HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- HMA Opens Registration for Fall Conference: Unlocking Solutions in Medicaid, Medicare, and Marketplace

- In Focus: Takeaways from the Ensuring Access to Medicaid Services Final Rule

- California Governor Retracts on Budget Deal to Use MCO Tax Revenue for Medicaid, Hospital Investments

- Colorado Releases Accountable Care Collaborative Phase III RFP

- Colorado Releases Behavioral Health ASO RFP

- Florida Governor Signs Bill Allowing Medicaid Home Health Services Ordered by Nurses, Physician Assistants

- Kansas Announces Intent to Award KanCare, CHIP Medicaid Managed Care Contracts

- Michigan Invests $1.3 Million to Expand Hospital Rooming-in for Substance-exposed Babies

- Missouri House Committee Advances Medicaid Hospital Tax Renewal

- New York Releases RFA for Medicaid Housing Subsidies, Services through $87 Million Grant Funding

- Oklahoma Hospitals See Higher Payments Under Managed Care

- Texas Releases STAR Kids RFP

- CMS Extends Medicaid Unwinding-related Waiver Demonstrations to June 2025

- DOJ Creates Antitrust Task Force to Combat Healthcare Consolidations, Acquisitions Violating Laws

- Eventus WholeHealth Acquires Premier Geriatric Solutions

- More News Here

In Focus
HMA Opens Registration for Fall Conference: Unlocking Solutions in Medicaid, Medicare, and Marketplace
Unlock Solutions in Medicaid, Medicare, and the Marketplace at HMA’s Fall Conference, October 7−9
This week, we preview what to expect at the 7th annual Health Management Associates, Inc. (HMA) Fall Conference “Unlocking Solutions in Medicaid, Medicare, and Marketplace,” October 7−9, 2024, at the Marriott Marquis Chicago, IL. Learn more about our Keynote Speaker and take advantage of our Early Bird Registration.
Keynote Speaker Announced
We are pleased to announce our Keynote Speaker will be Darshak Sanghavi, MD, program manager at the Advanced Research Projects Agency for Health (ARPA-H)—a newly created multibillion dollar federal agency tasked with developing health programs that are “so bold no one else, not even the private sector, is willing to give them a chance.” His talk, “Unlocking Health Solutions through Innovation,” will highlight the innovative collaborations and projects ARPA-H is advancing. A trained clinician who has served in high level public and private sector advisory roles, Dr. Sanghavi will discuss how this new wave of research and innovations is changing how we think about healthcare’s challenges and will address why the agency is so important at this time. He will highlight ARPA-H investments and commitments and the timeline for impact, including how healthcare systems and states should be thinking about ARPA-H funded innovations and preparing for scaling breakthroughs that improve outcomes.
Before joining ARPA-H, Dr. Sanghavi was global chief medical and clinical operating officer for Babylon, the global end-to-end digital healthcare provider serving more than a dozen countries and 24 million-plus people, with the mission of bringing “affordable and accessible healthcare to everyone on earth.” He also has served in senior roles at UnitedHealthcare’s Medicare & Retirement, OptumLabs, the R&D hub of UnitedHealth Group, and in the Obama Administration as the Director of Preventive and Population Health at the Center for Medicare and Medicaid Innovation, where he directed the development of large pilot programs designed to improve the nation’s healthcare costs and quality. He is an award-winning medical educator, who has worked in medical settings around the world. He will draw on these diverse experiences to inspire and challenge attendees to unlock solutions to some of our healthcare system’s most complex issues.
Network with Leaders in Healthcare
This is an important moment for ever-changing publicly sponsored healthcare programs like Medicaid, Medicare, and the Marketplace, with greater focus on value and federal initiatives that encourage improved health equity, affordability, quality, and outcomes. Don’t miss out on this opportunity to form new partnerships as you dig into today’s urgent issues and immerse yourself in insightful discussions, networking opportunities, and engaging workshops on the new Medicaid managed care rule, applications for AI in healthcare, approaches to meet rural workforce needs, value-based care contracting, and insights from state Medicaid services.
