HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- Interoperability and Patient Access Final Rule: The Next Phase in the Data Exchange Journey

- HMA Keynote Speakers Preview Themes, Imperatives for March 5-6 Value Based Care Workshop

- Arizona Releases Housing, Health Opportunities Services Program Administrator RFP

- Arizona Selects 57 Providers to Extend Medicaid Services to Incarcerated Individuals Prior to Release

- Connecticut Governor Calls for Increased Hospital, Pharmaceutical Oversight in Fiscal 2025 Spending Plan

- Florida Announces Intent to Award Florida Community Care Comprehensive IDD Managed Care Pilot Program Contract

- Georgia Governor’s Budget Proposal Increases Health Services Spending by $485 Million

- Kansas Governor Proposes $23 Million for IDD, Physical Disability Waiver Waitlists

- Minnesota Announces $8 Million RFP for Live Well At Home Program

- Mississippi Medicaid Requesting $83 Million Increase in State Support in Fiscal 2025

- Montana Grant Program to Increase Residential Bed Capacity for Individuals with SMI, Developmental Disability

- Pennsylvania Extends Medicaid to Cover Perinatal Doula Care

- Oregon Receives Federal Approval for HRSN Benefits Framework Under Section 1115 Waiver

- HHS Partners with Eight States, District of Columbia to Address Homelessness

- States Continue to Impose Regulations Around Prior Authorization Practices

- BCBS-LA Withdraws from Planned Merger with Elevance

- KKR to Buy Stake in Cotiviti from Veritas Capital

In Focus
Interoperability and Patient Access Final Rule: The Next Phase in the Data Exchange Journey
This week, our In Focus section reviews the Centers for Medicare & Medicaid Services (CMS) Interoperability and Prior Authorization Final Rule, published on January 17, 2024. This is CMS’s latest effort to flesh out regulations mandating payer interoperability and fully electronic prior authorization (PA) policies. The 2024 final rule also represents a new phase in the agency’s work to advance interoperability as it moves beyond policymaking focused on building interoperable systems to policies centered on the applications and usage of shared data.
The new requirements affect a large segment of the nation’s public health insurance programs, including Medicare Advantage (MA) organizations, state Medicaid fee-for-service (FFS) programs, state Children’s Health Insurance Program (CHIP) FFS programs, Medicaid managed care plans, CHIP managed care organizations, and qualified health plan (QHP) issuers on the federally facilitated exchanges (FFEs). These payers must implement and adhere to Health Level 7® (HL7®) Fast Healthcare Interoperability Resources® (FHIR®) application programming interfaces (APIs). These APIs were developed by the DaVinci project and the CARIN Alliance which are both HL7 FHIR accelerator programs. Leavitt Partners, an HMA company, leads the work of the CARIN Alliance.
The final rule demonstrates a commitment to information sharing across the industry landscape and confidence in the FHIR standard to support health data exchange across all required APIs. Ultimately, FHIR APIs are creating a more patient-centered data ecosystem that can provide a tangible return on investment.
Following are details about the requirements, opportunities, and next steps for stakeholders.
Prior Authorization API and Process
Payers must build and maintain PA APIs by January 1, 2027, allowing providers to ask payers whether PA is required for a patient’s procedure, what documents must be submitted to attain authorization, and to receive the final decision and reason for denied requests electronically within a specified timeframe (seven days for standard procedures and three days for expedited decisions).
The rule finalizes requirements for the PA process, regardless of whether the payer receives the PA request through the Prior Authorization API. Specifically, CMS is requiring that:
- Affected payers send notices to providers when they make a prior authorization decision, including a specific reason for denial when they deny a PA request
- Payers, other than QHP issuers on the FFEs, respond to prior authorization requests within specific timeframes
- Affected payers publicly report certain metrics about their PA processes
