This week our In Focus reviews Minnesota Department of Human Services (DHS) requests for proposals (RFPs) for two of the state’s Medicaid managed care programs: Minnesota Senior Health Options/Minnesota Senior Care Plus and Special Needs BasicCare/Integrated Special Needs BasicCare. Both RFPs, released on October 25, 2021, cover health care services in all 87 Minnesota counties.
Minnesota Senior Health Options (MSHO), Minnesota Senior Care Plus (MSC+)
MSHO and MSC+ cover health care and long-term services and supports to individuals ages 65 and older. MSHO is the state’s dual demonstration program, covering individuals who are eligible for Medical Assistance (MA), the state’s Medicaid program, and both Medicare Parts A and B. MSHO is one of the longest-standing fully integrated dual eligible, special needs plan (FIDE-SNP) programs operating through a Medicare Advantage platform. MSC+ provides MA coverage for individuals who may also have Medicare coverage. It is mandatory that individuals eligible for MA age 65 or older enroll in Medicaid managed care in Minnesota, either MSC+ or MSHO, unless an exception applies. Over 90 percent of older adults eligible for MA are enrolled in MSHO or MSC+.
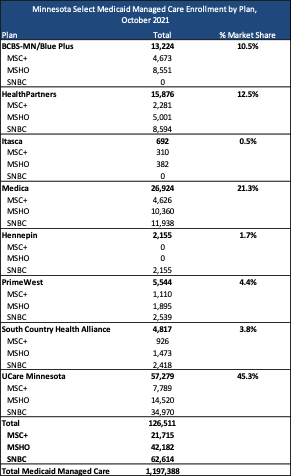
Current incumbents are Blue Plus, HealthPartners, Itasca Medical Care, Medica, PrimeWest Health, South Country Health Alliance, and UCare.
DHS aims to contract with at least two MCOs in the 13 counites identified as metro or large metro counties. In the remaining counties, the state will determine the number of MCOs. However, DHS intends to contract with more than one MCO in a county unless the sole bidder is already offered in that county, is the highest scoring for the county, and the only plan currently serving the county meeting the minimum requirements.
Medicaid managed care organizations that participate in MSHO in a county must also participate in MSC+ in the same county. MCOs cannot offer MSC+ as a standalone product in a county. Bidders who already operate MSHO and MSC+ in a county will be selected to participate if they meet the minimum requirements of the RFP. Additional MCOs will be selected based on scoring.
In 2019, DHS cancelled a previous RFP for MSHO and MSC+, in addition to MA Families and Children and MinnesotaCare programs, due to a court decision that made the contracting timeline impossible without disruptions to members.
Special Needs BasicCare (SNBC) and Integrated Special Needs BasicCare (Integrated SNBC)
SNBC and Integrated SNBC cover health care for individuals with disabilities age 18 to 64 who are enrolled in MA. The program is a voluntary, opt-out program. In order to be eligible for Integrated SNBC, an individual must also be eligible for Medicare Parts A and B. Integrated SNBC plans operates through a dual eligible special needs plan (D-SNP) Medicare Advantage platform. Most SNBC enrollees have five or more chronic conditions, with 70 percent of enrollees having a behavioral health diagnosis.
Current incumbents are Hennepin Health, HealthPartners, Medica, PrimeWest Health, South Country Health Alliance, and UCare.
Medicaid managed care organizations who participate in the Integrated SNBC program, must also participate in SNBC in the same county. MCOs can, however, provide SNBC as a standalone MA product in a county. Bidders who already operate an SNBC in a county will be selected to participate if they meet the minimum requirements of this RFP. Additional MCOs will be selected based on scoring.
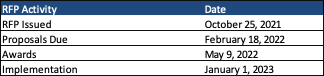
Timeline
Proposals for both RFPs are due February 18, 2022, with awards anticipated May 9, 2022. Contracts are expected to run from January 1, 2023, through December 31, 2023, with up to five optional years.
Evaluation
Proposals will be evaluated in three phases:
- Phase I Required Statements Review
- Phase II Evaluation of Proposal Requirements and Readiness Review
- Phase III Selection of the Successful Responder(s) and Readiness Review
The first phase, consisting of required statements, will be evaluated on a pass/fail basis. During the second phase, proposals will be scored on both a pass/fail basis and points basis.
Proposals will need to pass on the Service Delivery Plan including Executive Summary and Description of the Applicant Organization, but not including Section E, Care Coordination Model; Readiness Review; Financial Solvency; and Provider Network Adequacy Review. If a proposal fails on either component, it will not move on for consideration in the third phase. Each proposal can then earn up to 105 points based on the following criteria:
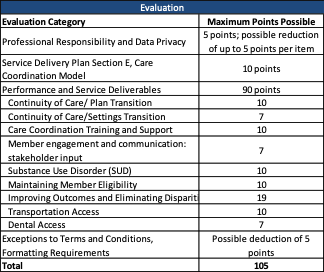
Proposals must receive a total score of 50 to pass.
Current Market
Among the MSC+, MSHO, and SNBC programs, there were 126,500 enrollees as of October 2021. UCare held the highest market share by enrollment for the three programs at over 45 percent. Total Medicaid managed care enrollment for all MA and MinnesotaCare was nearly 1.2 million.