Preconference tactical workshops will focus on exclusive tools, insights, and strategies to guide program design, navigate new regulatory frameworks, and advance value-based care. HMA’s premier national conference plenary and breakout sessions will focus on the landscape for innovation in healthcare, emerging service delivery models, and growth strategies in pursuit of improved value, quality, and better outcomes.
Who should attend?
Executives and leaders from federal, state, and local government agencies, health plans, payers, managed care, hospitals and health systems, provider and provider enablement organizations, community-based organizations, IT companies, life sciences organizations, investment firms, foundations, and associations.
Takeaways from the Ensuring Access to Medicaid Services Final Rule
This week’s second In Focus section delves into the Ensuring Access to Medicaid Services final rule. The Centers for Medicare & Medicaid Services (CMS) published the access rule May 10, 2024, alongside the similarly significant Medicaid managed care final rule. The two rules include new flexibilities and requirements aimed at enhancing accountability for improving access and quality in Medicaid and the Children’s Health Insurance Program (CHIP) across the fee-for-service (FFS) and managed care delivery systems and provide targeted regulatory flexibility in support of this goal.
Five Takeaways from the CMS Medicaid Managed Care Final Rule, which Health Management Associates, Inc. (HMA), published April 24, 2024, outlined key issues and implications that CMS advanced in the Medicaid managed care program. The Ensuring Access to Medicaid Services final rule, meanwhile, focuses on the following:
- Payment adequacy for direct care workers (80/20 rule)
- The role of self-direction and the 80/20 rule
- Establishment of a pathway to national benchmarking of Medicaid rates
- Potential impacts of the rule on programs that serve individuals with dual eligibility
Overview
The Ensuring Access to Medicaid Services finalized policies are designed to create an updated federal framework for Medicaid’s home and community-based services (HCBS) programs. These changes come at a pivotal time, as states are facing workforce shortages, particularly among HCBS direct care workers (DCWs). Table 1 provides an overview of several significant final policies.
Table 1. Ensuring Access to Medicaid Services: Overview of Final Rule Policies
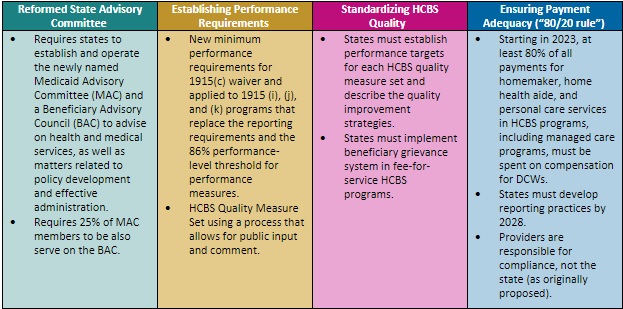
Below HMA reviews several key questions we are fielding regarding the impact of the rule.
Ensuring Payment Adequacy: How will states demonstrate that 80 percent of Medicaid payments go to direct care workers?
The final rule requires at least 80 percent of Medicaid payments be spent on compensation for DCWs workers, including homemaker, home health aide, and personal care services. In response to public comment, CMS adjusted the final rule to include some employer costs in the 80 percent calculation.
Recognizing it will take substantial time for providers to establish the necessary systems, data collection tools, and processes to collect the required information to report to states, CMS is providing states six years to implement the HCBS Payment Adequacy policy, and four years for reporting requirements. States and providers must ensure that that they are prepared to meet the payment adequacy requirements in the final rule. Being successful will require collaboration between states and providers, investments in systems, and analysis of – and potentially changes to – reimbursement levels.
How does the 80/20 rule apply to self-directed care?
CMS finalized its proposal to require that at least 80 percent of all payments for homemaker, home health aide, and personal care services in HCBS programs, including managed care programs, be spent on compensation for DCWs. In a change from its proposed policy, CMS limits the 80/20 compensation mandate to certain types of self-directed models. Specifically, the 80/20 rule will apply to models in which the beneficiary directing services does not set the payment rate for the worker, such as Agency with Choice and other self-directed models that use a fiscal intermediary or fiscal employer agent, in both managed care and FFS delivery systems. The compensation rule does not apply to self-directed models in which the beneficiary sets the rates paid to workers.
