Silver State Health Insurance Exchange beginning in 2026. Failure to submit a good faith proposal will disqualify an organization from participating in the Medicaid MCO procurement later this fall. Nevada’s current Medicaid MCOs must participate in the Marketplace by offering at least one Silver and one Gold qualified health plan (QHP) that has overlapping provider networks, serves the same service area, and charges reasonable premiums.
- Rhode Island and New Mexico require or intend to require that their Medicaid MCOs participate in the Marketplace. As an awardee of Rhode Island’s recent Medicaid MCO procurement, UnitedHealthcare, must reenter the HealthSource Rhode Island market in 2027. These states also have designed their Medicaid MCO auto-assignment methodology to favor enrollment in a Medicaid MCO affiliated with an individual’s previous Marketplace plan or a family member’s Marketplace plan.
- In its last Medicaid MCO procurement (2018), North Carolina offered bonus points to any bidder that agrees to offer a Marketplace MCO. The resulting contract codified the market entry commitment and included implications for failure to follow through. Nonfulfillment could result in the highest level of contract noncompliance and associated penalties.
- Arkansas expanded its Medicaid program using federal matching funds to purchase QHP coverage through the Marketplace. Minnesota, one of the few states offering a basic health program, contracts with the same organizations to provide coverage under both programs.
- Iowa uses contract language to encourage, but not require, Medicaid MCOs to participate in the Marketplace to facilitate continuity of care during coverage transitions.
The Centers for Medicaid & Medicare Services (CMS) collaborated with states to promote continuity of coverage following the end of the Medicaid continuous enrollment requirement established in the Families First Coronavirus Response Act of 2020, also known as the Medicaid public health emergency (PHE) unwinding. This support includes the clarification of permissible outreach activities by Medicaid MCOs that also offer a Marketplace plan, information sharing, and other assistance. Many states have incorporated the CMS guidanceiii into Medicaid MCO contracts. North Carolina, Utah, and West Virginia include additional contract terms supporting their Medicaid MCOs’ ability to co-market Medicaid and Marketplace plans, including when an individual is losing Medicaid eligibility.
What to Watch For
Coverage transition challenges throughout the Medicaid PHE unwinding have highlighted the real-life impact of coverage gaps and the importance of policies and practices that promote uninterrupted access to healthcare coverage. Historic Marketplace enrollment levels and recent CMS guidance clarifying the allowability of outreach to people who are losing Medicaid coverage about Marketplace plan available make the prospect of dual-market participation increasingly attractive for Medicaid MCOs. A greater focus on improving continuity of care and Marketplace plan choice may lead to more states encouraging or requiring Medicaid MCOs to participate in the Marketplace.
Connect with Us
The upcoming HMA event, Unlocking Solutions in Medicaid, Medicare, and Marketplace, will offer more opportunities to engage with leaders from various sectors who are advancing innovations in Medicaid managed care and Marketplace programs and the points at which these programs intersect. State Medicaid and insurance commissioners, health plan executives, and community leaders, among others, will share insights into their market success and initiatives designed to address healthcare costs and insurance affordability.
Experts from HMA and our family of companies have extensive experience in the policy, structure, and administration of healthcare markets and health plan contracting. For more information, contact Zach Sherman.