These prior authorization process requirements become effective January 1, 2026. The last 12 months of PA information also must be shared with patient, providers, and other payers when the member switches a plan through the respective APIs.
To promote adoption of electronic prior authorization processes, CMS is adding an Electronic Prior Authorization measure for Medicare clinicians who participate in the Merit-based Incentive Payment System (MIPS) and hospitals and critical access hospitals in the Medicare Promoting Interoperability Program as an attestation measure.
Payer to Payer FHIR API
To support continuity of care and value-based programs, payers must be able to send, receive, and incorporate enrolled member data from previous and concurrent payers if members are dually enrolled.
To comply with the new electronic data sharing, the final rule requires payers to build and use FHIR API by January 1, 2027. Payer-to-payer (P2P) data sharing will include the last five years of claims/encounters, clinical data, and the active and pending PA requests. The data collected through the P2P APIs will need to be available to the other APIs (i.e., provider, patient, and prior authorization). The rule requires payers to request data from previous payers within a week after the patient opts in to sharing data. For dually enrolled members, data sharing will incur at least quarterly.
Patients must opt in and agree to the P2P data sharing. To this end, health plans must adjust their enrollment administrative process to allow members to easily share previous and concurrent payer information and consent to data sharing. CMS allows Medicaid or CHIP agencies to contract with entities, such as Health Information Exchanges (HIEs), for the digital access and transfer of a patient’s medical records, which supports the Payer-to-Payer API.
Provider Access FHIR API
Payers also must build and maintain a Provider Access API to share patient data with in-network providers with whom the patient has a treatment relationship, enabling continuity and coordination of care, by January 1, 2027. Affected payers must maintain an attribution process to associate patients with the appropriate in-network providers responsible for the patient care. The data from the payer via the Provider Access API must be added to a provider’s electronic health record, practice management solution, or any other technology solution that a provider uses for treatment purposes.
The Provider Access API includes the same data covered in the Payer to Payer Access API (claims/encounters, clinical data, and prior authorizations). The payer has one business day to deliver the required information. Payers must offer a mechanism for members to opt out from making their data available to the attributed providers.
Patient Access FHIR API
The final rule further enhances patient access to data to improve their treatment and shopping experience. In addition to claims and clinical data, as of January 1, 2027, payers must make PA data available through the Patient Access API to inform patients on their plan’s PA process and the status of requests.
In addition, affected payers must report annual metrics about Patient Access API usage and data requests to CMS beginning January 1, 2026.
Key Considerations and Early Results
The rule presents a significant opportunity to improve patient experiences and outcomes and to address some of the administrative burden on clinicians. Though CMS made some adjustments to timeframes in the proposed rule, immediate attention is needed to evaluate technological solutions available to payers, assess gaps between current and future required state, and develop policies to comply with new requirements and measures reporting.
Commercial payers may also leverage the improved electronic data sharing but are not required to do so. CMS-funded payers must respond to any inquiries from commercial payers and must require commercial payers to provide the same information as affected payers. Commercial payers, state governments, and other stakeholders have an opportunity to collaborate around the electronic data exchange.