CMS will hold states accountable for compliance with the 80/20 rule, regardless of whether their HCBS are delivered through an FFS delivery system, managed care delivery system, or both. States will need to determine an approach to track compliance with the minimum performance requirement at the provider level, not the managed care plan level. States and managed care plans should collaborate to determine their respective roles in activities such as the data collection and mandatory reporting, and they should continue to seek and monitor clarifying guidance from CMS.
How will the Ensuring Access final rule affect national benchmarks in Medicaid rates? State Medicaid programs have many nuances that make it difficult to obtain applicable comparison data and best practices. Beginning July 1, 2026, the final rule requires that states publish their payment rates, specifically the average hourly Medicaid FFS fee schedule payment rates, separately identified for payments made to individual providers and provider agencies, if the rates vary. States also must conduct a comparative analysis of their base Medicaid FFS fee schedule payment rates with the Medicare non-facility payment rate. CMS does not, however, require that states change their payment rates based on the comparative analysis.
Payment rate transparency publications, comparative payment rate analyses, and payment rate disclosures present opportunities for states, MCOs, and providers to assess the adequacy of payment rates and their impact on access to services. The forthcoming data also will help federal and state level policymakers in their efforts to improve quality, access, and affordability. States will need to do baseline assessments comparing Medicaid and Medicare rates. States, managed care plans, and providers should monitor for CMS sub-regulatory guidance, including hypothetical examples of the service codes that would be subject to the comparative payment rate analysis.
Does the final rule affect integrated models of care for people who are dually eligible for Medicaid and Medicare? CMS finalizes policies that will have a variable impact on states and individuals dually eligible for Medicare and Medicaid because of differences in state approaches to integrated care for this population. For example, the new grievance system policies apply differently depending on the level of integration the state requires of Medicare Advantage (MA) dual-eligible special needs plans (D-SNPs) programs. Like grievance systems, states, providers, and MCOs should monitor how states address the final rules for critical incidents for individuals with dual eligibility when a Medicaid managed care plan is unable to access Medicare data.
CMS intends to provide additional sub-regulatory guidance and technical assistance to support implementation of policies that affect dually eligible individuals. States should verify their access to and readiness to use Medicare data related to the new requirements, and seek technical assistance to maximize use of these data for individuals enrolled in non-integrated D-SNPs. Commentors have also asked how the changes to the HCBS quality measure set may work in programs for dually eligible members.
Connect with Us
HMA is ready to support your efforts to understand and take action to account for the Ensuring Access to Medicaid Services final rule’s effects on your state’s or organization’s strategy and operations. Our experts are developing policies and procedures at the intersection of the access and managed care final rules. Please contact Susan McGeehan, Dari Pogach, and Patrick Tigue to connect with our expert team members on this vital set of issues.
HMA Roundup
California
California Governor Retracts on Budget Deal to Use MCO Tax Revenue for Medicaid, Hospital Investments. Politico Pro reported on May 10, 2024, that California Governor Gavin Newsom’s new budget plan proposes to use $7 billion of the $19 billion in revenue generated by the state’s new managed care organization (MCO) tax to reduce the budget deficit. The MCO tax revenue was originally intended to increase health care workers pay; help hospitals with compliance; increase reimbursement rates for emergency room doctors and ambulances; direct additional funding to public hospitals; and address workforce shortages. Read More