HMA Roundup
California
California Gold Coast Health Plan Replaces CEO
Ventura County Star reported on August 30, 2024, that Ventura County’s managed care Medi-Cal plan Gold Coast Health Plan (GCHP) has named current chief medical officer Dr. Felix Nuñez as interim chief executive. The county’s Medi-Cal Managed Care Commission is searching for a permanent replacement after voting to not extend its contract with Nick Liguori, who served as GCHP chief executive for two years. Nuñez, a family physician, has worked at GCHP for two years and stepped into the chief medical officer role last year. Read More
Colorado
Colorado Exceeds Medicaid Budget by Nearly $124 Million. The Denver Post reported on August 29, 2024 that Colorado exceeded its projected $16 billion Medicaid budget by about $123.8 million, or 1.2 percent in fiscal 2024. The Department of Health Care Policy and Financing underestimated how much care its traditional Medicaid patients would need. However the department has authority to continue paying claims even when over budget. Read More
Connecticut
Connecticut Medicaid Program Forecasts $210 Million Deficit in Fiscal 2025. CT Mirror reported on September 3, 2024, that Connecticut’s Medicaid program is facing a $210 million deficit in net expenditures for fiscal 2025 based on current trends that are exceeding budgeted levels, specifically in hospital outpatient, clinic, and pharmacy services. Additionally, the cost of coverage for undocumented children is increasing with over 15,000 children enrolled as of July 2024, although a portion of these costs were already budgeted under HUSKY B, partially offsetting the Medicaid shortfall. Lawmakers previously opted not to adjust a preliminary fiscal 2025 state budget as requested by Connecticut Governor Lamont. Lamont had proposed a $3.4 billion budget for the state Department of Social Services, up about $200 million from what lawmakers had approved in fiscal 2024. Read More
Illinois
Illinois Releases D-SNP RFP. The Illinois Department of Healthcare and Family Services (HFS) released a Dual Eligible Special Needs Plan (D-SNP) request for proposals (RFP) to replace the current Medicare-Medicaid Alignment Initiative (MMAI) demonstration. This procurement will transition the state to a Fully Integrated Dual Eligible Special Needs Plan (FIDE-SNP) model, which will include a requirement for plans to provide managed long-term services and support (MLTSS) beginning in 2027.
HFS will award multiple plans, which will provide whole-person, fully integrated care while addressing health equity, health related social needs, and social determinants of health. Plans will be expected to improve access and quality of community-based behavioral health services, improve quality of care in facilities, and reduce program opt-outs. Additionally, plans will need to describe the strategy for increasing the use of Alternative Payment Models (APMs) in Medicaid managed care in Illinois, particularly for behavioral health providers.
Proposals are due October 18 and awards are expected to be announced in December. Contract execution is estimated July 2025, with implementation January 1, 2026. Contracts will run through December 31, 2029, with extensions up to five years and six months. There are currently approximately 79,000 beneficiaries enrolled in MMAI through Aetna Better Health, Blue Cross Blue Shield of Illinois, Humana Health Plan, Meridian Health Plan, and Molina Healthcare, as of June 2024. Read More
Illinois to Release Medicaid Managed Care RFP Summer 2025. The Illinois Department of Healthcare and Family Services (HFS) announced on September 3, 2024, that it will release a request for proposals (RFP) for HealthChoice Illinois, the state’s statewide Medicaid managed care program, in summer 2025. HFS will host at least five stakeholder listening sessions where it hopes to receive public feedback prior to the procurement process, which is set to begin November 15. In-person sessions will be held September 12 and September 17, and all other sessions will be held virtually during the agency’s Medicaid Advisory Committee meetings. The state plans to implement new contracts in January 2027. Read More
Indiana
Indiana Must Provide Immediate Attendant Care for Medically Complex Children Amid Ongoing Litigation, Judge Rules. Indiana Public Media reported on September 2, 2024, that a federal judge has ruled the Indiana Family and Social Services Administration (FSSA) must provide immediate attendant care for two medically complex children whose families are involved in ongoing litigation over the state’s decision to stop reimbursing family members for home care starting July 1. The lawsuit, filed in May, argues that the state failed to provide necessary care to medically complex children and that it violates the federal Americans With Disabilities Act and could result in unnecessary institutionalization of children. FSSA will have to ensure that the rest of the children moved out of the program have in-home skilled nursing care, and that parents are reimbursed through the new Structured Family Caregiving program. Read More
Iowa
