HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Introduces Advance Notice of Methodological Changes for MA Capitation Rates and Medicare Part C and Part D Payment Policies

- Alaska Releases MMIS RFP California Awards $18 Million in Grants for Student Behavioral Health Center Training

- California Awards $18 Million in Grants for Student Behavioral Health Center Training

- Florida Appoints Ken Kniepmann as Assistant Deputy Secretary for Medicaid Policy and Quality

- Medicaid Expansion News: Florida, Kansas, Mississippi

- Idaho Senate Panel Recommends Focus on Prevention Through Managed Care for Medicaid Expansion Population

- Idaho Delays Award of Behavioral Health Plan Contract Pending Appeals Process

- New York Governor Prioritizes Medicaid Reimbursement Increases, Behavioral Health in Fiscal 2024 Budget

- North Carolina Seeks Waiver Amendment to Extend Medicaid Eligibility to Parents, Caretakers of Children in Foster Care

- North Carolina Announces Retirement of Medicaid Director Dave Richard

- Oklahoma to Apply for Medicaid Managed Care Waiver

- Vermont Releases Technical Assistance for Medicaid Supportive Housing Program RFP

- Federal Judge Rules Against Disenrollment of Medicaid Members Who Are Eligible for Medicare Savings Program

- CMS Officials Aim to Establish Universal Quality Measures Across Programs

- CVS Health to Acquire Oak Street Health

- Carlyle Group Looks to Acquire of Cotiviti from Veritas Capital

In Focus
CMS Introduces Advance Notice of Methodological Changes for MA Capitation Rates and Medicare Part C and Part D Payment Policies
This week, our In Focus section reviews recently announced major policy updates from the Centers for Medicare & Medicaid Services (CMS) that affect the Medicare Advantage (MA) and Part D programs. First, on January 30, CMS released the final Risk Adjustment Data Validation Final Rule, a highly anticipated and controversial policy that establishes the agency’s approach to auditing MA Organizations’ (MAOs) risk-adjustment payments and collecting overpayments as needed.
Then, on February 1, CMS published the Calendar Year (CY) 2024 Advance Notice for the MA (Part C) and Part D Prescription Drug Programs. Between these two directives and the proposed MA policy changes CMS announced in December 2022, the Administration continues its efforts to actively manage Medicare Advantage and strengthen quality and oversight of the program. HMA’s summary of the December 2022 proposed rule is available here.
Below are some highlights of the 2024 Advance Notice. By law, CMS must notify the public of planned changes in the MA capitation rate methodology and risk adjustment methodology annually. The deadline for submitting comments to CMS is Friday, March 3, 2023.
Payment Impact in MA: CMS is projecting an average increase in revenue of 1.09 percent in plan payments from last year. This percentage increase is based on a net number that reflects multiple factors including growth rates, change in STAR ratings, and risk score trends.
Risk Adjustment: CMS is seeking to make some refinements to the Part C risk-adjustment model. For example, CMS will begin using the International Classification of Diseases (ICD)-10 classification system (instead of the ICD-9 classification system) and updated underlying fee for service data years. More specifically, diagnoses data years are being updated from 2014 to 2018, and expenditure years are being updated from 2015 to 2019 to reflect changes in costs.
Star Ratings: CMS is proposing updates and refinements to the Star Ratings program, including:
- Retiring the diabetes care-kidney disease monitoring and Medication Reconciliation Post-Discharge
- Expanding the age range for colorectal cancer screening measure to 45−75 years old to align with the preventive task force
- Adding the Care for Older Adults (COA)—Functional Status Assessment measure back to the Star Ratings, and introducing Kidney Health Evaluation for Patients with Diabetes (KED), Concurrent Use of Opioids and Benzodiazepines (COB), Polypharmacy Use of Multiple Anticholinergic Medications in Older Adults (Poly-ACH), and polypharmacy Use of Multiple Central Nervous System Active Medications in Older Adults (Poly-CNS)
- Introducing a case-mix adjustment to Part D medication adherence measures for diabetes, hypertension, and cholesterol.