This rule may have positive downstream application to other areas beyond PA, including quality measurements, risk adjustment, and population health. Early adopters who have implemented the prior authorization APIs have, on average, recorded a 150% – 300% return on investment (ROI). The implementation of API-based prior authorization represents a demonstrable increase in efficiency and significantly reduced provider burden. Given the measurable ROI, state-based regional collaboratives being led by Leavitt Partners are forming between payers and providers to implement the core tenants of the CMS rule well in advance of the 2027 deadline.
Similar initiatives are taking place in the technology space, like the Digital Quality Implementers Community, which was recently convened by Leavitt Partners and National Committee for Quality Assurance (NCQA) to build industry readiness for transitioning to FHIR-based digital measurement that hinges on improved electronic data sharing
What to Watch
The HMA team will continue to analyze the CMS’s Interoperability and Patient Access rule in the context of other federal and state policy changes affecting MA organizations, Medicaid FFS programs, state CHIP FFS programs, Medicaid and CHIP managed care programs, and QHPs.
The work and opportunities afforded with the Interoperability and Patient Access final rule will be featured prominently at The HMA Spring Workshop: Getting Real About Transforming Healthcare Quality and Value, March 5-6. In addition to rich discussions, HMA and HMA companies, including Leavitt Partners and Wakely Consulting LLC, are available to support planning and implementation and related system redesign initiatives. If you have questions about these topics, contact Ryan Howells ([email protected]) and Daniela Simpson ([email protected]).
HMA Keynote Speakers Preview Themes, Imperatives for March 5-6 Value Based Care Workshop
HMA’s Spring Workshop on Value-Based Care, March 5-6 in Chicago, is just a few weeks away. Listen to why our speakers are so excited to engage with attendees on value-based care.
Elizabeth Mitchell, CEO, Purchaser Business Group on Health will deliver the keynote speech on “The Purchaser’s Dilemma: Why Employers Should Demand Value (and Why They Don’t).”
Our March 5 dinner headliner Katie Kaney, CEO of LovEvolve will discuss her “Whole Person Index” and how we can collaborate in new ways to transform the healthcare system to deliver better health at a lower cost for all.
Hurry – online registration ends February 28!
Register here.
HMA Roundup
Arizona
Arizona Releases Housing, Health Opportunities Services Program Administrator RFP. The Arizona Health Care Cost Containment System released on February 1, 2024, a request for proposals (RFP) for a Housing and Health Opportunities (H2O) Program Administrator. The H2O waiver demonstration, scheduled to go-live on October 1, 2024, is aimed at expanding housing services for Medicaid beneficiaries who are homeless or at risk of becoming homeless. The contract will run for three years with two one-year renewal options. Intent to bid is due April 1, with proposals due May 1. The anticipated award date is July 1 and implementation is set for October 1. Read More
Arizona Selects 57 Providers to Extend Medicaid Services to Incarcerated Individuals Prior to Release. The Arizona Health Care Cost Containment System announced on February 6, 2024, that it has selected 57 health care providers to receive incentive payments as part of a five-year program aimed at increasing physical and behavioral health services for Medicaid-eligible individuals transitioning from incarceration. The selected providers will create co-located, integrated clinics with prioritized appointments for those with complex health conditions. Read More
Arizona Releases External Quality Review Organization RFP. Arizona Healthcare Cost Containment System released on February 7, 2024, a request for proposals (RFP) for an external quality review organization (EQRO) for the state’s Medicaid managed care organizations. The contractor will be required to produce annual technical reports and ensure state compliance with federal rules. The state may award one vendor contract for each mandatory EQRO activity or it may award multiple activities to a single vendor. The contract will run for three years with two one-year renewal options, not to exceed a total of five years. The current EQRO contract is held by Health Services Advisory Group. Intent to bid is due March 4, with proposals due on March 28. Awards will be announced June 1, and the contract implementation will begin August 1. Read More
