Regulatory policy changes finalized by CMS aim to increase the percentage of dual-eligible individuals enrolled in integrated plans
This week, our In Focus section delves into important and complex regulatory policy changes that affect coverage and services for the 12.9 million individuals who are dually enrolled in both Medicare and Medicaid. These policy changes—which were finalized as part of a broader final rule that the Centers for Medicare & Medicaid Services (CMS) released on April 4, 2023—are designed to increase the percentage of dually eligible people who are enrolled in integrated Medicare Advantage (MA) Dual Eligible Special Needs Plans (D-SNPs). The modifications will be phased in gradually, with certain provisions affecting D-SNPs starting in 2025. These adjustments forge a stronger connection between state-level policy and operational decisions, shaping the future landscape of D-SNPs.
Overview
Amid rapid growth of D-SNP plan offerings and increased enrollment of dually eligible individuals into D-SNPs, CMS has finalized an interconnected set of regulatory policy changes to increase enrollment in integrated plans while simplifying coverage and plan options for this population.
By promoting enrollment in integrated plans, CMS seeks to improve the care experience and outcomes for dually eligible individuals, with the ultimate goal of making integrated plan enrollment the standard. Integrated D-SNP plans, which consolidate Medicare and Medicaid services under one managed care organization, offer uniform consumer protections (including unified grievance and appeals process), integrated plan materials, and more coordinated care.
Key policy changes include:
- Replacing the current quarterly special enrollment period (SEP) with a monthly SEP for dually eligible and other low-income subsidy (LIS) individuals to enroll into a standalone prescription drug plan (PDP)
- Establishing a new integrated care SEP that will enable dually eligible individuals to choose an integrated D-SNP plan on a monthly basis
- Restricting enrollment in certain D-SNPs to individuals also enrolled in an affiliated Medicaid managed care organization (MCO)
- Limiting the number of D-SNPs an MA organization can offer in the same service area as an affiliated Medicaid MCO to reduce and simplify plan offerings for dually eligible individuals.
What Issue is CMS Trying to Solve?
CMS intends to make it easier for dually eligible people make enrollment decisions. Simplified plan options and more integrated care could prevent beneficiaries from inadvertently selecting plans that fail to provide the comprehensive Medicare and Medicaid benefits they need.
This shift toward aligned enrollment could improve beneficiary experiences, enhance outcomes, and streamline administrative processes for CMS. The introduction of a monthly SEP specifically for dually eligible individuals enrolled in Medicaid managed care plans underscores CMS’s commitment to facilitating enrollment in affiliated D-SNP plans throughout the year. Health Management Associates (HMA) experts expect these changes to affect the sales cycle for dual eligibles and potentially increase member satisfaction, expand access to care, and improve overall health outcomes for this population.