CMS also is seeking to potentially align measures with other CMS programs. Specifically, the agency is introducing a “Universal Foundation” of quality measures, which is a core set of metrics aligned across programs. Additional information can be found in this New England Journal of Medicine “Perspective”.
Part D Impact
The Advance Notice also notifies plans on the changes to the Part D benefit occurring in 2024 as a result of the Inflation Reduction Act (IRA), including:
- Beginning in CY 2024, CMS will eliminate cost-sharing for Part D drugs prescribed to beneficiaries in the catastrophic phase of coverage.
- Beginning in CY 2024, the Low-Income Subsidy program (LIS) under Part D will be expanded so that beneficiaries who earn 135−150 percent of the federal poverty level and meet statutory resource limit requirements will receive the full LIS subsidies that were available only to beneficiaries earning less than 135 percent of the federal poverty level prior to 2024.
- During CY 2024, CMS will prohibit Part D plans from applying the deductible to any Part D covered insulin product and from charging more than $35 for each month’s supply of a covered insulin product in the initial coverage phase and the coverage gap phase.
- During CY 2024, CMS will prohibit Part D plans from applying the deductible to an adult vaccine recommended by the Advisory Committee on Immunization Practices and from charging any cost-sharing payments at any point in the benefit for these vaccinations.
- Beginning in CY 2024, CMS will cap the growth in the Base Beneficiary Premium at 6 percent. The Base Beneficiary Premium for Part D is limited to the lesser of a 6 percent annual increase or the amount that would otherwise apply under the prior methodology had the IRA not been enacted.
The HMA Medicare team will continue to analyze these proposed changes. We have the depth and breadth of expertise to assist with tailored analysis, to model policy impacts across the multiple rules, and to support the drafting of comment letters on this notice.
If you have questions about the contents of CMS’s MA advance notice and how it will affect MA plans, providers, and patients, contact Julie Faulhaber ([email protected]), Amy Bassano ([email protected]), or Andrea Maresca ([email protected]).
HMA Roundup
Alabama
Alabama Hospitals Seeks Federal Funding to Prevent Closures. Modern Healthcare reported on February 2, 2023, that the Alabama Hospital Association and hospital administrators are seeking an infusion of federal funding to prevent hospital closures across the state. Half of all hospitals in Alabama finished 2022 with negative operating margins. A spokesperson for the association said the state needs to look at long-term solutions to the problem. Read More
Alaska
Alaska Releases MMIS RFP. The Alaska Department of Health released on February 2, 2023, a request for proposals (RFP) for its Medicaid Management Information System (MMIS), which includes software development services, interfaces, and infrastructure hardware. Proposals are due on April 28, and awards are anticipated on December 1. The contract is set to begin on December 15. Read More
California
California Awards $18 Million in Grants for Student Behavioral Health Center Training. The California Department of Health Care Services (DHCS) announced on February 1, 2023, $18 million in grants for students interested in gaining on-the-job experience in behavioral health careers. DHCS is also providing $4 million in grants to 54 programs aimed at reducing opioid overdoses and opioid-related traffic fatalities. Read More
Florida
Florida Appoints Ken Kniepmann as Assistant Deputy Secretary for Medicaid Policy and Quality. Florida Politics reported on February 6, 2023, that Florida Governor Ron DeSantis appointed Ken Kniepmann as assistant deputy secretary for Medicaid policy and quality, effective January 30, 2023. Kneipmann previously served as associate director for health at the Florida Conference for Catholic Bishops. Read More
Florida Lawmakers Will Not Consider Medicaid Expansion in Special Session. Florida Politics reported on February 6, 2023, that Florida Democrats attempted to add Medicaid expansion to the agenda for the state legislature’s special session this week, but the addition did not pass a voice vote. Read More