Iowa Awards Health Link Medicaid Managed Care Contract to Centene. The Iowa Department of Human Services (DHS) announced on September 3, 2024, its intent to award incumbent Centene/Iowa Total Care a contract to provide physical health, behavioral health, pharmacy services, and long-term services and supports (LTSS) for the state’s Health Link program, which consists of traditional Medicaid program, the Children’s Health Insurance Program (CHIP) known as Healthy and Well Kids in Iowa (Hawki), and the Iowa Health and Wellness Plan (IHAWP). UnitedHealthcare/United Healthcare Plan of the River Valley and UCare also submitted bids. Other incumbents are Anthem/Amerigroup and Molina Healthcare, with separate contracts that have options through June 2029. The contract term will run for four years, beginning July 1, 2025, with one two-year renewal option. Read More
Iowa Medicaid Pharmacy Benefit Administrator Contract Winner Seeks to Block Disclosure of Bid Information. The Gazette/Iowa Capital Dispatch reported on September 2, 2024, that OptumRx is seeking a court injunction to block the state from disclosing its bid information for the Medicaid pharmacy benefit administration (PBA) services contract. OptumRx won the procurement to provide claims processing and pharmacy clinical services and Medicaid managed care program oversight in relation to pharmacy services. The state indicated the company’s unredacted bid was being sought by MedImpact, a competing company that also bid on the contract. OptumRx alleges that the information sought by MedImpact would give MedImpact an advantage over competitors and that disclosure will serve no public purpose. Read More
Louisiana
Louisiana Seeks Feedback, Partnership to Implement CMS Maternal Healthcare Model. The Louisiana Department of Health (LDH) announced in August 2024 that it is seeking feedback and partnership from providers and stakeholders for a future funding opportunity for the Centers for Medicare & Medicaid Services (CMS) Transforming Maternal Health (TMaH) model. The model aims to develop and implement a whole-person approach to perinatal health for people enrolled in Medicaid and CHIP, addressing physical health, mental health, and social needs. Two LDH-hosted informational meetings will be held before the September 20 TMaH application deadline. CMS plans to announce awardees in December. Read More
Massachusetts
Massachusetts Medicaid ACOs Improve Care for Pregnant, Postpartum Enrollees. Medical Xpress/Boston University reported on September 3, 2024, that Massachusetts Medicaid Accountable Care Organizations (ACOs) were associated with increases in prenatal and postpartum office visits, postpartum depression screenings, and timely postpartum care, according to a new study led by Boston University School of Public Health (BUSPH). The study evaluated pregnancy and postpartum measures for ACO and non-ACO patients from 2016 through 2020. Based on the results, the study authors suggest that implementing Medicaid ACOs could improve improve maternal health outcomes. Read More
New Mexico
New Mexico Private Marketplace Sees Less Than 5 Percent of Disenrolled Medicaid Beneficiaries Enrolling in Private Insurance. Source NM reported on August 30, 2024, that of the 219,100 people disenrolled from New Mexico’s Medicaid program during the post-pandemic unwinding process, 10,483, or about 4.7 percent, found coverage through the state’s private marketplace, BeWell NM. In July, the state reported it reinstated Medicaid coverage for approximately 21,000 children to provide families more time to pursue their coverage renewal. Read More
New York
New York Individual Marketplace Insurance Premiums to Rise in 2025. Crain’s New York Business reported on September 3, 2024, that individual marketplace insurance premiums are set to rise about 12.7 percent on average, approximately 4 percent less than requested by insurance companies, in 2025 due to high healthcare costs caused by prescription drug prices, hospital price increases, and taxes on insurance. Read More
New York Certified Home Health Agency Utilization Decreases. Crain’s New York Business reported on August 29, 2024, that New York home health agency enrollment in Medicare fee-for-service and Medicare Advantage programs, has declined by about 46,000 over five years, despite overall fee-for-service Medicare enrollment increasing. Meanwhile, enrollment for the state’s Medicaid Consumer Directed Personal Assistance Program (CDPAP) enrollment has expanded to cover more than 250,000 enrollees, with a 173 percent increase in the number of workers. Read More
North Dakota
North Dakota Submits Amendment Request for Section 1915 HCBS Demonstration. The Valley City Times Record reported on September 1, 2024, that North Dakota has submitted an amendment to its section 1915(c) waiver demonstration for home and community-based services (HCBS) to improve access to HCBS. The amendment would change allowable tasks for case management and broaden provider qualifications; update tasks for extended personal care services; and update language on the state’s nursing facility level of care process. Public comments will be accepted through September 26. Read More
Pennsylvania
Pennsylvania Releases CHIP RFA. The Pennsylvania Department of Human Services (DHS) released on September 3, 2024, a request for applications (RFA) for the Children’s Health Insurance Plan (CHIP), which provides comprehensive primary and behavioral healthcare services across all 67 counties to 168,000 children up to 19 years of age who are not eligible for or enrolled in Medicaid. Proposals are due October 18. Contracts will run for five years, with two one-year renewal options. Incumbents include Aetna Better Health, Capital BlueCross, Geisinger, Health Partners, Highmark HMO, Independence BlueCross/Keystone Health Plan East, UnitedHealthcare, and UPMC.