California Incorrectly Disenrolled, Renewed Medicaid Eligibility for Estimated 78,853 Beneficiaries, OIG Audit Finds. The U.S. Department of Health and Human Services announced on May 9, 2024, that an estimated 78,853 Medicaid beneficiaries in California had their coverage incorrectly renewed or incorrectly terminated during redeterminations from April 1 through August 31, 2023, according to an audit by the Office of Inspector General (OIG). In total, the state had renewed or terminated coverage for 1,830,923 enrollees during the audit period. The study looked at a sample of 140 individuals. OIG recommendations include the redetermination of eligibility for the sampled enrollees that were identified as having incorrect eligibility determinations and correcting system issues that caused incorrect Medicaid eligibility actions. Read More
Colorado
Colorado Releases Accountable Care Collaborative Phase III RFP. The Colorado Department of Health Care Policy and Financing released on May 10, 2024, a request for proposals (RFP) seeking contractors to serve as Regional Accountable Entities (RAEs) for the Department’s four regions of the Accountable Care Collaborative (ACC). The procurement launches phase III of the ACC, which is designed to reduce health disparities and improve access for members by streamlining and standardizing existing systems. Proposals are due July 13, 2024. The contract will include an initial start-up period beginning February 1, 2025, through June 30, 2025. Implementation of Phase III begins July 2025. The contract term will not exceed seven years. The incumbents are Colorado Access, Colorado Community Health Alliance, Rocky Mountain Health Plans, Health Colorado, Northeast Health Partners, and Denver Health Medicaid Choice. Read More
Colorado Releases Behavioral Health ASO RFP. The Colorado Behavioral Health Administration released on May 14, 2024, a request for proposals (RFP) seeking vendors to perform as Behavioral Health Administrative Service Organizations (BHASOs) to provide behavioral health services for each of the state’s four geographic regions, which aligns with Colorado’s Medicaid Accountable Care Collaborative Phase III regional map to be launched in 2025. BHASOs will establish, administer, and maintain regional networks of behavioral health care providers and implement community-based initiatives to improve care coordination, quality, and access. Proposals are due July 15, 2024. The contract will have an initial six-month start-up period from January 1, 2025, through June 30, 2025. The BHASO Network will officially launch on July 1, 2025, with five one-year renewal options. Read More
Florida
Florida Governor Signs Bill Allowing Medicaid Home Health Services Ordered by Nurses, Physician Assistants. Florida Politics reported on May 11, 2024, that Florida Governor Ron DeSantis has signed a bill allowing Medicaid to reimburse for home health services ordered by advanced practice registered nurses and physician assistants, effective July 1. Covered services include equipment and appliances, home health visits, and nursing and home health aide services. Read More
Illinois
Illinois Disenrolls Approximately 660,000 Medicaid Beneficiaries During Redeterminations Through April. STLPR reported on May 14, 2023, that Illinois has disenrolled approximately 660,000 Medicaid beneficiaries during redeterminations from March 2023 through April 2024, with about two-thirds losing coverage due to procedural reasons. The state renewed coverage for 2.6 million Medicaid beneficiaries and still has more than 300,000 pending eligibility cases. Read More
Indiana
Indiana Launches Monthly Medicaid Financial Reporting. The Indiana Capital Chronicle reported on May 10, 2024, that Indiana has launched a webpage with monthly Medicaid finance reports detailing expenditures, enrollment, and funding. As of February 2024, Medicaid expenditures were $102 million above the December 2023 forecast and $1.7 billion above expenditures from February of 2023. Medicaid enrollment across all programs and delivery systems totaled nearly 2 million individuals, which is 1.3 percent above the forecasted amount and 3.4 percent below enrollment in February 2023. Read More