Florida Governor Proposes Fiscal 2024 Budget Prioritizing Postpartum Coverage, Behavioral Healthcare. Florida Politics reported on February 2, 2023, that Florida Governor Ron DeSantis’ proposed fiscal 2024 budget called for $143 million to extend Medicaid coverage for pregnant and postpartum women and children to 12 months. The budget proposal also included $531 million for comprehensive behavioral health services and $78.9 million to increase the number of beds at state-operated mental health facilities. Total proposed expenditures across the state’s health and human services-related agencies was $47.5 billion. Read More
Idaho
Idaho Could Reduce Medicaid Spending by $65.7 Million, Consultant Says. The Idaho Capital Sun reported on February 6, 2023, that Idaho could reduce its Medicaid spending by $65.7 million, according to a presentation to state lawmakers from consulting firm Sellers Dorsey. The savings would come from cuts to professional services, hospital spending, adult dental care, provider reimbursements, and other categories. The firm is scheduled to deliver final recommendations in April. Read More
Idaho Senate Panel Recommends Focus on Prevention Through Managed Care for Medicaid Expansion Population. The Lewinston Tribune reported on February 3, 2023, that the Idaho Senate Health and Welfare Committee recommended that the state focus on health and wellness and work with providers to incentivize preventative care through Medicaid managed care in a letter summarizing the committee’s five-year review of the state’s Medicaid expansion program. The recommendations mirrored those of a House committee review, which called for transitioning the expansion population to managed care. The Senate committee also directed the state Department of Health and Welfare to complete the Medicaid redetermination process as quickly as possible, to request federal waivers for Medicaid work requirements, and to allow some eligible individuals to choose between Medicaid and Exchange plans. Read More
Idaho Delays Award of Behavioral Health Plan Contract Pending Appeals Process. Health Payer Specialist reported on February 1, 2023, that Idaho delayed the award of the state’s behavioral health plan contract pending the result of appeals from incumbent UnitedHealth/Optum and Centene/Magellan. The state has announced its intent to award the contract to Elevance/Beacon Health Options. Read More
Idaho House Committee Recommends Transitioning Medicaid Expansion Members to Managed Care. The Idaho Press-Tribune reported on February 1, 2023, that the Idaho House Health and Welfare Committee recommended that the state transition Medicaid expansion beneficiaries to managed care. The proposal was one of six recommendations included in the committee’s five-year review of the state’s expansion program. The committee also recommended that the state disenroll all participants who are no longer eligible for Medicaid by July 1, 2023, and submit a revised budget for the Medicaid program based on the removal of these enrollees. Additionally, the legislators suggested that the Department of Health and Welfare submit a Section 1332 waiver to allow some Medicaid-eligible individuals to enroll in Exchange plans. Read More
Kansas
Kansas Lawmakers Introduce Medicaid Expansion Bills. KZRG reported on February 7, 2023, that Kansas lawmakers introduced Medicaid expansion bills in committees in both the House and Senate. Kansas Governor Laura Kelly has proposed expansion in her fiscal 2024 budget. Read More
Kentucky
Kentucky Awards $10.5 Million to Pilot Program Offering Behavioral Care to Individuals with Substance Use Disorder in Lieu of Incarceration. The Associated Press reported on January 31, 2023, that the Kentucky Opioid Abatement Advisory Commission awarded $10.5 million to a pilot program that will provide behavioral health treatment options for individuals with substance use disorder as an alternative to incarceration. The funding comes from a settlement with opioid companies. Read More
Mississippi
Mississippi Senate Passes Bill to Extend Postpartum Medicaid Coverage from 60 Days to 12 Months. The Associated Press reported on February 7, 2023, that the Mississippi Senate passed a bill to extend postpartum Medicaid coverage from 60 days to 12 months. The bill now heads to the House.
Mississippi Senate Passes Bill to Ease Restrictions on Community-Owned Hospitals. The Associated Press reported on February 3, 2023, that the Mississippi Senate passed a bill that would ease restrictions on community-owned hospitals, including allowing for consolidation or collaboration with health care facilities outside their service areas. The bill is aimed at helping individuals maintain access to health care at a time when hospitals are facing financial difficulties. Fifty-four percent of rural hospitals in the state are at risk of closing due to financial pressure. The bill now moves to the House for a vote. Read More