Connecticut
Connecticut Governor Calls for Increased Hospital, Pharmaceutical Oversight in Fiscal 2025 Spending Plan. The CT Mirror reported on February 7, 2024, that Connecticut Governor Ned Lamont focused on oversight of hospitals, nursing homes, and pharmaceutical companies in his plan for the 2025 fiscal year, which starts July 1. The Governor also proposed transitioning some residents from the Medicaid program to free coverage provided through Connecticut’s health insurance exchange, along with allocating $627,000 to create four new positions in the state’s Office of Health Strategy. The positions would focus on financial monitoring of hospitals, monitoring policies around prescription drug affordability, and overseeing performance improvement plans for providers exceeding the state’s cost growth benchmarks. Read More
Florida
Florida Announces Intent to Award Florida Community Care Comprehensive IDD Managed Care Pilot Program Contract. Florida Politics reported on February 12, 2024, that the Florida Agency for Health Care Administration has announced its intent to award a six-year contract to Florida Community Care to transfer the state’s home and community-based services for the intellectual and developmental disabilities (IDD) population to a pilot program for long-term care plans participating in the Statewide Medicaid Managed Care (SMMC) program. These services currently utilize a fee-for-service reimbursement system through the Developmental Disabilities Individual Budgeting waiver. The initial phase will enroll up to 600 individuals in SMMC regions D and I and will run from the execution date in 2024 through September 30, 2030. Elevance/Simply Healthcare was the only other respondent to the Invitation to Negotiate. Read More
Florida House Considers Bill to Allow Hospital Districts to Convert to Nonprofit Organizations. Health News Florida reported on February 8, 2024, that the Florida House Select Committee on Health Innovation approved a bill, sponsored by Representative Randy Fine (R-Brevard County), that would permit public hospital districts to convert to non-profit organizations. The bill would also require districts to analyze the financial feasibility of converting to nonprofits or selling to for-profit companies. The bill now heads to the State Affairs Committee. A Senate version of the bill was filed but has not been reviewed in committees. Read More
Georgia
Georgia Partners With HOPE for Georgia Moms to Provide Community Grants. Valdosta Today reported on February 13, 2024, that Georgia is partnering with HOPE for Georgia Moms at Northeast Georgia Health System to provide $60,000 in community mini-grants aimed at improving Medicaid redetermination awareness. The state will award up to five organizations grants to place ads in local papers, staff local outreach, or host an event through May 31, 2024. Eligible organizations can apply for one grant, a combination of grants, or all grants offered, up to a total amount of $12,000. Applications are due by February 21. Read More
Governor’s Budget Proposal Increases Health Services Spending by $485 Million. The Georgia Budget and Policy Institute reported on February 7, 2024, that Georgia Governor Brian Kemp’s fiscal 2025 proposed budget provides the Department of Community Health with $5.2 billion in state funds, an increase of $485 million. The proposed budget calls for raising Medicaid reimbursement for home and community-based services. It also includes a $273 million increase to replace the end of the increased federal Medicaid funding that was tied to the COVID pandemic and a $118 million increase to reflect 2021 cost reports for skilled nursing centers that serve Medicaid enrollees requiring long-term care. Read More
