This week, our In Focus section reviews the notice of funding opportunity (NOFO) for the Transforming Maternal Health (TMaH) Model, which the Centers for Medicare & Medicaid Services (CMS) Center for Medicaid and Medicare Innovation (the Innovation Center) announced on December 15, 2023. States interested in participating in this model must submit an application to CMS during the competitive application process.
As described in a December 2023 In Focus, pregnancy-related deaths have more than doubled since 1987 to 17.6 deaths per 100,000 live births, with health disparities only worsening outcomes for different racial and ethnic groups. For example, the pregnancy-related mortality rates for Black and Native American and Alaska Native people are approximately two to three times higher than the rate for White people. In recent years, 38 states have extended postpartum coverage, and 11 states now offer doula coverage for Medicaid enrollees. This initiative accelerates the focus on maternal outcomes and, with Medicaid paying for nearly 43 percent of births, has the potential to affect health across generations.
This model is designed exclusively to improve maternal healthcare for people enrolled in Medicaid and the Children’s Health Insurance Program (CHIP). The TMaH model takes a whole-person approach to pregnancy, childbirth, and postpartum care, addressing the physical, mental health, and social needs people experience during pregnancy.
Model Overview
Up to 15 participating state Medicaid agencies (SMAs) will receive as much as $17 million over the 10-year period to develop a value-based alternative payment model for maternity care services, with the intention of improving quality and health outcomes and promoting the long-term sustainability of services. TMaH will focus on three pillars:
- Access to care, infrastructure, and workforce capacity
- Quality improvement and safety
- Whole-person care delivery
The TMaH model is designed to support birthing persons along their care journey, expanding continuity, and improving outcomes.
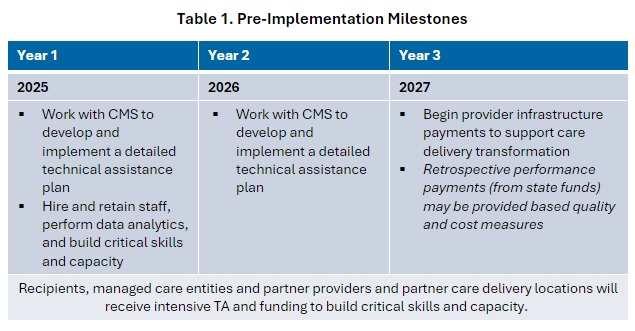
During the model’s first three years, states will receive targeted technical assistance to achieve pre-implementation milestones. The table below highlights the key activities in the pre-implementation phase.
Following pre-implementation, participants will enter a seven-year implementation period during which the SMAs will implement the program with partners, such as managed care organizations (MCOs), perinatal quality collaboratives, hospitals, birth centers, health centers and rural health clinics, maternity care providers, and community-based organizations.
In year four, states will offer partnering providers and care delivery sites upside-only performance payments from state funds (no cooperative funds may be used). In year five, states will transition partner provider and partner care delivery locations to a new value-based payment model. CMS will lead the development of the value-based model, and it will be finalized during the pre-implementation period.
The model also requires a health equity plan, which has been a consistent requirement across models from the Innovation Center. Awardees must develop a plan that addresses disparities among underserved populations, such as racial and ethnic groups and people living in rural areas, who are at higher risk for poor maternal outcomes.
State Medicaid Agency Requirements
For states considering TMaH, the NOFO outlines the requirements for participating SMAs, which include:
- States must include CHIP if pregnant people receive services through CHIP
- States that have managed care plans must contract with at least MCO for implementation
- Collaborate with partner providers (e.g., OBs, midwives, doulas), care delivery location (e.g., hospitals, birth centers, federally qualified health centers), and partner organizations
- Collaborate in the process to create cost and quality benchmarks with CMS
- Be actively involved in technical assistance activities, including attending regularly scheduled calls, providing input and working on portions of documents as appropriate
- Execute the data-sharing agreements necessary to support the exchange of data and information related to the TA activities and completion of milestones
- Provide CMS and contractors the necessary information and data to support the development of documents to help reach milestones
- States must demonstrate their ability to meet these requirements as part of the NOFO process, and CMS will evaluate their responses as part of the selection process
TMaH Opportunities and Considerations
The model offers states resources and technical assistance to develop value-based alternative payment models to support whole-person pregnancy, birth, and postpartum care and improved outcomes. Many SMAs already are working on programs to innovate care and payment, and the TMaH is an opportunity to expand and accelerate those programs.
The model offers an opportunity for states that have yet to expand postpartum coverage or added doula benefits to adopt these policies with the funding and technical assistance they may need to support their efforts.
SMAs interested in this opportunity should evaluate their application readiness and pre-plan for the application.
What’s Next?
States interested in TMaH should submit a letter of intent by August 8, 2024. Applications are due by September 20, 2024, and the model is expected to start January 2025.
The Health Management Associates team will continue to evaluate the TMaH model as more information becomes available. For more information, contact our featured experts below.