Mississippi Medicaid Expansion Bills Die in Legislature. The Mississippi Free Press reported on February 2, 2023, that several Medicaid expansion bills died in the Mississippi legislature, including bipartisan legislation calling for a referendum on the issue. Mississippi Governor Tate Reeves reiterated his opposition to Medicaid expansion in his State of the State address. Read More
Montana
Montana House Committee Considers Bill to Increase Reporting Requirements for HEART Initiative. Kaiser Health News reported on February 3, 2023, that the Montana House Health Services Committee is considering a bill that would increase reporting requirements for the Healing and Ending Addiction Through Recovery and Treatment (HEART) initiative. Lawmakers and advocates are both looking for accountability and clarity on how the money is being spent. The HEART initiative has spent $5.2 million since 2022, and the state is waiting for federal approval of the HEART waiver as well as an additional $19 million in federal funding.
Nebraska
Nebraska Nursing Homes Call for Additional Medicaid Funding to Prevent Closures. KLKN reported on February 7, 2023, that the Nebraska Health Care Association is calling for increased Medicaid reimbursement rates for nursing homes and long-term care facilities to avoid further closures. Governor Jim Pillen’s proposed budget for fiscal 2024 allocates $17.5 million of American Rescue Plan Act funding to address staffing shortages in nursing homes but does not increase rates further. Reimbursement rates for nursing homes rose 25 percent in fiscal 2022 and almost 16 percent 2023. In 2022, 11 long-term care facilities closed, mostly in rural communities. Read More
New Hampshire
New Hampshire Provider Groups Urge Lawmakers to Increase Medicaid Reimbursement Rates. New Hampshire Public Radio reported on February 2, 2023, that New Hampshire provider groups are urging lawmakers to pass healthcare legislation that would dedicate $145 million to increase Medicaid reimbursement rates in the next two years. The stakeholders, who made the remarks during hearings on the bill, are seeking funds to address staffing shortages, long-term care facilities, and mental health treatment. Read More
New York
New York Counties Oppose Potential Loss of Enhanced Federal Medicaid Funds. The Post-Star reported on February 3, 2023, that the New York State Association of Counties is opposing a proposal in Governor Kathy Hochul’s proposed budget in which the state would no longer share temporary enhanced federal Medicaid funding with counties. State Assemblywoman Carrie Woerner (D-Round Lake) and Assemblyman Matt Simpson (R-Horicon) have indicated they do not support the proposal. Read More
New York Governor Prioritizes Medicaid Reimbursement Increases, Behavioral Health in Fiscal 2024 Budget. Crain’s New York reported on February 2, 2023, that New York Governor Kathy Hochul proposed a five percent reimbursement rate increase for hospitals, nursing homes, and assisted living providers in her fiscal 2024 budget proposal. Hochul also proposed $88 billion in Medicaid spending ($35 billion from the state and $53 billion from the federal government), and an option for the state to competitively procure managed care contracts for the long-term care program. The proposed budget includes a breakdown of Hochul’s $1 billion plan to address mental health in New York, with $890 million allocated to new units for individuals with mental health conditions, $60 million for comprehensive psychiatric emergency programs, and $18 million for inpatient psychiatric beds. Read More
North Carolina
North Carolina Seeks Waiver Amendment to Extend Medicaid Eligibility to Parents, Caretakers of Children in Foster Care. The Centers for Medicare & Medicaid Services announced on February 7, 2023, that North Carolina submitted an amendment application for its North Carolina Medicaid Reform Demonstration Section 1115 waiver, which seeks to extend Medicaid eligibility to parents and caretaker relatives of children in foster care who are making reasonable efforts to comply with a court-ordered plan of reunification. The state is also proposing expanding eligibility for the Children and Families Specialty Plan to include additional Medicaid-eligible beneficiaries. The federal comment period is open until March 9. Read More