Georgia Disenrolls 550,444 Medicaid Beneficiaries During Redeterminations From May Through January. The Georgia Department of Community Health released data on February 12, 2024, showing that it has disenrolled 550,444 Medicaid beneficiaries during redeterminations from May through January. Of those, 468,110 were due to procedural reasons. The state renewed coverage for 543,967 beneficiaries, and has nearly 1.5 million pending eligibility cases. Read More
Indiana
Indiana to Resume Premiums, Cost-sharing for Medicaid Expansion Beneficiaries Beginning July 1. WBOI reported on February 8, 2024, that Indiana Medicaid expansion beneficiaries will be required to resume premiums and participate in cost-sharing via POWER account contributions beginning July 1, following a long-term pause due to the pandemic. POWER Account contributions are mandatory for beneficiaries receiving HIP Plus, a plan which includes additional benefits. HIP Basic has co-payments for some services. The Indiana Family and Social Services Administration has indicated that it will collaborate with managed care entities and various stakeholders to inform beneficiaries of the return of cost-sharing 60 days before payments resume. Read More
Kansas
Kansas Governor Proposes $23 Million for IDD, Physical Disability Waiver Waitlists. Kansas Reflector reported on February 7, 2024, that Kansas Governor Laura Kelly has proposed to allocate over $23 million in the fiscal year 2025 budget amendment, aimed at lowering the intellectual and developmental disability (IDD) services and the physical disability services waitlists. The IDD waitlist is at 5,187 people, and the physical disability list is at 2,361, as of December. The funding is expected to take 250 individuals off each waitlist. Read More
Kentucky
Kentucky House Approves Fiscal 2025 Budget Cutting $139 Million Medicaid Funds. Kentucky Lantern reported on February 13, 2024, that the Kentucky House approved a budget proposal cutting about $139 million in state funds for Medicaid in fiscal 2025. The budget will now go to the Senate Appropriations and Revenue Committee, and a hearing will be held with lawmakers seeking to reinstate those funds into the budget. Read More
Maine
Maine Proposed Supplemental Budget Includes $30 Million For Behavioral Health Initiatives. The Maine Department of Health and Human Services announced on February 14, 2024, that the Governor’s supplemental budget proposal includes $30 million in proposed investments aimed at strengthening the state’s behavioral health system. The investments will support mental health and substance use disorder services, individuals in crisis, children in state custody, and initiatives to advance violence prevention and public safety. Read More
Minnesota
Minnesota Announces $8 Million RFP for Live Well At Home Program. The Minnesota Department of Human Services Aging and Disability Services Division released on February 12, 2024, a Request for Proposals (RFP) for vendors to develop and/or provide services for the state’s Live Well at Home program which allows older Minnesotans to live in the community. Approximately $8 million will be available to awardees in fiscal 2025, with the individual annual maximum grant award being $350,000. Eligible projects include capital and renovation to enhance accessibility in homes or buildings and long-term services and supports development. The term of the contract will be for six to twenty-four months with up to five renewal years. Proposals are due April 5, and contract implementation is July 1, 2024. Read More
Mississippi
Mississippi Medicaid Requesting $83 Million Increase in State Support in Fiscal 2025. The Mongolia Tribune reported on February 8, 2024, that the Mississippi Division of Medicaid (DOM) is requesting $992 million in state support in fiscal 2025, an increase of $83 million, or nine percent, since last year. The increase is due to a lower than expected Federal Medicaid Assistance Percentage projection and a higher than expected utilization rate. DOM estimated that the state support request could reach $1.45 billion in fiscal 2026. Read More
Montana
