This week, our In Focus section recognizes International Overdose Awareness Day (IOAD), August 31, by highlighting how states can use opioid abatement funds to mitigate the persistent overdose crisis in communities across the country.
In honor of IOAD, the August 2024 edition of HMA’s Podcast, Vital Viewpoints, features Erin Russell, a Principal at Health Management Associates (HMA), who discusses the importance of emphasizing harm reduction as a compassionate approach to drug policy. Meanwhile, this article addresses current gaps, opportunities, and strategies for applying opioid abatement funds to make further progress in addressing overdoses and the crisis.
Context for Opioid Abatement
Overdoses have claimed more than one million lives since the late 1990s, with more than 100,000 deaths occurring annually. Exacerbating the overdose epidemic and the racial and ethnic disparities in fatal overdoses are persistent inequities in access to evidence-based treatment, which extend to biases based on physical and/or mental ability, sexual orientation and gender identity, geographic location, and socioeconomic and housing status.
In 2021, nationwide settlements were awarded to resolve all opioid litigation that states and local subdivisions brought against pharmaceutical distributors and manufacturers, with subsequent agreements reached in 2022 against pharmacy chains and additional manufacturers. These historic opioid settlement agreements, which total more than $56 billion, will provide funds to state and local governments to address the crisis in their communities.
Policy changes and investments to address this epidemic remain critical. These approaches require careful consideration of the data and evidence-based strategies that are responsive to the crisis. In 2024, the US Department of Health and Human Services issued a rule that updates the regulations regarding the governance of opioid treatment programs; for example, removing barriers to the treatment of substance use disorder (SUD) and expanding access to care. The State Opioid Response and Tribal Opioid Response grant programs are another significant tool to improve prevention, expand treatment, and deliver free, lifesaving medications. Medicaid, including Medicaid managed care plans, also can be instrumental in supporting harm reduction strategies and enhancing access to addiction treatment and recovery support.
Opioid abatement funds offer states the opportunity to apply innovative solutions in response to the overdose epidemic. Despite their potential, however, HMA experts have identified significant opportunities across many states to effectively use available opioid abatement funds.
Opioid Abatement Funds and planning for Community Needs
Strategic planning processes allow state and community leaders to understand the needs of residents, examine current services offered and their existing strengths, and explore barriers to accessing care to make informed decisions about how the settlement funding can be used successfully. A strategic plan can assist in tracking progress and establishing a clear vision for an organization’s future and can yield a living document that guides the most advantageous use of the funds. HMA experts supported a strategic planning process for Carrabus County, NC, that identified strategies for designing, implementing, and evaluating tailored solutions for disbursing opioid abatement funds. The following are examples of approaches that are included in strategic plans for opioid abatement.
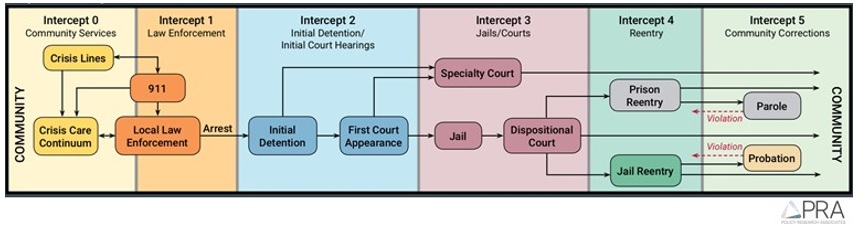
Sequential intercept model (SIM). SIM, one of the models used to support communities in building a stronger system of care, helps identify intervention opportunities with the highest potential for success based on a community’s strengths and needs. SIM maps out the stages of intervention to pinpoint gaps and opportunities, ensuring funding is used to address the most critical areas for improving community care systems, including those integrated within Medicaid managed care delivery systems (see Figure 1).
Figure 1: Sequential Intercept Model
Low-barrier/low-threshold recovery supports and treatment. The expansion of low-barrier/low-threshold recovery supports and treatment, including access to medications for opioid use disorder, is essential to reducing overdose deaths. States, local jurisdictions, and individual providers can redesign their treatment delivery systems to incorporate person-centered, low-barrier treatment access, including flexible scheduling and walk-in visits, same-day admission and medication initiation, and revision of clinic policies and procedures to eradicate practices that produce high barriers to treatment.
Though expanding low-barrier care in traditional treatment settings is an essential element of the response, implementation of nontraditional delivery modalities is another important target for using opioid abatement funds. Examples include:
- Emergency medical service (EMS)-initiated buprenorphine
- Medication units in unconventional locations (e.g., housing units)
- Mobile medication units and delivery of street/shelter medicine in which SUD treatment and services are brought to disenfranchised and marginalized communities.
Finally, the availability of opioid abatement funds can introduce opportunities for local governments to partner with community members, including people with both past and current lived experience, to design, implement, and disseminate culturally responsive and tailored SUD treatment and recovery support services, including services to address health-related social needs to mitigate barriers to treatment entry and engagement.
Continuous quality improvement (CQI) plans. Locales that receive opioid abatement funds have the opportunity to develop strategies to create transformational systemic change. Each entity should have an intentional CQI plan in place. Ensuring the presence of strong CQI processes can streamline and improve services, connect data to practice, and ensure interventions are progressively more effective.
Connect with Us
The upcoming HMA event, Unlocking Solutions in Medicaid, Medicare, and Marketplace, will offer more opportunities to engage with leaders across multiple sectors and industries advancing innovations in the design of mental health and SUD systems, value-based purchasing, and care strategies. Notably, state Medicaid and behavioral health directors, insurance commissioners, health plan executives, and community leaders, among others, will share insights into major initiatives under way in their states to manage ongoing crises in mental health and SUDs.
HMA has a strong, diverse bench to help communities maximize opioid abatement funds and build a stronger system of care. We provide technical assistance in large-scale initiative implementation, convening stakeholder groups, designing CQI strategies, developing planning documents, and facilitating strategic discussions. For more information about HMA’s work, contact behavioral health experts Anika Alvanzo, Rachel Johnson-Yates, and Jessica Perillo.