The draft CHIP agreement included in Appendix B of the RFA describes the options and requirements associated with value-based purchasing (VBP) and other key issues. Regarding VBP, the draft CHIP agreement indicates that CHIP managed care organizations (MCOs) will need to work toward implementing VBP Payment Strategies and Models. MCOs will need to enter into approved low, medium, or high-risk VBP payment arrangements with providers, which have to include quality benchmarks, as well as financial incentives and/or penalties to encourage quality care. These can include performance-based contracting, shared savings, shared risk, bundled payments, or global payments. All MCOs will be required to participate in patient centered medical homes. They will also have the option of participating in Accountable Care Organizations. MCOs will ramp up their VBP financial strategies, with 10 percent of the medical portion of the capitation rate being expended through VBP in contract year 1. In subsequent years, MCOs must incorporate community-based organizations into their VBP arrangement with providers to address social determinants of health, such as childcare, clothing, employment, food insecurity, housing, transportation, and utilities. Read More
Pennsylvania Allowed $7 Million in PBM Spread Pricing Due to Lack of Oversight, Audit Finds. ABC 27 News reported on August 28, 2024, that pharmacy benefit managers (PBMs) in Pennsylvania retained nearly $7 million more than they were entitled to in 2022 for Medicaid prescription drug transactions. This overage was attributed to insufficient oversight by the Department of Human Services (DHS), according to a performance audit conducted by the state’s Auditor General. The audit found that DHS did not effectively monitor the Physical HealthChoices Medicaid program’s 2022 expenditures, nor did it properly monitor the contracts between Medicaid managed care organizations (MCOs) and pharmacy benefit managers (PBMs), which resulted in spread pricing through undisclosed drug transmission fees that PBMs retained. PerformRX, the primary PBM identified in the audit, was found to be transparent with pharmacies about transmission fees, but not adequately transparent about fees with MCOs or DHS. State officials disputed the audit findings. Read More
Tennessee
Tennessee Submits Section 1115 Waiver Amendment to Expand Coverage for Working Individuals with Disabilities. The Centers for Medicare & Medicaid Services (CMS) announced on August 29, 2024, that Tennessee has submitted an amendment for its Section 1115 TennCare demonstration. This amendment aims to establish a Work Incentives Group designed to offer coverage for working individuals with disabilities whose income or resources exceed the thresholds for current coverage categories. Under this new Work Incentives Group, individuals would pay monthly premiums equal to 5 percent of their countable earned and unearned income. The public comment period will be open through September 28. Read More