Montana Grant Program to Increase Residential Bed Capacity for Individuals with SMI, Developmental Disability. The Montana Department of Public Health and Human Services announced on February 6, 2024, that it has launched a $10 million grant program aimed at increasing residential bed capacity for congregate living facilities serving individuals with a serious mental illness (SMI) or developmental disability diagnosis. The grant is provided through a $300 million Behavioral Health System for Future Generations investment to expand behavioral health care and developmental disabilities services. Funding proposals must be submitted by March 8. Read More
Nebraska
Nebraska Senate Committee Advances Bill to Expand Medicaid Prenatal Care Reimbursement. The Nebraska Examiner reported on February 8, 2024, that the Nebraska Senate Health and Human Services Committee advanced a bill, sponsored by Senator George Dungan (D-Lincoln), that would establish the Nebraska Prenatal Plus Program. The program, aimed at at-risk mothers who are Medicaid recipients, not Children’s Health Insurance Program recipients, would expand Medicaid reimbursements for prenatal care to include nutrition counseling and targeted case management beginning six months prior to birth. The program would be funded through the Medicaid Managed Care Excess Profit fund. The bill will next be reviewed by the Senate floor. Read More
Senate Advances Bill to Increase Medicaid Dental Reimbursement. The Unicameral Update reported on February 8, 2024, that the Nebraska Senate approved a bill, sponsored by Senator Lynne Walz (D-Fremont), that would increase reimbursement rates for dental services covered by Medicaid by 25 percent. Read More
Nevada
Nevada Market Stabilization, Public Option Federal Public Comment Period Opens. The Nevada Division of Health Care Financing and Policy announced on February 13, 2024, that the Centers for Medicare & Medicaid Services (CMS) and the Department of the Treasury have determined Nevada’s Section 1332 state innovation waiver application complete and have opened a federal public comment period that will run until March 14. The waiver aims to establish a market stabilization program and a new public option program. The waiver would also create an annual bonus payment program for health insurance carriers that improve health outcomes and quality of care and a loan repayment program to support health care providers committed to practicing in the state for at least four years. Read More
North Carolina
North Carolina Launches Behavioral Health Dashboard for Children. The Winston-Salem Journal reported on February 12, 2024, that the North Carolina Department of Health launched a child behavioral health dashboard to provide behavioral health data on children living in seven different regions in the state. The dashboard, which includes data beginning in 2017, includes statistics on diagnoses for conditions such as depression and ADHD as well as breakdowns by demographics. Read More
Oregon
Oregon Receives Federal Approval for HRSN Benefits Framework Under Section 1115 Waiver. The Centers for Medicare & Medicaid Services (CMS) approved on February 1, 2024, Oregon’s structure for how health-related social needs (HRSN) benefits will be delivered under the state’s Section 1115 Medicaid waiver demonstration. The protocol, effective through September 30, 2027, provides detailed requirements for the state’s HRSN services including member eligibility, the process for identifying eligible individuals, and provider qualifications. Read More
Pennsylvania
Pennsylvania Extends Medicaid to Cover Perinatal Doula Care. WHYY reported on February 11, 2024, that Pennsylvania’s Medicaid program now permits certified perinatal doulas to partner with managed care organizations to offer in-network maternity care services, effective February 1. Read More
South Dakota
South Dakota Projects Decreased Medicaid Expansion Enrollment. South Dakota Public Broadcasting reported on February 13, 2024, that the South Dakota Department of Social Services has lowered its projected monthly Medicaid expansion enrollment from an average of 57,000 to 40,000 due to lower than expected enrollment in the expansion program. South Dakota approved Medicaid expansion in 2022. Read More.
Texas
Texas Disenrolls 44,042 Medicaid Beneficiaries During January Redeterminations. The Texas Health and Human Services Commission announced on February 8, 2024, that the state disenrolled 44,042 Medicaid beneficiaries during January redeterminations, including 24,911 due to procedural reasons and 19,131 due to ineligibility. Read More