Indiana Hospitals are Down $731 Million in 2023 Compared to Pre-COVID Levels, Report Finds. WFYI reported on May 9, 2024, that Indiana hospitals earned $358 million in operating income in 2023 – approximately $731 million less than the pre-COVID-19 pandemic levels, according to a Kaufman Hall report. Indiana hospitals cumulative operating margin is below 1 percent. Providers cite low reimbursements from Medicaid and Medicare as one of the contributing factors. Indiana’s hospital average Medicaid rates are below the median compared to other states, while charity care increased 21.6 percent in 2023. Read More
Iowa
Iowa Governor Signs Bill Extending Postpartum Medicaid Coverage, Limiting Eligibility. The Iowa Capital Dispatch reported on May 8, 2024, that Iowa Governor Kim Reynolds signed legislation extending Medicaid postpartum coverage to 12 months while lowering eligibility from 375 percent of the federal poverty level to 215 percent. Read More
Kansas
Kansas Announces Intent to Award KanCare, CHIP Medicaid Managed Care Contracts. The Kansas Department of Administration announced on May 14, 2024, its intent to award KanCare Medicaid & CHIP capitated managed care contracts to three health plans: incumbents Centene/Sunflower Health Plan and UnitedHealthcare, and non-incumbent Elevance/Healthy Blue. The program covers approximately 458,000 beneficiaries. Contracts will be effective January 1, 2025, through December 31, 2027, with up to two one-year renewal options. Read More
Michigan
Michigan Invests $1.3 Million to Expand Hospital Rooming-in for Substance-exposed Babies. The Michigan Department of Health and Human Services (MDHHS) announced on May 9, 2024, that it is investing $1.3 million in opioid settlement dollars to expand rooming-in options at five birthing hospitals across the state, which allows birthing individuals, caregivers, and substance-exposed babies to lodge in the same room after birth. Funding was provided to Hurley Medical Center in Flint, Covenant Medical Center in Saginaw, OSF St. Francis Hospital in Escanaba, University of Michigan Health-Sparrow Hospital in Lansing, and Bronson Battle Creek Hospital. Read More
Missouri
Missouri House Committee Advances Medicaid Hospital Tax Renewal. KBIA reported on May 14, 2024, that the Missouri House Budget Committee advanced legislation renewing the state’s Medicaid hospital tax through September 2029. The bill, which funds approximately a third of the state’s Medicaid program, now heads to the full House for further consideration. Read More
Governor Signs Bill Ending Medicaid Payments to Planned Parenthood. The Missouri Independent reported on May 8, 2024, that Missouri Governor Mike Parson has signed a bill prohibiting Medicaid from paying for health care services from any organization that affiliates with abortion providers, including Planned Parenthood. The new law will go into effect on August 28. Read More
New Mexico
New Mexico Failed To Recoup $139.2 Million in Nursing Care Overpayments to MCOs, Audit Finds. U.S. Department of Health and Human Services Office of Inspector General (OIG) released on May 13, 2024, an audit which found that New Mexico failed to recoup $139.2 million in community benefit (CB) services through managed care organizations (MCOs) for patients who did not use these services from April 2020 through June 2023. Total CB services capitated payments during this time period were $3.8 billion. The audit report also found that MCOs received a higher capitated payment whether serving nursing facility level of care (NFLOC) beneficiaries in a nursing facility or in their community. The OIG has recommended that New Mexico refund nearly $120 million in Medicaid NFLOC payments to the federal government, and recoup $139.2 million in capitated payments from its MCOs. Read More
New York
New York Releases RFA for Medicaid Housing Subsidies, Services through $87 Million Grant Funding. The New York State Department of Health (DOH) released on May 7, 2024, a request for applications (RFA) for the Medicaid Redesign Team Health Home Supportive Housing Program (HHSHP) to provide permanent rental subsidies and housing tenancy services to unhoused Medicaid members through $86.9 million in statewide grant funding. The state will make awards to no more than 17 organizations, with at least one award being made to each service area within the state. Some counties may have more than one award and applicants may apply to serve more than one service area. Applications are due June 27, and contracts are expected to run from October 1, 2024, through September 30, 2029. Read More