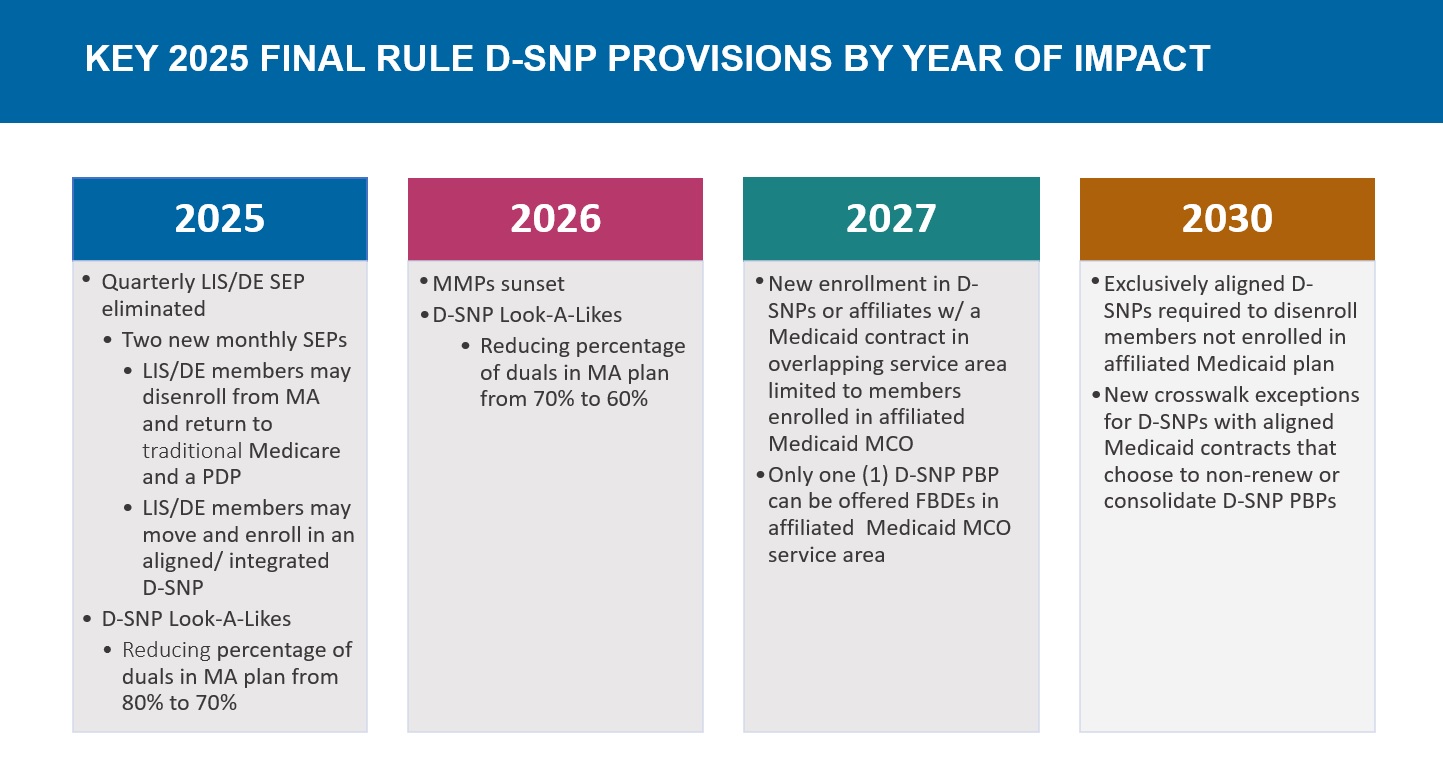
Timeline of Regulatory Changes
Considerations for Health Plans
The impact on individual health plans hinges on state-specific approaches to dually eligible beneficiaries and D-SNPs, as well as each plan’s strategy for integrating Medicare and Medicaid services. HMA experts identified the following key factors as essential for understanding and monitoring these interconnected dynamics:
- Does the state administer managed Medicaid, and if so, does it include the dually eligible population?
- Does the Medicare D-SNP (or an affiliated/ related company) hold a state Medicaid contract that covers dually eligible individuals?
- What is the state’s vision regarding duals and D-SNPs?
- Does the state require its Medicaid contractors to offer a D-SNP?
- Does the state currently or plan to restrict D-SNPs to their Medicaid contractors?
- Is the state moving toward an exclusively aligned enrollment model?
What’s Next
The changes in D-SNPs present opportunities and risks for beneficiaries, MA and Medicaid health plans, and states. Successful navigation of these changes requires proactive planning and anticipation of forthcoming federal and state regulations. Health plans operating within the D-SNP space must actively engage with state Medicaid agencies to understand and potentially help shape this evolving environment. For example, health plan strategies may include:
- Understanding the state’s priorities and its current and planned approach to integrated care for dually eligible individuals
- Participating in and/or advocating for stakeholder meetings with the state regarding dually eligible members and D-SNPs to ensure the opportunity to shape regulations
- Developing internal integration strategies that align product design, operations, quality, clinical, and member experience capabilities for D-SNPs and Medicaid
- Strategically planning actions, such as participating in Medicaid procurements, to achieve the plan’s objectives
Connect with Us
These regulatory changes significantly affect dually eligible beneficiaries, states, and both Medicare and Medicaid health plans. Though some changes may disrupt the duals’ market, others align state objectives with plan strategies. Ultimately, dually eligible individuals with full benefits will gain the most, experiencing improved opportunities to choose suitable plans, access necessary care, and achieve optimal health outcomes and well-being.
For further insights into these upcoming changes, view the D-SNP Growth and Integration: Key Implications of the 2025 CMS Final Rule webinar, featuring our experts below. Join them and other experts at HMA’s Fall Conference to stay informed about the strategic directions plans and states are pursuing.



