This week’s In Focus highlights a recent HMA publication examining the drivers and barriers to Medicare Advantage plan adoption of newly available supplemental benefits intended to address unmet health and social needs. Unlike Traditional Medicare, Medicare Advantage plans, which provide coverage for 40 percent of all Medicare beneficiaries, may offer enrollees supplemental benefits which are not covered by the Medicare program. Until recently, the Medicare program has required that supplemental benefits be limited to those that are medical in nature. However, in recent years, Congress and CMS —through four different legislative and regulatory authorities — granted new flexibilities for Medicare Advantage plans to offer non-medical benefits that address social needs. Medicare Advantage plans may also now tailor supplemental benefits and make them available only to certain subpopulations based on chronic disease or health status.
Many in the policy community believe that these new flexible benefits will enable Medicare Advantage plans to better manage both the healthcare needs and social needs of medically complex and frail beneficiaries. However, only 18 percent of Medicare Advantage plans — accounting for less than 20 percent of the Medicare Advantage enrollment — offered these new flexible benefits in 2020, raising questions regarding their perceived value by plans and beneficiaries. In addition, there is limited data to-date that demonstrates that the benefits offered under current requirements meet the specific needs of the individuals served or improve health outcomes.
HMA, with the support of a grant from Arnold Ventures, requested and conducted interviews with beneficiary advocates, Medicare Advantage plans, and supplemental benefit service providers to better understand the factors contributing to a Medicare Advantage plan’s determination to offer (or not offer) newly available supplemental benefits as well as opportunities and challenges with the adoption and implementation of the various flexibilities. HMA also sought to understand the extent to which enrollees used the available flexible benefits, as well as their effectiveness as a tool to contain costs, improve outcomes, and address unmet health and social needs.
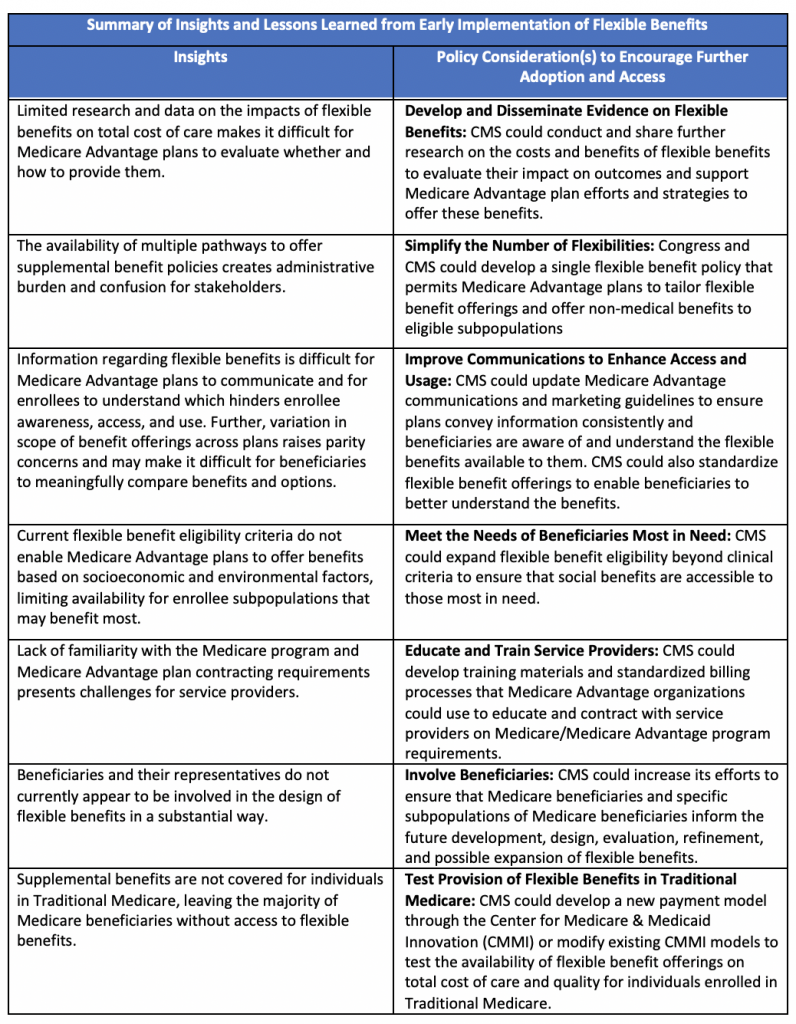
All Medicare Advantage organizations interviewed indicated that 2020, the first year in which all four benefit flexibilities were available, served as a period for learning, experimentation and evidence gathering; and expressed a need for more data on which flexible benefits would be most effective in improving health outcomes and reducing costs. The beneficiary advocacy organization interviewed was generally supportive of the new policies permitting Medicare Advantage plans to offer non-medical supplemental benefits but raised concerns regarding how the availability of those benefits are communicated and whether beneficiaries have meaningful access to them when eligible. All stakeholders interviewed indicated that additional time and experience is needed to understand whether the new benefit flexibilities enable plans to better serve individuals with complex health and social needs and urged CMS and Congress to promote further availability of these flexible benefits. These findings are summarized in the table below along with corresponding considerations for future flexible benefit policies that may further facilitate plan adoption, beneficiary access, effectiveness, and relevance of the benefits.
Detailed insights and policy considerations are included in the brief which can be found here. For more information, please contact HMA Senior Consultant Narda Ipakchi.