North Carolina
North Carolina Medicaid Expansion Enrollment Surpasses 450,000. WCCB Charlotte reported on May 9, 2024, that enrollment in the North Carolina Medicaid expansion program has surpassed 450,000 since launching in December. The program has also covered more than 1 million prescriptions for new enrollees and more than $17.9 million in claims for dental services. As of May, the state enrollment dashboard shows 112,199 enrollees live in rural communities and 37,394 enrollees are young adults. Read More
Oklahoma
Oklahoma Hospitals See Higher Payments Under Managed Care. Oklahoma Watch reported on May 8, 2024, that the Oklahoma Health Care Authority made its first enhanced directed payment to hospitals since the state transitioned to a new Medicaid managed care program, SoonerSelect, in April. Hospitals received $252.4 million, with a similar payment expected in July. The enhanced directed payments, which fall under the Supplemental Hospital Offset Payment Program (SHOPP), are unrestricted. These enhanced payments are supported by the SHOPP’s 4 percent provider tax for hospitals. Read More
Pennsylvania
Pennsylvania Lawmakers Advance Marketplace Subsidies Bill. The Pittsburgh Post-Gazette reported on May 11, 2024, that the Pennsylvania House Insurance Committee advanced a bill that would provide subsidies to Pennsylvanians who buy healthcare insurance through the state’s Marketplace, Pennie. The legislation is intended to assist thousands of Pennsylvanians who were disenrolled from Medicaid following the end of the COVID-era Medicaid continuous enrollment requirement. The legislation heads to the full House for a vote. Read More
Pennsylvania Senator To Introduce Medicaid-covered Doula Bill. The Pennsylvania Capital-Star reported on May 9, 2024, that a bill expected to be introduced in the Pennsylvania Senate would require Medicaid to cover doula services for prenatal, delivery, and postpartum care. The bill looks to address the disparate maternal mortality rates for Black and Indigenous women, as well as overall maternal health for all women. This follows the passage of a similar bill in the House. Read More
South Carolina
South Carolina Bill to Merge Six Public Health Agencies Dies in Senate. The Associated Press reported on May 9, 2024, that a bill to merge six separate South Carolina state public health agencies into a single Executive Office of Health and Policy has died in the Senate. The agencies encompassed the Department of Alcohol and Other Drug Abuse Services, Disabilities and Special Needs, Health and Human Services, Mental Health and Aging, and the newly created Department of Public Health. Read More
Texas
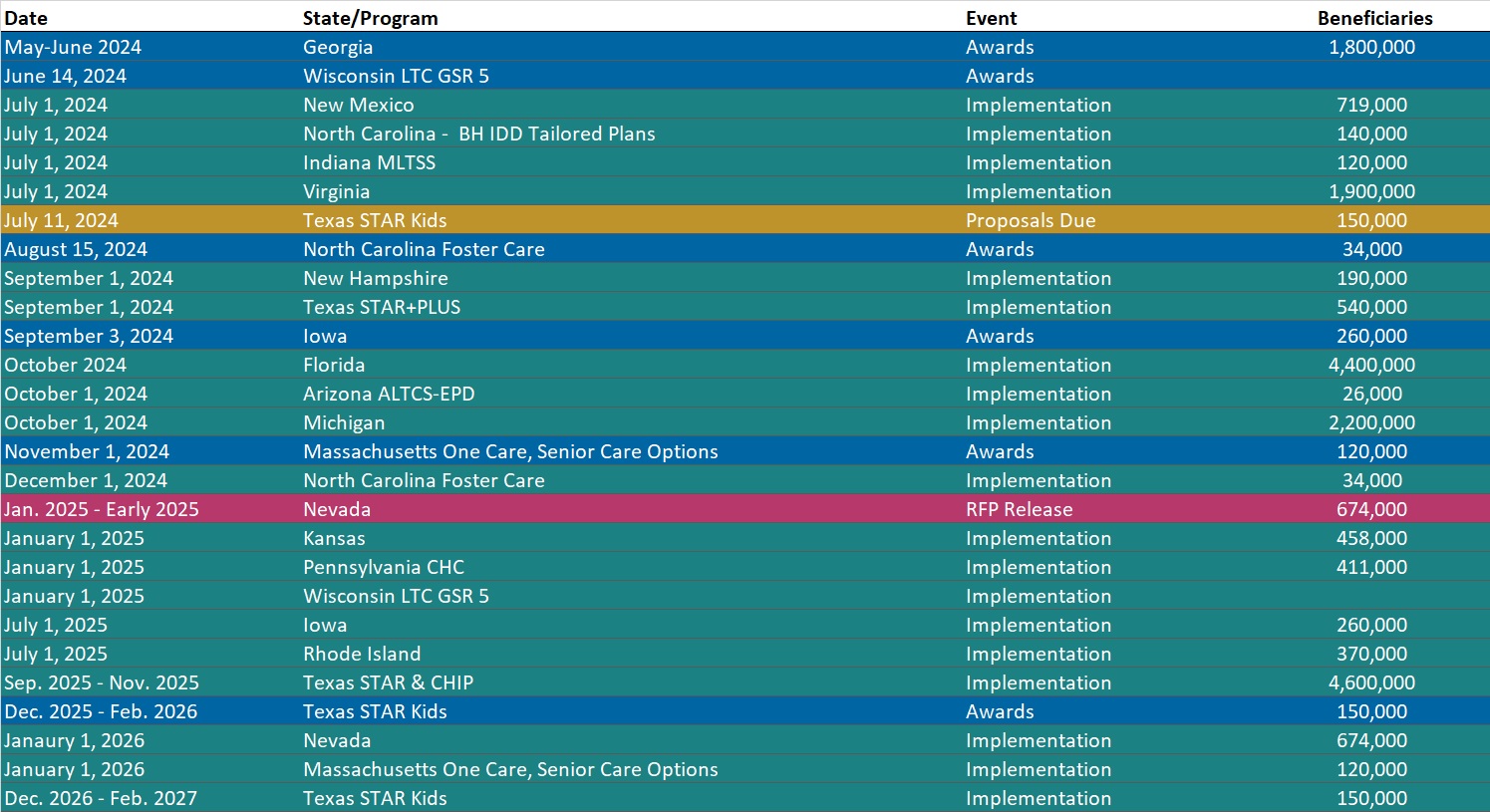
Texas Releases STAR Kids RFP. The Texas Health and Human Services Commission released on May 10, 2024, a request for proposals (RFP) for the STAR Kids program, which provides Medicaid managed care to approximately 150,000 children and youth under age 21 with disabilities who receive supplemental security income. Texas plans to award contracts to at least two plans for each service area (SA), and each MCO can be awarded up to six SAs. Contracts will run for six years with three two-year renewal options. Incumbents are CVS/Aetna, Elevance/Amerigroup, Blue Cross Blue Shield of Texas, Centene/Superior Health Plan, Community First Health Plan, Cook Children’s Health Plan, Driscoll Children’s Health Plan, Texas Children’s Health Plan, and UnitedHealthcare. Prior contracts were worth an estimated $4 billion annually. Proposals are due July 11, with awards expected between December 2025 and February 2026. The contract start date is anticipated to begin between December 2026 and February 2027.
MCOs will need to describe reimbursement strategies that incentivize high-quality and cost-effective health care, while controlling spending and reducing ineffective service utilization, in their proposals. MCOs will provide a proposed Alternative Payment Model and a way to track its effectiveness. This includes implementing processes to support and incentivize providers to implement value-based care models and reward the high-performing providers. Read More
Utah