North Carolina Announces Retirement of Medicaid Director Dave Richard. The Associated Press reported on February 2, 2023, that North Carolina Medicaid director Dave Richard will retire at the end of February. Richard, whose official title is deputy secretary for Medicaid at the state Department of Health and Human Services, has held the position for the past eight years. Read More
North Carolina Launches Health System Transformation Collaborative. North Carolina announced on February 2, 2023, the launch of a public-private State Transformation Collaborative (NCSTC), which will focus on strengthening primary care, aligning quality measures, enhancing health equity data, and improving data infrastructure. NCSTC is a collaborative of Duke University’s Margolis Center for Health Policy, North Carolina Department of Health and Human Services Division of Health Benefits, Health Care Payment Learning & Action Network (HCPLAN), and the Centers for Medicare & Medicaid Services. State Transformation Collaboratives have also been established in California, Colorado, and Arkansas through HCPLAN, with the goal of continuing to shift healthcare from fee-for-service to a value-based, person-centered approach through alternative payment models in Medicaid and Medicare. Read More
Oklahoma
Oklahoma to Apply for Medicaid Managed Care Waiver. The Oklahoma Health Care Authority (OHCA) announced on February 3, 2023, it intends to submit a Section 1915 waiver application to implement a comprehensive Medicaid managed care program covering medical, behavioral, pharmacy, and care coordination services. The waiver would cover eligible pregnant women, low-income parents and caretakers, infants, children under age 18, and adults in the expansion population. Public comments will be accepted through March 5, 2023. Read More
Vermont
Vermont Releases Technical Assistance for Medicaid Supportive Housing Program RFP. The Vermont Agency of Human Services released on February 3, 2023, a request for proposals (RFP) for technical assistance in the planning, implementation, and development of a Medicaid Supportive Housing Assistance Program, which will take effect in 2024. Services would include an engagement plan for pre-tenancy supports, tenancy-sustaining supports, and community transition services. Responses are due by March 2. Read More
Washington
Washington Submits Section 1115 Family Planning Waiver Extension Request for Federal Approval. The Centers for Medicare & Medicaid Services announced on January 20, 2023, that Washington applied for an extension of its Section 1115 family planning waiver though June 30, 2028. The waiver program covers 10 months of family planning services for individuals formerly enrolled in Medicaid postpartum coverage and offers family planning services to individuals with household incomes at or below 200 percent of federal poverty. Read More
National
Biden Calls for Extending Insulin Price Cap, Enhanced Exchange Subsidies in State of Union. Fierce Healthcare reported on February 7, 2023, that President Biden called for expanding the $35 monthly cap on insulin costs to everyone (not just Medicare beneficiaries), a permanent extension of enhanced Exchange plan subsidies, and continued funding for COVID-19 vaccines and treatments in the State of the Union address. Biden also emphasized he will not accept cuts to Medicare or Social Security. Read More
Federal Judge Dismisses Lawsuit by Drug Manufacturers Regarding Importation of Pharmaceuticals. STAT reported on February 7, 2023, that U.S. District Court Judge Timothy Kelly dismissed a lawsuit from the Pharmaceutical Research & Manufacturers of America (PhRMA) against the U.S. Department of Health and Human Services (HHS) regarding a rule allowing the importation of prescription drugs from Canada. The judge ruled that the PhRMA failed to demonstrate “concrete risk of harm” to drug manufacturers that could result from HHS allowing states to import drugs. Read More
Medicaid, CHIP Enrollment Increased 28.5 Percent During Pandemic, Study Finds. Health Payer Intelligence reported on February 7, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) increased by 20.2 million lives, or 28.5 percent, to 91.3 million between February 2020 and October 2022, according to an analysis from Kaiser Family Foundation. All states saw enrollment growth. Read More