Wisconsin
Wisconsin Announces Maternal Health Innovation Bridge Project Grant Funding. The Wisconsin Department of Health Services (DHS), Division of Public Health announced on August 20, 2024, a $400,000 grant funding opportunity for organizations looking to implement Maternal Health Innovation Bridge Projects, which aim to reduce maternal mortality and morbidity by improving maternal healthcare and reducing maternal health disparities. Projects eligible for funding must serve one of three focus areas: Wisconsin’s Native American/American Indian population; Medicaid beneficiaries or those who are uninsured in the Southern region; or Medicaid beneficiaries or those who are uninsured in the Northern and/or Western region. DHS will issue up to twelve awards between $25,000 and $50,000 for use between January 1, 2025, and September 30, 2025. Applications are due September 24. Read More
National
CMS Issues State Guidance on Medicaid, CHIP Eligibility Renewal Timeliness Requirements. The Centers for Medicare & Medicaid Services (CMS) issued on August 29, 2024, an informational bulletin and slide deck to provide states with guidance on staying compliant with federal regulations for timely processing of Medicaid and Children’s Health Insurance Program (CHIP) eligibility renewals. The guidance also explains the temporary revisions to the deadlines for states to complete eligibility renewals, address persistent backlogs in processing redeterminations, and ensure that states achieve compliance with federal renewal timeliness requirements by December 2025. Read More
Medicaid, CHIP Enrollment Drops by 841,000 in May 2024, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) announced on August 30, 2024, that Medicaid and Children’s Health Insurance Program (CHIP) enrollment was nearly 81 million as of May 2024, down by 840,795 from April 2024. Medicare enrollment was 67.4 million, an increase of nearly 123,000 from April 2024, including nearly 34 million enrolled in a Medicare Advantage plan. More than 8 million were dually eligible and counted in the enrollment totals for both programs. Read More
CMS Suspends 450 Marketplace Brokers Over Fraud, Abusive Conduct Suspicions. Health Payer Specialist reported on August 30, 2024, that the Centers for Medicare & Medicaid Services (CMS) has suspended 450 marketplace brokers for suspicion of fraud or abusive conduct related to unauthorized enrollments and plan switches. CMS began practicing more stringent oversight of individual insurance brokers in July, adding rules that require brokers to be on a three-way phone call with the broker, plan, and enrollee to make changes to a plan or enroll a prospective beneficiary. The agency expects more suspensions to come as they continue with stricter anti-fraud practices. Read More
Industry News