University of Utah Health Plans Introduces New CHIP Plan Offering. The University of Utah Health Plans announced on May 9, 2024, that it is launching Healthy U CHIP, a new Children’s Health Insurance Program plan which will be available starting July 1 in Utah. Utah does not have a competitive Medicaid managed care procurement process. Read More
Vermont
Vermont Submits Section 1115 Global Commitment to Health Demonstration Amendment. The Centers for Medicare & Medicaid Services announced on May 14, 2024, that Vermont has submitted an amendment request for its Section 1115 Global Commitment to Health demonstration. The amendment aims to expand access to care for individuals with mental health conditions and substance use disorder, provide housing and other supports to promote whole-person health, and advance payment and delivery reforms. The public comment period will be open through June 13. Read More
Legislature Passes Prior Authorization, Step Therapy Bill, Strips Medicaid Expansion Bill. The Vermont Digger reported on May 10, 2024, that lawmakers plan to include a budget provision to increase the state’s income threshold for the Medicare Savings Programs, which provides subsidies to help low-income Vermonters who are 65 and older pay for Medicare. Lawmakers were originally considering broader eligibility expansion policies. Another bill, which passed the General Assembly, would reduce private insurers’ ability to influence a clinician’s care decisions. The bill, HB 766, modifies the timeframes within which health plans must respond to prior authorization requests, requires health plans to grant exceptions to prescription drug step-therapy requirements under certain circumstances, and prohibits prior authorization requirements for generic medications. The bill awaits the governor’s signature. Read More
National
CMS Extends Medicaid Unwinding-related Waiver Demonstrations to June 2025. Modern Healthcare reported on May 10, 2024, that the Centers for Medicare & Medicaid Services (CMS) has extended COVID-19 related Medicaid unwinding flexibilities to June 2025. The extension aims to ensure that eligible individuals retain coverage while states continue redeterminations. States will be permitted to continue flexibilities such as accessing income and residency information from other government agencies; permitting Medicaid managed care contractors to assist members with coverage renewals; and retroactively restoring coverage to people erroneously disenrolled. Read More
DOJ Creates Antitrust Task Force to Combat Healthcare Consolidations, Acquisitions Violating Laws. The Department of Justice announced on May 9, 2024, that it has created an Antitrust Division’s Task Force on Health Care Monopolies and Collusion (HCMC), which aims to oversee issues regarding mergers and acquisitions, payer-provider consolidations, quality of care, medical billing, health care IT services, and health care data access. The HCMC task force will include civil and criminal prosecutors, healthcare economists, data scientists, and policy advisors. Patients, providers, and other members of the public can submit concerns. Read More
U.S. Lawmakers Introduce Bill for Medicaid-covered Doulas. 19th News reported on May 10, 2024, that Senator Elizabeth Warren (D-MA) and Representative Gwen Moore (D-WI) have introduced a bill called the Mamas First Act, which would allow Medicaid coverage for doulas, midwives, and tribal midwives. The legislation aims to fill in widening gaps in obstetric care and reduce the disparate health outcomes for underserved communities. Twelve states and Washington D.C. have already implemented Medicaid-covered doula care. Warren previously introduced the bill in 2022. Read More
CMS Proposes Model to Increase Kidney Transplant Access For Individuals with ESRD. The Centers for Medicare & Medicaid Services (CMS) announced on May 8, 2024, a proposed rule for the Increasing Organ Transplant Access (IOTA) Model, which aims to increase access to kidney transplants for all people living with end-stage renal disease (ESRD) while also reducing Medicare expenditures. CMS plans to select approximately half of the donation service areas (DSAs) and all eligible kidney transplant hospitals in those DSAs to participate in the mandatory model. Model participants would be evaluated by increases in the number of transplants, increased organ acceptance rates, and post-transplant outcomes. If approved, the model will begin January 1, 2025. Read More