Implementing Nursing Home Spending Thresholds Alone Will Not Guarantee Adequate Staffing, Study Finds. McKnight’s Long-Term Care News reported on February 6, 2023, that requiring nursing homes to spend a specific amount of revenues on direct care will not alone guarantee that facilities are adequately staffed, according to a Health Affairs study. However, the study found that spending thresholds in conjunction with minimum staffing requirements, as well as adequate federal funding, would help with staffing levels. Read More
Federal Judge Rules Against Disenrollment of Medicaid Members Who Are Eligible for Medicare Savings Program. The Connecticut Mirror reported on February 3, 2023, that a federal judge in Connecticut issued a temporary injunction aimed at blocking the disenrollment of Medicaid members who have become eligible for the Medicare Savings Program (MSP). Despite the continuous enrollment provisions of COVID-19 relief legislation, a November 2020 rule allowed states to disenroll certain individuals, including those eligible for the MSP. As part of the judge’s ruling, federal regulators must inform states not to comply with the November rule. Read More
State Governors Push for Increased Funding for Mental Health Services in Fiscal 2024 Budget Proposals. The Wall Street Journal reported on February 5, 2023, that state governors are pushing for increased funding for mental health services in their fiscal 2024 budget proposals. Key areas include the mental health worker shortage, mental health needs in schools, and a growing demand for emergency services. Read More
House Lawmakers Introduce Bill to Make Telehealth Benefits Permanent, Stand-alone Offering. mHealthIntelligence reported on February 3, 2023, that House lawmakers introduced a bipartisan bill that would make telehealth benefits a permanent, stand-alone offering similar to vision and dental coverage. The bill is sponsored by Representatives Suzan DelBene (D-WA), Tim Walberg (D-MI), Angie Craig (D-MN), Ron Estes (R-KS), Mikie Sherrill (D-NJ), and Rick Allen (R-GA). Read More
Insurers Oppose Exchange Plan Essential Health Benefits. Fierce Healthcare reported on February 3, 2023, that insurers opposed Exchange plan essential health benefits in response to a request for information on the topic by federal regulators. Providers are pushing the Centers for Medicare & Medicaid Services (CMS) to increase insurer oversight. Essential benefits require payers to cover 10 essential services, including inpatient hospital care and prescription drug coverage. Read More
CMS Officials Aim to Establish Universal Quality Measures Across Programs. Fierce Healthcare reported on February 2, 2023, that Centers for Medicare & Medicaid Services (CMS) officials are seeking to establish a “universal foundation” of quality measures across over 20 CMS programs, according to a letter submitted to The New England Journal of Medicine. The universal measures outlined in the letter include prevention and screening rates, immunizations, control of chronic conditions, and health equity. Read More
Combined Medicaid, Medicare Spending on Dual Eligibles was $456 Billion in 2020, MACPAC, MedPAC Report Finds. The Medicaid and CHIP Payment and Access Commission (MACPAC) reported on February 2, 2023, that combined Medicare-Medicaid spending on dual eligibles was $456.2 billion in 2020. The information appeared in 2023 Data Book: Beneficiaries Dually Eligible for Medicare and Medicaid jointly produced annually by MACPAC and the Medicare Payment Advisory Commission (MedPAC). The data book also includes information on dual eligible demographics, utilization, and trends. Read More
Insurers Oppose Limits on Non-standardized Exchange Plan Options. Fierce Healthcare reported on February 1, 2023, that insurers strongly oppose proposed federal limits on the number of non-standardized Exchange plan options allowed in 2024, according to comments submitted to the Centers for Medicare & Medicaid Services. The proposal would allow two non-standardized Exchange plan options per network type and metal tier in a service area. The final rule is expected to be released in the spring. Read More
MACPAC Signals Support of Proposed Substance Use Disorder, Medicaid Enrollment Rules. Medicaid and CHIP Payment and Access Commission (MACPAC) indicated on January 2023, its support of a proposed federal rule aimed at improving care coordination for substance use disorder (SUD) patients. However, MACPAC urged in comments submitted to the U.S. Department of Health and Human Services that implementation guidance is needed. Separately, MACPAC also submitted comments in support of rules aimed at helping beneficiaries transition between Medicaid and Exchange coverage but added that more needs to be done. Read More