Elevance to Enter Maryland, Florida, Texas Marketplaces in 2025. Health Payer Specialist reported on September 4, 2024, that Elevance Health’s Wellpoint subsidiary is entering the Marketplace in Maryland, Florida, and Texas in the 2025 plan year. The insurer will operate plans in 24 of the 67 counties in Florida; 24 of the 254 counties in Texas; and did not specify where plans will be sold in Maryland. Read More
UnitedHealthcare to Launch Simplified Prior Authorization Program October 1. Modern Healthcare reported on September 3, 2024, that UnitedHealthcare is launching a program to allow certain in-network providers to use a simplified prior authorization process for about 500 procedure codes, beginning October 1. The program will be offered across Medicaid, Medicare Advantage, individual Marketplace, and commercial business lines. Eligible providers must have submitted at least 10 eligible prior authorization requests over each of the past two consecutive calendar years, with an approval rate of 92 percent or higher. UnitedHealthcare estimates that roughly 20 percent of provider groups that submitted enough prior authorization requests qualify for the program. Read More
The Ensign Group Acquires Skilled Nursing Facilities in Colorado, Kansas. The Ensign Group announced on September 3, 2024, that it acquired the operations of seven skilled nursing facilities in Colorado and one in Kansas. The Colorado acquisitions include 106-bed Desert Willow Health and Rehabilitation Center; 133-bed Junction Creek Health and Rehabilitation Center; 104-bed Pelican Pointe Health and Rehabilitation Center; 100-bed Riverbend Health and Rehabilitation Center; 100-bed Broadview Health and Rehabilitation Center; 107-bed Westlake Lodge Health and Rehabilitation Center; and 110-bed Linden Place Health and Rehabilitation Center. The Kansas acquisition is 102-bed Prairie Ridge Health and Rehabilitation. Ensign currently has 323 healthcare operations across 14 states. Read More
Help At Home Acquires Several Georgia-Based HCBS Organizations. Home care provider Help at Home announced on September 4, 2024, that it has acquired several Georgia-based home and community-based services (HCBS) organizations, including Care By Your Side, One Care Health, and AAMedcare. The acquisition will expand Help at Home’s HCBS to more residents living in Southern Georgia. The Illinois-based provider serves 67,000 clients across 11 states. Read More
BrightSpring Health Services Acquires Florida-Based Haven Hospice Assets. BrightSpring Health Services announced on September 3, 2024, that it has acquired assets of North Central Florida Hospital and Haven Medical Group, known together as Haven Hospice. Haven Hospice holds a certificate of need in 18 Florida counties. The transaction was worth $60 million. Read More
CareTrust REIT Acquires Two Skilled Nursing Facilities. Real estate investment company CareTrust REIT announced on August 29, 2024, that it acquired two skilled nursing facilities in August for approximately $62.1 million. The company acquired a 125-licensed bed skilled nursing facility in the Mid-Atlantic and closed an investment in a 134-licensed bed skilled nursing facility located on the West Coast. CareTrust REIT has 222 skilled nursing facilities as of June 30. Read More