Industry News
Federal Court Drops Private Equity Firm from FTC Lawsuit Against U.S. Anesthesia Partners. Modern Healthcare reported on May 15, 2024, that the U.S. District Court for the Southern District of Texas removed private equity firm Welsh, Carson, Anderson & Stowe from the Federal Trade Commission (FTC) lawsuit against U.S. Anesthesia Partners. The FTC initially filed the lawsuit in September alleging that the private equity firm and U.S. Anesthesia Partners consolidated practices in Texas, inflated the cost of care for patients, and engaged in deals to prevent other competitors from entering the market. While the lawsuit against the firm was dismissed due to lack of evidence, the suit against U.S. Anesthesia Partners will continue on the basis that the provider may have violated antitrust laws. Read More
Humana Names Jim Rechtin President, CEO Effective July 1. Humana announced on May 13, 2024, that Jim Rechtin will assume the role of president and chief executive effective July 1, 2024, as part of a planned transition. Humana’s current chief executive, Bruce Broussard, will resign from the Humana Board of Directors effective July 1, 2024, and will serve as a strategic advisor through 2026. Rechtin is currently the chief operating officer. Read More
Eventus WholeHealth Acquires Premier Geriatric Solutions. Eventus WholeHealth announced on May 3, 2024, its acquisition of Virginia-based Premier Geriatric Solutions, which provides value-based medical directorships, and primary care and behavioral health services. The combined entities will form a merged multispecialty group practice, as Eventus, to provide integrated primary care, specialty care, and behavioral health services to more than 44,000 patients in long-term care facilities. Read More
Steward Healthcare to Sell All Hospital Operations Amid Bankruptcy Filing. Modern Healthcare reported on May 8, 2024, that Texas-based Steward Health Care plans to sell all 31 of its hospitals as part its Chapter 11 bankruptcy filing. Steward operates in eight states including Arizona, Arkansas, Florida, Louisiana, Massachusetts, Ohio, Pennsylvania, and Texas. Read More
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Kansas Medicaid Beneficiaries and Expenditures by Population Group, FY 2015-24
- Minnesota Medicaid Managed Care Enrollment is Down 13.4%, May-24 Data
- Mississippi Medicaid Managed Care Enrollment is Up 3.9%, Apr-24 Data
- North Carolina Medicaid Managed Care Enrollment is Up 2%, Jan-24 Data
- Oregon Medicaid Managed Care Enrollment is Flat, Jan-24 Data
- South Carolina Medicaid Managed Care Enrollment is Flat, Jan-24 Data
- South Carolina Dual Demo Enrollment is Down 6.3%, Jan-24 Data
- Virginia Medicaid Managed Care Enrollment is Flat, Feb-24 Data
- Virginia Medicaid MLTSS Enrollment is Flat, Feb-24 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Colorado Accountable Care Collaborative Phase III RFP, May-24
- Colorado Behavioral Health Administrative Service Organizations RFP, May-24
- New York MRT Health Home Supportive Housing Program RFA, May-24
- Texas STAR Kids Managed Care RFP, May-24
Medicaid Program Reports, Data, and Updates:
- Arizona AHCCCS External Quality Review Annual Reports, 2023
- Arizona HCBS Annual Report, CYE 2023
- California Governor’s Proposed Budget, FY 2025
- California HHS OIG Medicaid Eligibility Actions During Unwinding Period Audit, May-24
- Connecticut Managed Care Report, CY 2023
- Updated Florida State Overview
- Georgia Medicaid External Quality Review Reports and CMO Compliance Reports, 2017-23
- Illinois Medicaid Annual Reports, 2013-23
- Illinois Medical Programs External Quality Review Annual Reports, FY 2012-23
- Indiana Medicaid Financial Report, Feb-24
- Kansas Medical Care Advisory Committee Meeting Materials, 2019-23
- Mississippi PHE Medicaid Redeterminations Monthly Reports to CMS, Feb-24
- New Mexico Medicaid NFLOC Services Capitated Payment Audit Report, May-24
- Updated New Mexico State Overview
- Texas Initiatives to Reduce Avoidable Emergency Room Utilization and Improve Health Outcomes in Medicaid Reports, 2022-24
- Vermont Global Commitment to Health 1115 Waiver Documents, 2015-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