Industry News
CVS Health to Acquire Oak Street Health. Modern Healthcare reported on February 8, 2023, that CVS Health will acquire Illinois-based primary care provider Oak Street Health for $10.6 billion in cash and assumed debt. Oak Street employs about 600 providers in 169 locations across 21 states. The deal is set to close this year. Read More
Carlyle Group Looks to Acquire of Cotiviti from Veritas Capital. Axios reported on February 7, 2023, that Carlyle Group is in talks to acquire healthcare software company Cotiviti in a $15 billion deal, including debt, from Veritas Capital. The transaction would involve a $5.5 billion loan. Read More
Lifepoint Health Acquires Majority Stake in Springstone’s Operating Company. Lifepoint Health announced on February 7, 2023, the acquisition of a majority stake in Springstone’s operating company, including 18 behavioral health hospitals and 35 outpatient clinics in nine states. Medical Properties Trust will continue to own a minority stake in Springstone’s operating company and a majority of Springstone’s real estate locations. The acquisition extends Lifepoint’s behavioral health network to 62 community hospital campuses, more than 50 rehabilitation and behavioral health hospitals, and more than 200 other care sites. Read More
AmeriHealth Caritas Appoints Marla Purvis as GA Market President. AmeriHealth Caritas announced on February 1, 2023, the appointment of Marla Purvis as Georgia market president. Previously, Purvis served as Florida market president and corporate vice president of Medicare Operations for Evolent Health. Georgia is expected to release a request for proposals for its Medicaid managed care program in early 2023. Read More
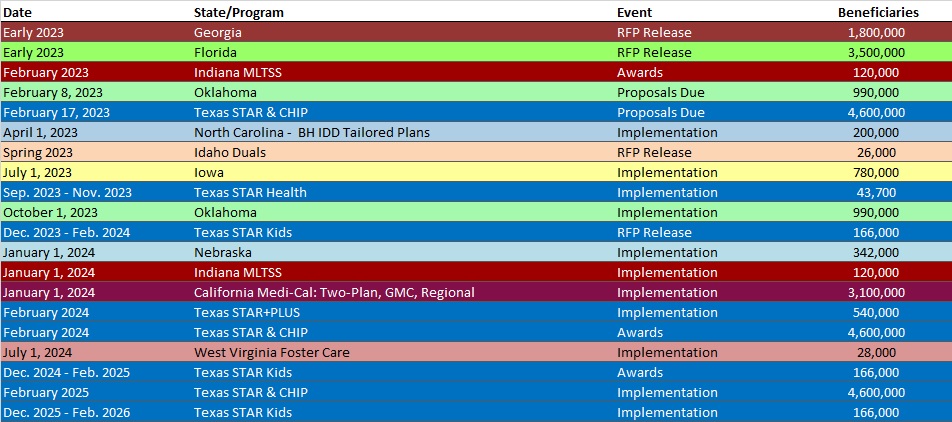
RFP Calendar
Company Announcements
Highmark to Use MCG Care Guidelines and Solutions to Optimize Care Management
MCG Health, part of the Hearst Health network, announces that Highmark Inc. will transition to MCG’s evidence-based solutions to guide care management decisions for its plan membership of over 6 million. Read More.
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Louisiana Medicaid Managed Care Enrollment is Up 5.8%, 2022 Data
- Michigan Medicaid Managed Care Enrollment is Up 3.7%, Oct-22 Data
- Michigan Dual Demo Enrollment is Up 8.3%, Oct-22 Data
- Minnesota Medicaid Managed Care Enrollment is Up 7.1%, Nov-22 Data
- Missouri Medicaid Managed Care Enrollment is Up 26.7%, Nov-22 Data
- Nevada Medicaid Managed Care Enrollment is Up 4.6%, Nov-22 Data
- New Jersey Medicaid Managed Care Enrollment is Up 6.3%, Nov-22 Data
- New Mexico Medicaid Managed Care Enrollment is Up 2%, Oct-22 Data
- North Dakota Medicaid Expansion Enrollment is Up 10.2%, 2022 Data
- Oregon Medicaid Managed Care Enrollment is Up 7.3%, 2022 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 6%, Nov-22 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 2.6%, Nov-22 Data
- Washington SNP Membership at 98,973, Nov-22 Data
- West Virginia SNP Membership at 28,802, Nov-22 Data
- Wyoming SNP Membership at 803, Nov-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alaska MMIS Support Services RFP, Feb-23
- California Preadmission Screening and Resident Review Level II Evaluations IFB, Feb-23
- Colorado Medicare D-SNP Contract, 2023
- Iowa Medicaid Program Integrity Professional Services RFP, Feb-23
- Vermont Optical Benefits to Medicaid Beneficiaries RFP, Feb-23
- Vermont Technical Assistance for Medicaid Supportive Housing Assistance Program RFP, Feb-23
Medicaid Program Reports, Data, and Updates:
- Colorado Prescription Drug Affordability Board Meeting Materials, 2021-23
- Delaware Governor’s Proposed Budget, FY 2024
- Florida Governor’s Proposed Budget, FY 2024
- Georgia Governor’s Proposed Budget, FY 2024
- Idaho Governor’s Proposed Budget, FY 2024
- Maine Prescription Drug Affordability Board Meeting Materials, 2022
- Maryland Prescription Drug Affordability Board Meeting Materials, 2021-23
- Nebraska Governor’s Budget Recommendations, 2023-25
- Ohio Governor’s Budget Recommendations, FY 2024-25
- Ohio Prescription Drug Transparency and Affordability Council Report, 2020
- Texas HHS Presentation to Senate Finance Committee on Medicaid Budget, Feb-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