Steward Healthcare to Sell Six Massachusetts-based Hospitals. Modern Healthcare reported on August 29, 2024, that Steward Health Care has entered into definitive agreements to sell four of its Massachusetts hospitals and is finalizing agreements for two others. Massachusetts-based Lawrence General Hospital will purchase two Holy Family Hospital campuses, and Rhode Island-based Lifespan Health System will purchase Morton Hospital and St. Anne’s Hospital. Agreements are being finalized with Boston Medical Center for the sale of Good Samaritan Medical Center and St. Elizabeth’s Medical Center. Read More
RFP Calendar
HMA News & Events
HMA Webinars:
2025 Medicare Advantage Bids Are Over. Now What? Thursday, September 5, 2024, 11:30 AM ET. The Medicare Advantage (MA) market has had an eventful year, and the chaos is expected to continue. As plans begin their preparation for the upcoming 2026 Plan Year, what are the emerging trends in benefits, Stars, revenue optimization and the regulatory environment? Are you a Medicare Advantage health plan leader overwhelmed with all the changes in the industry? Register Here
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
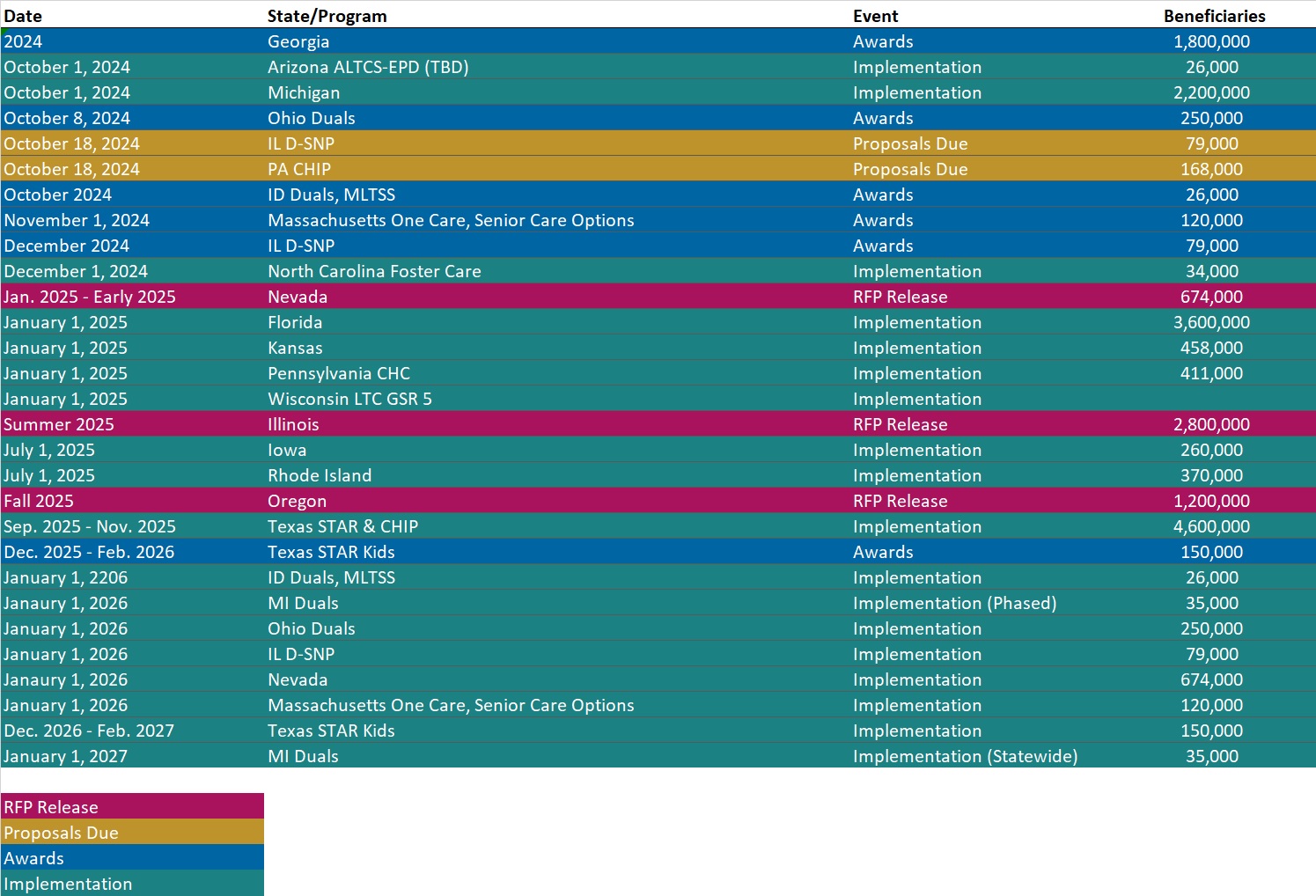
- Updated Medicaid Managed Care RFP Calendar: 50 States and DC
Medicaid Data
Medicaid Enrollment:
- Georgia Medicaid Managed Care Enrollment is Down 11%, Aug-24 Data
- Indiana Medicaid Managed Care Enrollment is Flat, Jan-24 Data
- Kansas Medicaid Managed Care Enrollment is Down 3.3%, Jun-24 Data
- Maryland Medicaid Managed Care Enrollment Is Down 2%, May-24 Data
- New Jersey Medicaid Managed Care Enrollment Is Down 14.4%, Jul-24 Data
- Wisconsin Medicaid Managed Care Enrollment is Down 10.9%, Jul-24 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Pharmacy Average Acquisition Cost Program RFP, Aug-24
- Illinois Dual Eligible Special Needs Plan (D-SNP) RFP, Sep-24
- Iowa Health Link RFP, Award, and Related Documents, 2024
- Iowa Pharmacy Benefit Administration Re-released RFP and Award, 2024
- Maine Project and Organizational Change Management for MES Health PAS Modernization Process, Aug-24
- Pennsylvania Children’s Health Insurance Plan (CHIP) RFA, Sep-24
- Wisconsin Maternal Health Innovation Bridge Project Grant Funding Opportunity, Aug-24
- Wyoming Medicare Advantage SNP Contract, 2025
Medicaid Program Reports, Data, and Updates:
- Indiana Medicaid External Quality Review Reports, 2012-23
- Kansas Joint Committee on HCBS and KanCare Oversight Meeting Materials, 2024
- Maryland Health Benefit Exchange Annual Reports, 2018-23
- North Dakota Home and Community-Based Services Waivers, 2018-24
- Pennsylvania Department of Auditor General PerformRx PBM Performance Audit, Aug-24
- Tennessee TennCare III 1115 Waiver Documents, 2021-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
About HMA