West Virginia
West Virginia House Considers Bill to Establish Buy-in Medicaid Program. Lootpress reported on February 14, 2024, that West Virginia House Delegates Amy Summers (R-Taylor) and Heather Tully (R-Nicholas) sponsored a bill that would establish a buy-in program for residents to obtain affordable Medicaid coverage. The bill would require the West Virginia Bureau of Medical Services to apply for a Basic Health Plan Option or a State Innovation Waiver. The bill has been referred to the House Committee on Health and Human Resources. Read More.
National
CMS Releases QI Tools For Behavioral Health Follow Up Care. The Centers for Medicare & Medicaid Services (CMS) announced on February 13, 2024, that it is releasing a set of quality improvement (QI) tools aimed at helping states improve behavioral health follow-up care. The tools include a driver diagram/change ideas table, a measurement strategy, and a highlights brief that gives an overview of state projects completed as part of the Improving Behavioral Health Follow-up Care Affinity Group. Read More
HHS Partners with Eight States, District of Columbia to Address Homelessness. The Department of Health and Human Services (HHS) announced on February 9, 2024, that eight states and the District of Columbia have been selected to participate in the Housing and Services Partnership Accelerator, a federal initiative intended to reduce homelessness by providing states with resources to address health-related social needs and housing-related services. The selected states, Arizona, California, Hawaii, Maryland, Massachusetts, Minnesota, North Carolina, and Washington, and the District of Columbia, will receive technical assistance to support implementing housing-related services for people with complex health needs over the next 12 months. Read More
Medicare Advantage D-SNP Enrollment, Availability Grows, KFF Reports. KFF reported on February 9, 2024, that the number of Medicare and Medicaid dual-eligible individuals enrolled in dual-eligible special needs plans (D-SNPs) increased from 11 percent to 29 percent between 2010 and 2021. In 2022, there was an average of 10 D-SNPs offered per dual-eligible individual, compared to 6 plans in 2018. The share of dual-eligible individuals enrolled in D-SNPs by state ranged from 5 percent to 58 percent in 2021. Despite fewer prior authorizations in D-SNP-only plans compared to all Medicare Advantage plans, the rate of denials was twice as high. Read More
CMS Proposes Rule to Increase Regulations for Accrediting Organizations. Modern Healthcare reported on February 9, 2024, that the Centers for Medicare & Medicaid Services (CMS) have proposed a rule to increase oversight and regulations for the nine accrediting organizations approved to survey and accredit Medicare-certified facilities. Under the proposed rule the organizations would be required to standardize survey agency practices and their application process; limit fee-based consulting services; ensure non-bias participation in surveys or related activities; and submit a public correction plan to CMS if the organization is performing poorly. CMS is also asking for feedback on whether to limit the number of times an accrediting organization can submit an incomplete application. Read More
States Continue to Impose Regulations Around Prior Authorization Practices. Modern Healthcare reported on February 9, 2024, that several states are continuing to impose limitations on prior authorization requirements, with more than 20 prior authorization bills enacted in 2023. Approximately 70 additional bills aimed at addressing provider and patient complaints around denied or delayed care are still pending. New Jersey has recently signed legislation requiring insurance companies to process authorizations within 24 hours for urgent services and 72 hours for non-urgent services. Read More
HHS Releases Final Rule to Enhance Confidentiality of Substance Use Disorder Treatment Records, Integrated Care. The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Office of Civil Rights, released on February 8, 2024, a final rule making changes to the Confidentiality of Substance Use Disorder (SUD) Patient Records requirements (Part 2). The changes align certain aspects of Part 2 with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Rules and the Health Information Technology for Economic and Clinical Health Act (HITECH). The modifications are intended to strengthen privacy protections for patients’ substance use disorder (SUD) treatment records, increase coordination among providers treating patients for SUDs, and improve integration of behavioral health information with other medical records. Read More
Industry News
BCBS-LA Withdraws from Planned Merger with Elevance. The Louisiana Department of Insurance (LDI) announced on February 14, 2024, that Blue Cross Blue Shield of Louisiana (BCBS-LA) withdrew from its planned merger with Elevance. Anticipated LDI hearings regarding the merger have been cancelled. Read More
CareOregon, SCAN Drop Planned Merger. Willamette Week reported on February 13, 2024, that CareOregon, the state’s largest Medicaid insurer, and SCAN Group of California jointly terminated their merger. The merger faced criticism from an independent oversight panel and public comments revealed concerns. Read More
KKR to Buy Stake in Cotiviti from Veritas Capital. Healthcare software company Cotiviti, a subsidiary of Veritas Capital, announced on February 14, 2024, that it has entered into a definitive agreement with private equity firm KKR & Co, allowing KKR to acquire a stake in the company. Under the agreement, KKR and Veritas will become co-sponsors with equal ownership stakes in Cotiviti. Read More
Varsity Healthcare Partners Completes Sale of Angels of Care. Varsity Healthcare Partners (VHP) announced on February 13, 2024, the completion of its sale of Angels of Care (AOC), a provider of home health services for pediatric patients with complex medical conditions, to Nautic Partners. Over the course of its investment, VHP expanded AOC’s service area from two to seven states. Terms of the transaction were not disclosed. Read More
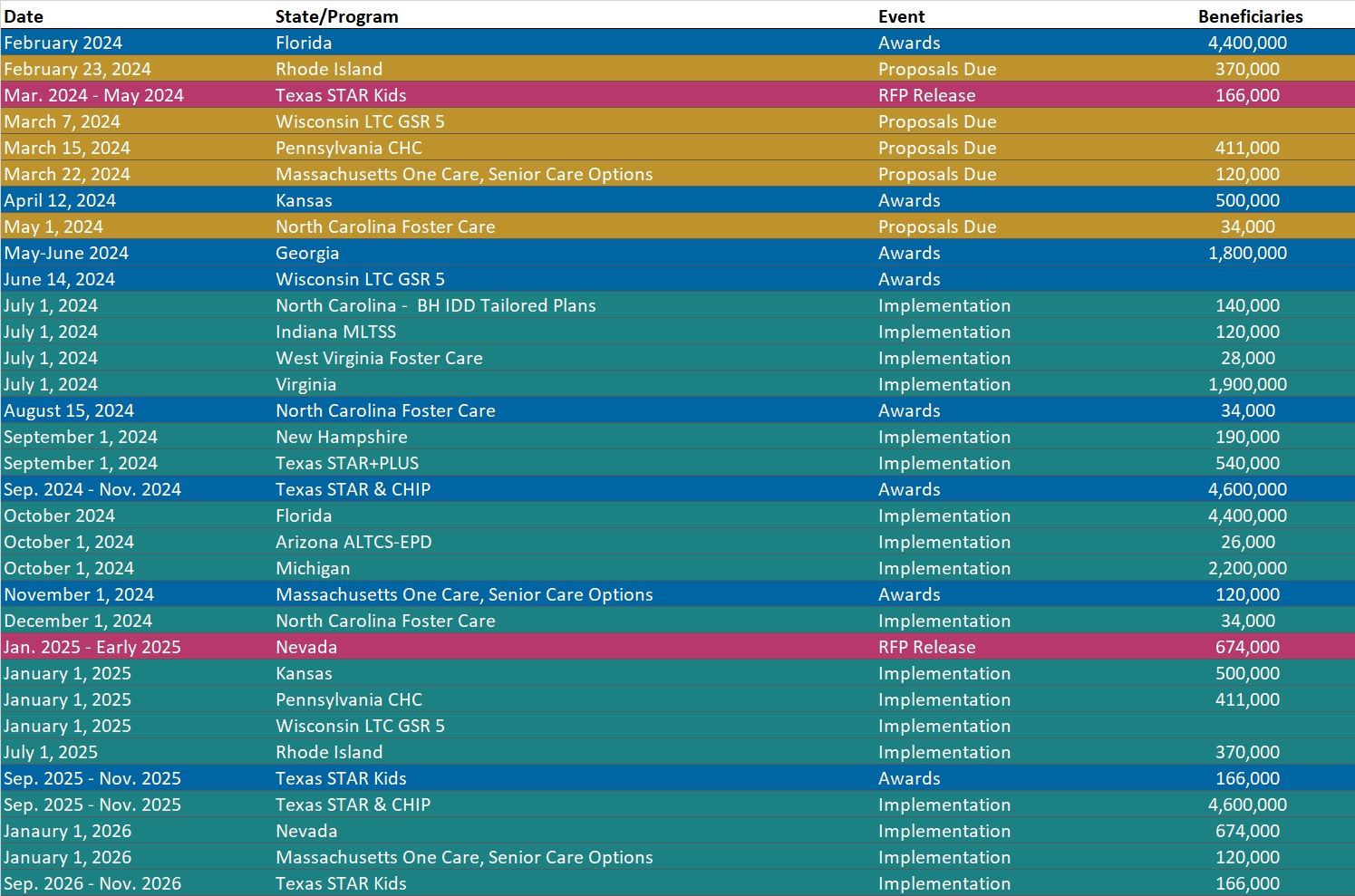
RFP Calendar
HMA News & Events
HMA Webinars:
Substance Use Disorder (SUD) Ecosystem of Care: Pivoting to Save Lives – An Overview. Wednesday, February 28, 2024, 12 PM ET. Join us for part 1 of our 5-part webinar series, “Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives.” This session will introduce overarching themes of the webinar series, including the diverse pathways within the continuum of care and unravel a comprehensive framework that spans prevention, early intervention, treatment, and long-term care. The webinar will also delve into the intricate network of support systems designed to maintain life and resource individuals on their unique recovery journey, examining what is working and what we can leave behind to pivot toward what matters. Register Here
Summary and Implications of the 2025 Medicare Advantage Advance Notice. Wednesday, February 21, 2024, 01:30 PM ET. The Centers for Medicare & Medicaid Services (CMS) recently released the 2025 Advance Notice of Methodological Changes for Medicare Advantage Capitation Rates and Part C/D Payment Policies, which proposes important changes in plan payments, risk adjustment and other key financial and regulatory requirements for 2025. During this webinar, Wakely consultants will provide an overview of the proposed changes, with an emphasis on the likely impact that the new rates and policies will have on Medicare Advantage bids, membership growth, quality and strategy. Speakers will also touch on other recent public statements from federal regulators that could point to additional changes for Medicare Advantage in the future. Register Here
Wakely, an HMA Company, White Papers:
Summary of CY2025 Medicare Advantage Advance Notice. The Wakely Summary of the CY2025 Advance Notice provides a thorough summary of the proposed Medicare Advantage (MA) Part C and Part D payment policies for 2025. The Summary covers implications for the growth rate, risk scores, Part D changes, Star ratings, and overall revenue in CY2025. It also provides critical financial information as plans begin the 2025 Medicare Advantage bid preparation process. Read More
